Introduction
Patients discharged from inpatient psychiatric services are at elevated risk for an array of adverse outcomes, such as suicide and other causes of premature mortality, nonfatal self-harm and interpersonal violence perpetration and victimization [Reference Steadman, Mulvey, Monahan, Robbins, Appelbaum and Grisso1–Reference Musgrove, Carr, Kapur, Chew-Graham, Mughal and Ashcroft6]. Previous studies have predominantly examined risks for a single adverse outcome, with some recently published papers reporting risks for multiple adverse outcomes in the same study cohort [Reference Walter, Carr, Mok, Antonsen, Pedersen and Appleby5]. Physical harm inflicted on oneself and on other people occurs much more frequently among individuals who have received inpatient psychiatric treatment than in those without such a history [Reference Musgrove, Carr, Kapur, Chew-Graham, Mughal and Ashcroft6–Reference Mellesdal, Kroken, Lutro, Wentzel-Larsen, Kjelby and Oedegaard10]. However, no study to date has estimated absolute risks for the two outcomes stratified by psychiatric diagnosis in a single cohort of discharged persons, enabling the identification of individuals at especially heightened risk. Self-harm is a major risk factor for suicide [11], and therefore understanding self-harm risks by gender and by diagnostic group among patients discharged from inpatient psychiatric care offers opportunities for tailoring of timely preventive measures. Interpersonal violence causes physical and emotional harm to others and oneself and is also associated with increased risk of dying from unnatural causes [Reference Steeg, Webb, Mok, Pedersen, Antonsen and Kapur12]. Identifying individuals at higher risk of perpetrating interpersonal violence following discharge from inpatient psychiatric provides further possibilities for preventive follow-up in a patient group likely to be in ongoing contact with mental health services, general healthcare and criminal justice agencies.
In this register-based study, we aimed to compare absolute risks for fatal and nonfatal self-harm and interpersonal violence in a cohort of Danish persons discharged from their first inpatient psychiatric care episode, and to stratify these risks by gender across the full spectrum of psychiatric diagnostic categories. We estimated absolute risks for these adverse outcomes within 1 year and at 10 years post-discharge. This work expands on previously conducted studies in the same study cohort [Reference Walter, Carr, Mok, Astrup, Antonsen and Pedersen4, Reference Walter, Carr, Mok, Antonsen, Pedersen and Appleby5]. We hypothesized that risks for self-harm and interpersonal violence perpetration would be higher among discharged patients diagnosed with substance misuse disorders compared to individuals in other diagnostic groups. This is the first study to report on gender-specific absolute risks of the two adverse outcomes across the spectrum of diagnosed mental illnesses, and also the first to report the absolute risk for either outcome occurring post-discharge.
Methods
Study cohort
The cohort was delineated from the Danish Civil Registration System [Reference Pedersen13], which was established in 1968 and records demographics and continuously updated vital status of all Danish residents. The unique identification number assigned to each resident enables accurate linkage with other Danish national registers. Cohort members were all persons born in Denmark during 1967–2000, alive and residing in the country at their 15th birthdays, and with two Danish-born parents. The Data Protection Agency approved the study, with data access agreed by the Health Data Authority and Statistics Denmark. Because the study was conducted using registry data, according to Danish legislation informed consent from cohort members was not required.
Exposures
Information on first discharge from inpatient psychiatric services was obtained from the Psychiatric Central Research Register [Reference Mors, Perto and Mortensen14]. This source was computerized in 1969 and contains data on all admissions to inpatient psychiatric facilities. The following diagnostic categories were examined: substance misuse disorders; schizophrenia and related disorders; mood disorders; anxiety and somatoform disorders; personality disorders; early onset behavioral and emotional disorders; comorbid substance misuse disorder with each of the other diagnostic categories examined; all diagnostic categories combined. The ICD codes used to classify these categories are shown in eTable 1 in the Supplementary Material [Reference Pedersen, Mors, Bertelsen, Waltoft, Agerbo and McGrath15]. Individuals with more than one psychiatric disorder were included in the analysis for each specific disorder, and thus the categories were not mutually exclusive. We also investigated number of diagnostic categories at first discharge (1, 2, 3, or more). Any psychiatric diagnoses not under the six aforementioned categories were grouped together and counted as an additional category.
