To the Editor—Prior to the coronavirus disease 2019 (COVID-19) pandemic, serum procalcitonin (PCT)-based antimicrobial stewardship (AMS) algorithms have been shown to be effective at differentiating between bacterial and nonbacterial respiratory tract infection, leading to improved mortality, less antibiotic use, and decreased risk of antibiotic side effects.Reference Schuetz, Wirz and Sager1 In the context of COVID-19, initial reports of the utility of PCT were from hospitalized patients in whom PCT was found to correlate with disease severity, longer intensive care unit (ICU) stay, and inpatient mortality, along with a range of other biochemical markers.Reference Chen, Wu and Guo2–Reference Chen, Wu and Chen4 However, PCT would have unique value if its measurement at admission for COVID-19 or at time of clinical deterioration could be an important discriminator between bacterial coinfection versus noninfectious cause, allowing for improved AMS.Reference Han, Gatheral and Williams7 Widespread use of empiric antibiotics is occurring globally in patients hospitalized with COVID-19, despite low rates of microbiologically proven bacterial infection.Reference Vaughn, Gandhi and Petty5,Reference Huttner, Catho, Pano-Pardo, Pulcini and Schouten6
We investigated whether PCT was associated with commencement of antibiotic therapy. Additionally, we examined whether PCT was associated with duration of antibiotic therapy, intravenous-to-oral antibiotic switch, and other clinical and biochemical markers of COVID-19 severity.
A single-center, prospective, observational cohort study of patients with COVID-19 admitted to Austin Health (Melbourne, Australia) was undertaken. All patients were admitted to a specialized, multidisciplinary unit coordinated by infectious diseases physicians. PCT was measured at the time of ICU admission or at clinician discretion outside the ICU. Patients were stratified based on their initial PCT measurement into normal (<0.07 µg/L), medium (0.07 µg/L – 0.5 µg/L) and high (>0.5 µg/L) groups, based on consensus guidelines and recently published data in a COVID-19 patient group.Reference Vaughn, Gandhi and Petty5,Reference Schuetz, Beishuizen and Broyles8 Demographic, clinical, and laboratory data were also collected. Statistical analysis was performed using Stata version MP 16.1 software (StataCorp, College Station, TX). We used χ2 and rank-sum tests for univariate analysis according to PCT strata. Given the limited sample size, multivariable analysis was not performed.
In total, 166 patients were admitted with COVID-19 at the Austin Hospital between March and September 2020. Of these, 55 had at least 1 PCT measurement during their admission (Table 1). Most patients had PCT measured within the first day of admission (median days, 1; interquartile range [IQR], 0–3). Blood cultures were taken in 42 of 55 patients, with 3 positive results (4.7%) (Blood culture organisms: Enterobacter cloacae, PCT 38.8 µg/L; Escherichia coli, PCT 1.37 µg/L; Staphylococcus epidermidis, PCT 0.14 µg/L).
Table 1. Demographics, Laboratory Parameters, Treatment Parameters, and Outcomes for Normal PCT, Medium PCT, and High PCT Groups
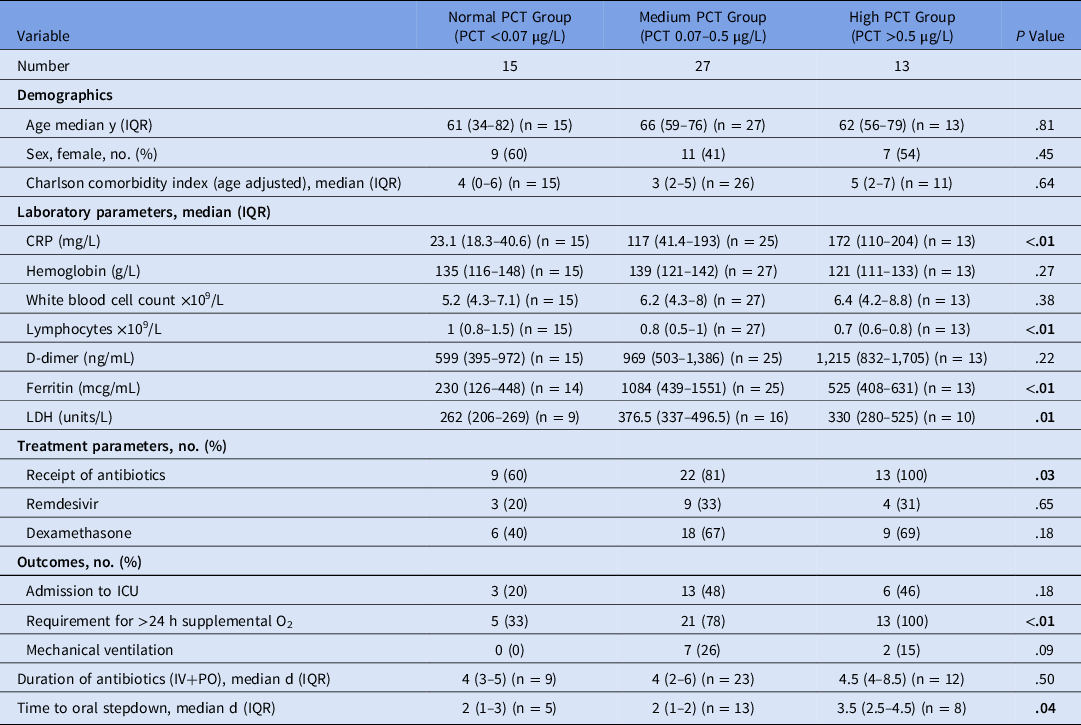
