The United States has a shortage of trained healthcare epidemiologists. The field of infectious diseases overall has had trouble recruiting physician trainees in recent years, with only 82% of fellowship positions being filled in the 2021 match. 1 Healthcare epidemiology as a subspecialty of infectious diseases does not have an accredited fellowship program, and only a few nonaccredited, dedicated fellowship programs exist. No estimate of how many formally trained healthcare epidemiologists currently work in the United States has been published.
The COVID-19 pandemic has highlighted the critical importance of the fields of healthcare epidemiology and infection prevention. Coinciding with this heightened awareness and appreciation for infection prevention specialists were Herculean demands that have contributed to burnout and infection prevention workforce erosion. Reference Nori, Stevens and Patel2
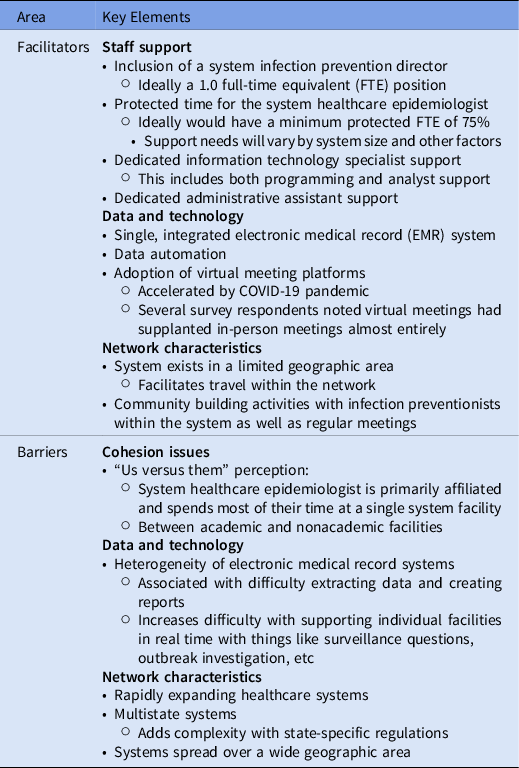
Hospitals are increasingly consolidating into health systems. Reference Furukawa, Machta and Barrett3 With this expansion has come a need for system-level coordination of key programs. Some health systems have appointed system healthcare epidemiologists to oversee system-level infection prevention activities. Best practices for healthcare epidemiologist–led, health-system–wide approaches to the prevention of healthcare-associated infections (HAIs) are urgently needed. We interviewed 7 healthcare epidemiologists with recent experience leading and building health system-based infection prevention programs who self-identified in response to a query on a longstanding e-mail group of healthcare epidemiologists. These informal surveys were used to identify several key themes (Table 1).
Table 1. Key Facilitators and Barriers for System Infection Prevention Program Implementation and Function
The hospital epidemiologists who were interviewed had been in their system healthcare epidemiology leadership roles for an average of 5.4 years (range, 1–11). Protected time ranged from 50%–100% (mean, 79%). None of the interviewees had clinical responsibilities in an outpatient clinic, and inpatient service responsibilities ranged from 0 to 10 weeks per year (mean, 5.6). The number of inpatient facilities covered in each health system ranged from 5 to 40 (median, 13), and all were also responsible for outpatient facilities. Also, 4 hospital epidemiologists (57%) were responsible for systems spanning multiple states.
In addition to the key facilitators and barriers identified in Table 1, several other key themes emerged. Lack of data access was a challenge. Although most systems produce system-level HAI-outcome dashboards and report on hand hygiene compliance, none regularly produced comprehensive system-level process-measure dashboards. Most of the respondents reported through their system’s chief quality officer or chief medical officer and had limited direct authority over system personnel. Identifying local culture and engaging local stakeholders were considered critically important. Community building among infection prevention personnel was also considered vital. Many of the respondents also served as the primary healthcare epidemiologist for individual system facilities (often academic hospitals). This overlap could lead to concerns about bias by some system facilities, which could undermine influence and negatively impact team building. Many were working to create system-level infection prevention policies and noted that COVID-19 had facilitated this work. A few systems had adopted centralized HAI surveillance.
System healthcare epidemiologists added value in several ways: overseeing data quality; report standardization; establishing, implementing, and assuring compliance with best practices; sharing knowledge gained from HAI events and regulatory surveys; providing expertise with product value analysis; advocating for infection preventionist support locally and at the system level; and promoting research and innovation. Policy unification and data automation were identified as future opportunities. Many programs also planned on adopting centralized HAI surveillance. Additionally, a goal of multiple programs was reporting system-level process metrics.
Data on system-level infection prevention programs are limited. Barnes et al Reference Barnes, Zirges and Tomas4 surveyed a group of corporate and system-level directors of infection prevention in 2016. Of the 32 respondents, only 37% had physician support funded for their corporate programs. The training background for the involved physicians and their roles within these programs was not described. Although the survey did not explore the potential advantages of physician engagement in system-level infection prevention programs, these researchers postulated that physician involvement would benefit programs in several ways. These benefits included influencing executives and physicians with practice change, assistance with analyzing data and assessing risk, helping to set program goals, and supporting individual facilities lacking direct physician support. The respondents noted varied program structure and support, but most had the support of a data analyst (1–4 FTEs). Most corporate infection prevention directors (75%) had some sort of direct authority over infection preventionists in individual facilities. Reference Barnes, Zirges and Tomas4
Infection prevention and antimicrobial stewardship programs share similarities in strategies, infrastructure, and key metrics. Reference Assi, Abbas and Nori5 Buckel et al Reference Buckel, Stenehjem and Hersh6 published an analysis of 20 system-level antimicrobial stewardship programs. They identified 4 program models ranging from centrally led teams with formal system-level leadership, resources, and participation requirements to collaborative teams with no formal structure and voluntary participation. Barriers to implementing centralized stewardship programs included inadequate data infrastructure and staff funding as well as securing local facility participation. Reference Buckel, Stenehjem and Hersh6 Inadequate data infrastructure and staff funding support were also noted as key barriers to system infection prevention program creation in our informal survey.
We hope that our experience will be of value to those considering system healthcare epidemiologist positions. Ultimately, research is needed to determine the impact of system coordination on HAI reduction and healthcare worker safety. Additionally, key resources and training standards should be delineated. System-level infection prevention programs have enormous potential to capitalize on the knowledge and expertise of the limited number of trained healthcare epidemiologists and to expand and transform HAI prevention.
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
R.A.M. reports funding from the Centers for Disease Control and Prevention. G.M.S. is an advisor for Infectious Diseases Connect. All other authors report no relevant financial conflicts of interest.