Outcomes
Self-harm
For consistency with the “Interpersonal violence” outcome (which included homicides), deaths by suicide and nonfatal self-harm episodes were both included. Hospital-presenting self-harm episodes were ascertained using a previously developed algorithm [Reference Nordentoft, Mortensen and Pedersen16], with at least one of the following criteria met according to information recorded in either the National Patient Register [Reference Lynge, Sandegaard and Rebolj17] or the Psychiatric Central Research Register [Reference Mors, Perto and Mortensen14]: (a) Reason for contact code = 4 (National Patient Register); (b) Any psychiatric diagnosis (ICD-10 Chapter F) and a comorbid diagnosis of poisoning with medication and biological compounds (ICD-10 codes T36–T50) or nonmedical compounds, excluding alcohol and poisoning from food (ICD-10 codes T52–T60); (c) Any psychiatric disorder (ICD-10 Chapter F) and comorbid diagnosis reflecting lesions on forearm, wrist or hand (ICD-10 codes S51, S55; S59, S61, S65, or S69); (d) Any hospital contact due to poisoning with weak or strong analgesics, hypnotics, sedatives psychoactive drugs, anti-epileptics and anti-Parkinson drugs or carbon monoxide (ICD-10 codes T39, T42, T43, and T58); (e) Intentional self-harm: ICD-10 X60–X84 (recorded as a primary or secondary diagnosis in either Register). Persons who died by suicide were identified from the Register of Causes of Death [Reference Juel and Helweg-Larsen18], classified as ICD-8 E950–E959 or ICD-10 X60–X84, Y87.0.
Interpersonal violence
Cases were identified from the National Crime Register [Reference Jensen, Greve, Høyer and Spencer19] and included convictions for homicide, assault, robbery, aggravated burglary or arson, possessing a weapon in a public place, threats of violence, extortion, human trafficking, abduction, kidnapping, rioting and serious public order offenses, terrorism, and sexual offenses. We considered the first violent crime that was committed after 15th birthday—the age when adult criminal responsibility commences in Denmark.
Study design and analyses
We delineated a matched cohort study that consisted of 62,922 persons aged 15 years and older who had been discharged from inpatient psychiatric care for the first time. Individuals who had been discharged before their 15th birthdays, and those admitted to psychiatric emergency rooms without transfer to an inpatient ward, were excluded. From competing risk survival analyses, gender-specific cumulative incidence percentages (absolute risks) for each adverse outcome were calculated for each diagnostic category separately, within 1 year and at 10 years after the index discharge. For the investigation of risks of adverse outcomes by number of diagnostic categories at first discharge, cumulative incidence plots were generated using Epanechnikov kernel-weighted local polynomial smoothing method to mask step changes associated with small event counts, in accordance with Danish data protection law. Each of the 62,922 discharged patients was matched on date of birth (±1 day) and gender with 25 comparators (n = 1,573,050) who were alive, residing in Denmark, and had not been admitted to inpatient psychiatric services on or before the date of first discharge for the person to whom each comparator was matched (henceforth referred to as the “index date”). The discharged cohort and the matched comparators were followed up from the index date until the outcome of interest, death, emigration from Denmark, or December 31, 2015, whichever came first. Analyses were conducted using Stata v15.1.
Results
Characteristics of the study cohort
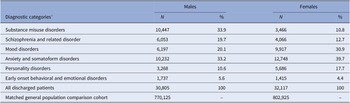
Of the 62,922 individuals aged 15 or over who had been discharged from inpatient psychiatric services for the first time, 51.0% were females. Males were most likely to be diagnosed with substance misuse disorders (Table 1; 33.9% of male patients) and anxiety and somatoform disorders (33.2%), with the most common diagnostic categories for females being anxiety disorders (39.7% of female patients) and mood disorders (30.9%). A diagnosis of an early onset behavioral and emotional disorder at first discharge was relatively rare in this cohort, with 5.6% of males and 4.4% of females classified in this diagnostic group.