Note. PCT, serum procalcitonin; CRP, C-reactive protein; LDH, lactate dehydrogenase; IQR, interquartile range; O2, oxygen; IV, intravenous; PO, oral; ICU, intensive care unit.
PCT levels were significantly associated with antibiotic use (P = .03). In total, 44 of 55 patients (80%) received antibiotic therapy during their admission. Of 15 patients, 9 (60%) with normal PCT received antibiotic therapy during their admission, compared with 22 of 27 patients (81%) in the medium PCT group, and 13 of 13 patients (100%) in the high PCT group. In those who received antibiotics, PCT was not associated with total duration of antibiotic therapy (P = .50). PCT was associated with earlier de-escalation to oral therapy, with a median duration of 2 days prior to step down in the normal and medium PCT groups versus 3.5 days in the high PCT group (P = .04).
PCT levels were associated with supplemental oxygen requirements during admission. Moreover, 100% of patients in the high PCT group required supplemental oxygen, compared with only 35% of patients in the normal PCT group (P < .01). PCT was not associated with requirement for ICU admission or with dexamethasone and remdesivir therapy. Serum PCT levels were associated with C-reactive protein (CRP) (P < .01), lymphocytes (P ≤ .01), ferritin (P < .01), and lactate dehydrogenase (LDH) (P = .01).
In our experience with PCT in COVID-19, we have noted that changes in serum PCT are associated with both initiation of antibiotic therapy, and intravenous-to-oral switch. These findings highlight the potential utility of PCT as a component of antimicrobial stewardship interventions.Reference Bennouar, Bachir Cherif and Kessira10,Reference Sheng, Wang, Tang, Meng, Huang and Li11 Indeed, all patients in the high PCT group received antibiotics during their admissions, while 20% in the medium PCT group and 40% in the low PCT group did not receive any antibiotic therapy. This finding suggests that clinicians were more comfortable withholding antibiotic therapy in patients with lower PCT, which may represent a stewardship intervention opportunity.
Once initiated, the total duration of antibiotic therapy (intravenous [IV] and oral) was the same across the groups. However, we found a significant association between PCT and de-escalation to oral therapy. Patients in the high PCT group received, on average, 1.5 days of additional IV antibiotics compared to those in the medium- and low-PCT groups, suggesting increased clinician comfort in de-escalating antibiotics for patients without high PCT.
Although our study was limited by small study size and nonrandomized design, our results still suggest that, in COVID-19 patients, measurement of PCT, in conjunction with other clinical assessment, may have a role in prognostication and decision-making algorithms for a wider group of patients than only those admitted to ICU, aiding AMS interventions in this cohort.
Acknowledgments
The authors acknowledge the work of Dr Que Lam, Chemical Pathologist, Austin Pathology and the Departments of Infectious Diseases, Clinical Biochemistry, and the COVID Unit at Austin Health, Heidelberg, Australia.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




