Weight-loss programmes based on restricted eating are becoming more and more popular in social contexts where being slim is perceived as ideal but being overweight has become more common. The long-term benefits of such programmes are questionable, as the majority of individuals eventually regain the weight they lose( Reference Jeffery, Epstein and Wilson 1 , Reference Mann, Tomiyama and Westling 2 ). Previous research examining the success of dieting has concluded that diets lead to short-term weight loss, usually 5–10 % of body weight, but this weight loss is not maintained in the long term by the majority of people( Reference Jeffery, Epstein and Wilson 1 – Reference Garner and Wooley 3 ). It has been estimated that about 20 % of individuals with overweight are successful at long-term weight loss, when defined as losing at least 10 % of one’s initial body weight and maintaining the loss for at least 1 year( Reference Wing and Phelan 4 ). Most weight-loss diets expect people to constantly control consumption. However, poor long-term results suggest that the majority of persons who have overweight cannot sustain rigid control.
In contrast to controlled eating, intuitive eating is a style of eating that follows the natural contingencies of an individual’s perception of physical hunger and satiety cues rather than emotional or environmental cues( Reference Avalos and Tylka 5 , Reference Tylka 6 ). Three central and interrelated components of intuitive eating have been identified: (i) unconditional permission to eat when hungry and what food is desired (i.e. lack of restrictions in eating); (ii) eating for physical rather than emotional reasons; and (iii) reliance on internal hunger and satiety cues to determine when and how much to eat( Reference Tylka 6 ). Intuitive eating has found to be related to the absence of eating disorder symptoms( Reference Tylka 6 ) and to better psychological( Reference Tylka 6 , Reference Bacon, Stern and Van Loan 7 ) and physical health, such as lower BMI( Reference Tylka 6 , Reference Augustus-Horvath and Tylka 8 , Reference Hawks, Madanat and Hawks 9 ), cholesterol levels and blood pressure( Reference Bacon, Stern and Van Loan 7 ). Despite the promising results related to intuitive eating, few studies have attempted to explain the processes supporting intuitive eating regulation. What self-regulation processes are needed in order to resist eating based on emotional or external cues?
Overeating in response to emotional experiences and external cues (e.g. presence of palatable food) can be understood as a failure in self-regulation( Reference Forman and Butryn 10 ). Studies have indicated that persons with obesity who have difficulty losing or keeping off weight more often use food as a source of comfort and satisfaction( Reference Castelnuovo-Tedesco and Schiebel 11 ), eat after difficult interpersonal situations( Reference Hockley 12 ) and eat in response to negative emotions( Reference Hudson and Williams 13 ). Consequently, the function of emotional eating appears to be experiential avoidance that is an attempt to avoid negative private experiences (thoughts, feelings, sensations). Experiential avoidance is a central process in the development of a range of mental health and behavioural health problems( Reference Hayes, Luoma and Bond 14 , Reference Lillis and Hayes 15 ) including eating-related difficulties( Reference Forman, Hoffman and McGrath 16 – Reference Lillis, Hayes and Bunting 18 ). Accordingly, ‘third wave’ behaviour therapies, such as acceptance and commitment therapy (ACT), focus on avoidance by helping individuals to relate flexibly to interfering private events and regulate their behaviour based on personal values and goals instead of emotional experiences or thoughts( Reference Hayes, Strosahl and Wilson 19 ).
More precisely, ACT is expected to improve individuals’ functioning and quality of life by increasing their psychological flexibility including mindfulness skills. Psychological flexibility and mindfulness are adaptive regulation and coping processes that can be seen as opposites to experiential avoidance( Reference Kashdan and Rottenberg 20 ). Psychological flexibility is defined as the ability to act effectively in accordance with one’s personal values in the presence of interfering thoughts, emotions and bodily sensations( Reference Hayes, Luoma and Bond 14 ). Mindfulness can be described as an adaptive regulation process involving enhanced attention and non-judgemental awareness concerning present-moment experiences( Reference Brown and Ryan 21 , Reference Chambers, Gullone and Allen 22 ). The current state of evidence suggests that the concepts specified by the ACT model work very consistently as mediators across the wide range of problems, including eating-related issues( Reference Lillis, Hayes and Bunting 18 ), targeted by ACT. Successful ACT mediators include general or specific measures of acceptance and psychological flexibility( Reference Gifford, Kohlenberg and Hayes 23 – Reference Lillis and Hayes 27 ), defusion( Reference Lundgren, Dahl and Hayes 25 , Reference Varra, Hayes and Roget 28 , Reference Zettle and Hayes 29 ), values( Reference Lundgren, Dahl and Hayes 25 ) and mindfulness( Reference Forman, Hoffman and McGrath 16 ).