Table 1. Total numbers of discharged patients by gender and psychiatric diagnostic category.

a Categories are not mutually exclusive.
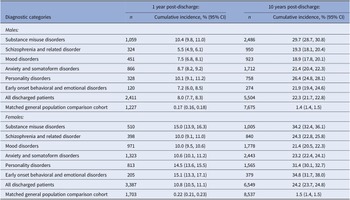
Self-harm risk
Table 2 shows gender-specific cumulative incidence for self-harm at 1 year and 10 years after first discharge from inpatient psychiatric services. Overall, absolute risk of self-harm for males was 8.0% (95% CI 7.7, 8.3%) within 1 year and 22.3% (21.7, 22.8%) within 10 years. Risks were highest among those diagnosed with substance misuse disorders: at 10.4% (9.8, 11.0%) within 1 year, rising to 29.7% (28.7, 30.8%) within 10 years post-discharge. Risks were also particularly high among males diagnosed with a personality disorder: at 10.1% (9.1, 11.2%) within 1 year and 26.4% (24.8, 28.1%) within 10 years post-discharge. Self-harm risk among females was 10.8% (10.5, 11.1%) by 1 year post-discharge and 24.2% (23.7, 24.8%) within 10 years. Females with a diagnosis of early onset behavioral and emotional disorders, substance misuse disorders, and personality disorders at first discharge from inpatient psychiatric care had the highest self-harm risks. Around one in seven of these patients at 1 year, and a third at 10 years, will have had at least one secondary care treated self-harm episode or died by suicide.
Table 2. Absolute risk of self-harm within 1 year and at 10 years after first discharge.

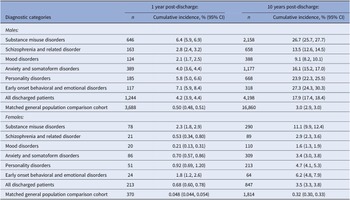
Interpersonal violence risk
The absolute risk of perpetrating interpersonal violence among males was 4.2% (3.9, 4.4%) within a year of being discharged and around one in six (17.9%; 17.4, 18.4%) at 10 years post-discharge (Table 3). In addition to substance misuse disorders, discharged males with early onset behavioral and emotional disorders also had particularly elevated absolute risks; around a quarter of males in each of these diagnostic groups will have engaged in interpersonal violence at 10 years after first discharge from inpatient psychiatric services. On the contrary, absolute risk was relatively low for males diagnosed with mood disorders (9.1%; 8.2, 10.1%) and schizophrenia or related disorders (13.5%; 12.6, 14.5%) within 10 years of discharge.
Table 3. Absolute risk of interpersonal violence perpetration within 1 year and at 10 years after first discharge.

Whereas absolute risks of self-harm were slightly higher for females versus males, absolute risks of interpersonal violence were much lower among females: 0.68% (0.60, 0.78%) within a year and 3.5% (3.3, 3.8%) at 10 years post-discharge (Table 3). Females diagnosed with substance misuse disorders had the highest risk of interpersonal violence: 11.1% (9.9, 12.4%) at 10 years post-discharge, followed by those diagnosed with early onset behavioral and emotional disorders: 6.2% (4.8, 7.9%) at 10 years. As with males, interpersonal violence risk among women diagnosed with mood disorders (1.6%; 1.3, 1.9%) and schizophrenia or related disorders (2.9%; 2.3, 3.6%) was relatively low at 10 years post-discharge.
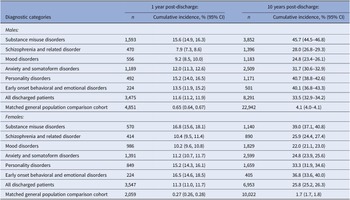
Combined risk of either adverse outcome occurring
In Table 4, cumulative incidence values for either of the two adverse outcomes occurring at 1 year and 10 years post-discharge are presented. A third of males and a quarter of females will have at least one nonfatal or fatal self-harm episode or will have engaged in interpersonal violence within 10 years of their first discharge from inpatient psychiatric care. Risks of one or both adverse outcomes occurring within 10 years after discharge were particularly high among patients diagnosed with substance misuse disorders (45.7% males and 39.0% females), early onset behavioral and emotional disorders (40.1% males and 36.8% females), or personality disorders (40.7% males and 33.3% females).
Table 4. Absolute risk of either adverse outcome (self-harm or interpersonal violence) within 1 year and at 10 years after first discharge.

Risks associated with substance misuse disorder comorbidity
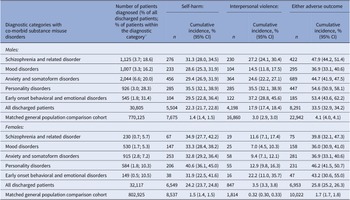
Table 5 shows the cumulative incidence values for self-harm, interpersonal violence, and for either of these two adverse outcomes at 10 years post-discharge associated with a substance misuse disorder diagnosis in conjunction with one of the other diagnostic categories. Because of the relatively small number of these patients with the adverse outcomes examined at 1 year post-discharge, cumulative incidence values at this follow-up are not reported. Around 3 in 10 males and 1 in 10 females with early onset behavioral and emotional disorders or personality disorders also had a diagnosis of substance misuse disorders. These comorbid diagnostic categories were associated with particularly high absolute risks for the two adverse outcomes investigated. Around half of males and females with a diagnosis of substance misuse in conjunction with personality disorders or early onset behavioral and emotional disorders will self-harm or engage in interpersonal violence within 10 years post-discharge.
Table 5. Absolute risk of self-harm, interpersonal violence, and either of the two adverse outcomes, within 10 years after first discharge for patients with co-morbid substance misuse disorders.

a “Percentage of patients within the diagnostic category” is, for instance, the percentage of all male patients in the schizophrenia and related disorder category who were also diagnosed with a substance misuse disorder at first discharge.
Risks associated with number of diagnostic categories at first discharge
Three-quarters of males and females had a psychiatric diagnosis in only one diagnostic category at first discharge (eTable 2 in the Supplementary Material). Figure 1 shows the cumulative incidence for self-harm, interpersonal violence perpetration, and for either adverse outcomes, in the 10 years post-discharge by number of diagnostic categories. The numbers of patients with an adverse outcome at 1 and 10 years are presented in eTable 3 in the Supplementary Material. Risks for all outcomes increased with the number of diagnostic categories.

Figure 1. Absolute risks of self-harm, interpersonal violence perpetration, and either adverse outcome, by number of diagnostic categories and gender. Kernel-weighted local polynomial smoothing applied.
Discussion
Main findings
This national cohort study yielded absolute risk estimates for self-harm and interpersonal violence perpetration among individuals discharged from their first inpatient treatment episode according to gender and psychiatric diagnostic categories. Among males, within a year after first discharge the risk of self-harming was highest among those with substance misuse disorders, whereas for interpersonal violence, individuals diagnosed with early onset behavioral and emotional disorders had the highest absolute risk. The same pattern was observed 10 years post-discharge. For females, absolute risks for self-harm at 1 year and at 10 years were highest among those diagnosed with early onset behavioral and emotional disorders as well as those with substance misuse disorders. Interpersonal violence was most common among those with substance misuse disorders. In both genders, the absolute risks of either internalized or externalized violence within 10 years of first discharge among former inpatients were markedly raised in the riskiest diagnostic categories—substance misuse disorders, personality disorders, and early onset behavioral and emotional disorders. Substance misuse that was comorbid at first discharge with either of these other two high-risk diagnostic categories was the group with the greatest absolute risks. Risk for each examined outcomes also increased with the number of diagnostic categories.