Psychological flexibility and mindfulness promote the willingness to approach and experience emotions and are therefore likely to reduce experiential avoidance, such as emotional eating. Mindfulness practice has been suggested to help individuals ‘connect’ with their inner experiences, such as hunger, thereby attenuating their sensitivity to external or emotional cues to eat( Reference Kristeller and Wolever 30 , Reference Alberts, Thewissen and Raes 31 ). On a cognitive level, mindfulness has been proposed to reduce identification with thoughts about food, body and shape, thereby interrupting dysfunctional thinking patterns( Reference Albers 32 ) that could predispose someone to emotional or restricted eating. Thus, psychological flexibility and mindfulness can be possible self-regulation processes that promote adaptive eating behaviours, such as intuitive eating, and offer a new approach to effecting weight management.
The current study is based on a recent randomized controlled trial comparing three psychological lifestyle interventions aimed at improving the well-being of adults with overweight experiencing psychological stress: (i) an ACT-based face-to-face group intervention; (ii) an ACT-based mobile intervention; and (iii) a web-based education intervention (for details of the design, see Lappalainen et al.( Reference Lappalainen, Sairanen and Järvelä 33 )). Kolehmainen and colleagues (M Kolehmainen, E Sairanen, E Järvelä-Reijonen et al., unpublished results) found that psychological flexibility related to weight issues improved in ACT intervention groups. The current study sought to further examine the effects of the ACT interventions on psychological processes and adaptive eating behaviour. The aim was to provide a complementary perspective on the role of acceptance and flexibility in the context of intuitive eating by evaluating the mediating effects of mindfulness and psychological flexibility on intuitive eating and weight in terms of improvements. We were interested to see if processes specified by the ACT model worked as mediators in contrast to non-ACT-related processes. Accordingly, the mediating effects of psychological flexibility and mindfulness were investigated in comparison with sense of coherence, a variable less associated with ACT yet commonly used to explain how people manage stressful situations and stay well( Reference Eriksson and Lindstrom 34 ).
The specific aims of the present study were as follows. First, we investigated the effects of the ACT interventions – face-to-face (in a group) and mobile (individually) – on intuitive eating, mindfulness and sense of coherence in comparison with each other and a control group. The face-to-face and mobile ACT interventions were expected to have similar effects on all measurements. Intervention effects on weight and psychological flexibility have been reported elsewhere (M Kolehmainen, E Sairanen, E Järvelä-Reijonen et al., unpublished results) and are presented as descriptive statistics herein. Second, we examined whether (i) psychological flexibility (general and weight specific), (ii) mindfulness skills and (iii) sense of coherence mediate the intervention effect on intuitive eating and weight in ACT interventions. The changes in psychological flexibility and mindfulness skills were expected to mediate the intervention effects similarly in both ACT interventions. Psychological flexibility and mindfulness were expected to be more important mediators in the ACT interventions than was sense of coherence.
Methods
Participants
The data of the present study stem from a larger lifestyle intervention study( Reference Lappalainen, Sairanen and Järvelä 33 ) that investigated the effects of three low-intensity psychological interventions concerning psychological flexibility, metabolic syndrome risk factors and general well-being among individuals with overweight or obesity experiencing stress. The study design and interventions of the larger study are described in detail elsewhere( Reference Lappalainen, Sairanen and Järvelä 33 ) and briefly here. The participants for the study were recruited through advertisements in local newspapers and selected based on specific inclusion criteria: BMI of 27·0–34·9 kg/m2 (based on self-reported weight and height), age 25–60 years and reporting symptoms of perceived psychological stress (scored at least 3 out of 12 points on the General Health Questionnaire( Reference Makowska, Merecz and Moscicka 35 )). The study took place in Finland.