Comparison with existing evidence
Most previous studies have examined risks of self-harm and violent offending in separate cohorts without the possibility of comparing magnitudes and patterns of risks for different outcomes in the same cohort. Our results do, however, largely concur with results reported from single-outcome cohort studies in the published literature. For instance, Gunnell et al. [Reference Gunnell, Hawton, Ho, Evans, O’Connor and Potokar7] examined the risk for readmission following self-harm and reported elevated risks among individuals diagnosed with substance misuse disorders and in a miscellaneous “other” diagnostic category. The latter consisted predominantly of personality disorders, concurring with our finding of especially high cumulative incidence values for those two diagnostic groups. Similar patterns were observed by Mellesdal et al. [Reference Mellesdal, Kroken, Lutro, Wentzel-Larsen, Kjelby and Oedegaard10]. However, prior to our study, no further examination of gender- and diagnosis-specific risks of self-harm post-discharge has to date been conducted. Direct inter-study comparison of risks across diagnostic categories relies on a similar set of diagnostic codes being used in delineating those groups. In the absence of a uniform approach, comparing our results to those reported by Gunnell et al. [Reference Gunnell, Hawton, Ho, Evans, O’Connor and Potokar7] and others is only possible to a limited degree.
There is a relatively large body of evidence concerning the risks of dying by suicide following contact with mental health services, and particularly following discharge from an inpatient admission. Using interlinked Danish registry data, as in our study, Nordentoft et al. [Reference Nordentoft, Mortensen and Pedersen16] examined suicide risks following contact with inpatient or outpatient mental health services, with estimates stratified by gender and psychiatric diagnostic category. The highest suicide risks observed were among both men and women diagnosed with bipolar disorder, unipolar affective disorder and schizophrenia, with co-occurring substance misuse and unipolar affective disorders further increasing risk. In another Danish registry study, Qin and Nordentoft [Reference Qin and Nordentoft20], focusing specifically on suicide risk following psychiatric admission, found particularly heightened risk among patients diagnosed with affective disorders and for women diagnosed with substance misuse disorders. However, this study also reported that suicide risk associated with affective disorders and schizophrenia spectrum disorders declined relatively quickly after treatment compared to the risk associated with substance misuse disorders. In a large US-based study conducted by Olfson et al. [Reference Olfson, Wall, Wang, Crystal, Liu and Gerhard21], suicide risk within 90 days of discharge was highest among males and females diagnosed with depressive disorders. Individuals with substance misuse disorders had comparatively low suicide rates in this cohort, a finding that contrasts with what we observed. However, the shorter length of follow-up (90 days compared to 1 year in our study) may not have captured the longer-term effects of substance misuse on suicide risk. Direct comparison with these findings is challenging due to our study outcome including both fatal and nonfatal self-harm episodes. However, given that self-harm is the strongest known risk factor for suicide, better understanding the spectrum of fatal and nonfatal self-harming behaviors among discharged inpatients is crucial; reducing risks of self-harm is a key and necessary component in suicide prevention strategies [11].
Exposure to family substance misuse in childhood is a common risk factor for the development of childhood emotional and behavioral disorders [Reference Ogundele22]. These diagnoses also commonly co-occur with other psychiatric diagnoses, including substance misuse, as well as involvement with the criminal justice system. Therefore, given that the diagnostic categories that we examined were not mutually exclusive, some of the elevated risk observed among the cohort members in our study is likely to partly reflect especially heightened risk among people with a co-occurring diagnosed or undiagnosed substance misuse disorder.
Several other investigations have explored the risk of violent criminal offending, including homicide perpetration, among individuals with a history of inpatient psychiatric treatment or in persons diagnosed with severe mental disorders, typically requiring inpatient treatment [Reference Fazel, Buxrud, Ruchkin and Grann8, Reference Fazel, Wolf, Palm and Lichtenstein9, Reference Schanda, Knecht, Schreinzer, Stompe, Ortwein-Swoboda and Waldhoer23–Reference Fazel and Grann25]. Most studies have focused exclusively on a specific subgroup of patients, such as those diagnosed with schizophrenia or other psychoses [Reference Fazel, Buxrud, Ruchkin and Grann8, Reference Fazel, Wolf, Palm and Lichtenstein9]. In our post-discharge study cohort, the absolute risk of interpersonal violence perpetration was not elevated among persons diagnosed with schizophrenia compared to most other psychiatric diagnoses. However, the absolute risk was still significantly greater than among cohort members who were diagnosed with mood disorders.
Clinical implications and future research
Patients diagnosed with substance misuse disorders should be offered treatment to address their condition whilst they are still inpatients, irrespective of the reason for their current admission. The positive effect of substance misuse treatment has been shown in several studies [Reference Prendergast, Podus, Chang and Urada26]. Thus, avoiding delays in receiving effective post-discharge treatments might lead to a reduction in post-discharge risks in this group. Furthermore, given that substance misuse disorders may have a more prolonged effect on increasing self-harm risk [Reference Qin and Nordentoft20], the benefits for patients and for services are likely to be substantial. Consideration of the specific needs of patients diagnosed with early onset behavioral and emotional disorders is indicated, particularly given the multitude of challenging and damaging situations likely to have been experienced by this group [Reference Ogundele22]. Given the high absolute risk for both adverse outcomes among those diagnosed with personality disorders, it is also especially important to put in place suitable interventions and treatment options for this high-risk group.
Recent adverse life events have also been shown to be associated with increased suicide risk after discharge from inpatient treatment [Reference Bickley, Hunt, Windfuhr, Shaw, Appleby and Kapur27] and should be considered by clinicians when planning further community-based mental health follow-up. Assessing the environment and social circumstances that patients are discharged into, and arranging appropriate longer-term follow-up, are likely to be particularly important in reducing interpersonal violence risk. Pre-discharge assessment of violence risk should be considered mindfully in relation to potentially complex ethical and legal implications [Reference Shaw28]. This assessment should include assessing known predictors, such as history of violence [Reference Tardiff, Marzuk, Leon and Portera29], and less commonly used approaches including asking patients about their violent thoughts [Reference Sanders, Milne, Brown and Bell30]. However, awareness of the complexity and limitations of violence risk assessment is crucial given that both static and dynamic factors influence likelihood of violent criminality involvement [Reference Beaudoin, Potvin, Dellazizzo, Luigi, Giguère and Dumais31]. Further research is therefore needed to provide better guidance for clinicians.
Care planning and coordinated approaches encompassing an array of support services can aid in reducing risks of self-harm and interpersonal violence to protect discharged patients and their families and communities. Therefore, primary and secondary care services should aim to improve the transition from inpatient care, for instance by providing timely at-home care [Reference Farrelly, Brown, Rose, Doherty, Henderson and Birchwood32]. Care coordinators can enhance this process by supervising and streamlining support in the post-discharge period [Reference Houghton, Bowling, Clarke, Hopkins and Jones33, Reference Walker, Naji, Howie, Andrew, Cameron and Eagles34]. Although there is some evidence as regards improving the safety of discharged persons as well as the safety of those in their communities, future research should establish specifically which preventive measures are most effective in reducing risks of self-harm and interpersonal violence in this high-risk group. The positive effects of peer-delivered interventions [Reference Fuhr, Salisbury, De Silva, Atif, van Ginneken and Rahman35] warrant further research into whether these concepts are suitable for the adverse outcomes examined in this study. Identifying those individuals who are at highest risk for engaging in either of these two harmful behaviors is paramount, and researchers should aim to understand the multiple determinants involved in driving the risk elevations that we and other investigators have observed.
Strength and limitations
This epidemiological study has revealed informative novel insights into two commonly occurring outcomes among persons discharged from inpatient psychiatric services. It was conducted using high-quality interlinked national registry data with a high degree of completeness and accuracy. The study cohort was large enough to enable analysis with a high degree of statistical power and precision. However, the study had two significant limitations. First, the outcome information that was extracted from these routinely collected administrative datasets was not comprehensive. This is especially pertinent to episodes of nonfatal self-harm that occurred in the community and that did not result in a hospital presentation. Therefore, the registered episodes are overrepresented by more medically serious ones [Reference Geulayov, Casey, McDonald, Foster, Pritchard and Wells36]. Interpersonal violence episodes included only criminal offense convictions, thereby excluding police-reported cases and those that went to court and were subsequently dismissed without a conviction, and episodes of interpersonal violence that were not reported to the authorities [Reference Steadman, Mulvey, Monahan, Robbins, Appelbaum and Grisso1]. Second, for early onset behavioral and emotional disorders, alignment is poor between ICD-8 coding (used between 1969 and 1993) and ICD-10 coding (from 1994) (see eTable 1 in the Supplementary Material). Many individuals who presented with symptoms of these disorders likely will not all have been diagnosed and registered under this category prior to 1994, resulting in misclassification and underreporting of these cases. We were therefore unable to investigate disorder-specific subsets within this broad diagnostic category.
Conclusion
By providing gender-specific absolute risk estimates according to diagnostic category, our results aid in identifying those individuals at greatest risk of physically harming themselves or other people post-discharge. This informs clinicians to help them to ensure that discharged persons receive the care that they need to keep them and their environment safe. This study has shown the elevated risk for self-harm and interpersonal violence across the spectrum of psychiatric diagnostic categories among people discharged from their first inpatient psychiatric admission. Although risk of self-harm was considerable in the short and longer-term in both genders, risk of violent behavior should also be addressed, particularly among discharged male patients with certain types of disorders. Persons diagnosed with substance misuse disorders, personality disorders and early onset behavioral and emotional disorders were at especially elevated risk for these adverse outcomes. Clinicians must be aware of the greatly raised risks in these specific patient groups and ensure appropriate care and support is offered following discharge.
Patients discharged from inpatient psychiatric care are at greatly elevated risk of perpetrating interpersonal violence, but it is crucial not to further stigmatize this already marginalized group. Even if the absolute risk in these individuals could be reduced to the same level as for persons without a history of psychiatric hospitalization, the total volume and societal burden of interpersonal violence would not be greatly altered. Our findings indicate a need for optimal care at discharge and during the challenging transition that these patients face in resuming their lives in the community, including targeted and individualized inter-agency support and interventions.
Data Availability Statement
Permission to access our study data is only granted to researchers in the study team. Researchers can apply to access Danish registry data to conduct other studies, in collaboration with experts based at a Danish academic institution.
Financial Support
This study was funded by a Medical Research Council Doctoral Training Partnership PhD studentship (F.W.) and by European Research Council starting grant (R.T.W., Grant Number 335905).
Author Contribution
MJC, PLHM, CBP, FW and RTW conceptualised the study. SA, MJC and CBP advised on statistical matters, and the analyses were carried out by PLHM. PLHM and FW initially drafted the article’s manuscript as joint first authors, and all other authors (SA, MJC, NK, CBP, JS, SS and RTW) critically reviewed the initial draft and subsequent versions, thereby providing intellectual input that led to revision of the material that is presented in the published article. All authors read the submitted manuscript and approved it prior to its submission.
Conflicts of Interest
N.K. reports grants and personal fees from the UK Department of Health and Social Care, the National Institute of Health Research (NIHR), the National Institute for Health and Care Excellence (NICE), and the Healthcare Quality and Improvement Partnership, outside the submitted work; works with NHS England on national quality improvement initiatives for suicide and self-harm; is a member of the National Suicide Prevention Strategy advisory group at the Department of Health and Social Care; has chaired NICE guideline committees for Self-harm and for Depression; and is currently the Topic Advisor for the new NICE Guidelines for self-harm. The remaining authors declare none.




Comments
No Comments have been published for this article.