In the larger study, altogether 298 participants completed the baseline measurements and were randomly divided into an ACT face-to-face intervention group (n 70), an ACT mobile intervention group (n 78), a web-based education intervention group (n 79) and a non-treatment control group (n 71). The participants of both ACT interventions (face-to-face and mobile) and the non-treatment control group comprised the study population of the present study (N 219; 15·5 % male; 84·5 % female). The web-based education group was excluded from the present study because it could not be compared with the ACT interventions since it had both different content and form of the programme. The mean age of the participants in the present study was 49·5 (sd 7·4) years (range 26·6–60·8 years) and their mean BMI was 31·3 (sd 2·9) kg/m2 (range 25·7–40·1 kg/m2). About half of the participants had an upper secondary education (51·6 %) and 45·7 % had a university degree. All participants were Caucasian and had Finnish as their native language.
Interventions
ACT face-to-face group intervention
The ACT face-to-face group intervention consisted of six group sessions during an 8-week period, with each session lasting about 90 min. The intervention programme aimed to support lifestyle changes and to enhance well-being through committed actions based on personally important values. The topics of the six sessions were: (i) my life here and now; (ii) values and mindful living; (iii) value-based actions and barriers; (iv) the observing self and acceptance; (v) mindful eating; and (vi) summary and reflection. Every session included experiential exercises based on the ACT model (such as mindfulness and acceptance exercises and individual activation through value work), pair and group discussions, and homework related to the topic of the session (for a more detailed description of these interventions, see Lappalainen et al.( Reference Lappalainen, Sairanen and Järvelä 33 )).
ACT mobile intervention
The participants in the ACT mobile intervention were invited to a group meeting that consisted of a brief overview of ACT principles. In the meeting, the participants were given smartphones that were pre-installed with a stand-alone mental wellness training application( Reference Ahtinen, Mattila and Välkkynen 36 ). They were instructed to use the application on their own during the 8-week intervention period. The application contained short exercises (n 41) that teach ACT skills to be applied in daily life. The mobile application delivered an ACT-based intervention programme similar to that of the face-to-face group.
Control group
The participants randomized into the control group participated in all of the measurements but were not part of any intervention.
Measurements
Participants completed an Internet-based survey at the pre, post (10weeks after the pre), and follow-up (36weeks after the pre) measurement points of the study. Body weight and height were measured at pre, post and follow-up laboratory visits. The BMI was calculated based on the measured weight and height data.
Intuitive eating
The Intuitive Eating Scale (IES)( Reference Tylka 6 ) is a twenty-one-item instrument containing three subscales that assess the components of intuitive eating: (i) Unconditional Permission to Eat (Permission; nine items, e.g. ‘If I am craving a certain food, I allow myself to have it’); (ii) Eating for Physical rather than Emotional Reasons (Reasons; six items, e.g. ‘I stop eating when I feel full (not overly stuffed)’); and (iii) Reliance on Internal Hunger and Satiety Cues (Cues; six items, e.g. ‘I trust my body to tell me how much to eat’). Participants rated the items on a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The subscale items were averaged, with higher scores indicating higher levels of intuitive eating. The internal consistency of the IES and its subscales was high (Cronbach’s α: IES total=0·80, Permission=0·70, Reasons=0·86, Cues=0·76).
Mindfulness
The Five Facet Mindfulness Questionnaire (FFMQ)( Reference Lattimore, Fisher and Malinowski 37 ) is a thirty-nine-item measure of being mindful in daily life. It measures the following five elements of mindfulness: (i) Observing (eight items), which includes noticing or attending to internal and external experiences such as sensations, cognitions, emotions, sights, sounds and smells; (ii) Describing (eight items), which involves labelling internal experiences with words; (iii) Acting with Awareness (ActAware; eight items), which represents attending to one’s activities of the moment and can be contrasted with behaving mechanically or automatically while attention is focused elsewhere; (iv) Non-judgement of Inner Experiences (NonJudge; eight items), which represents taking a non-evaluative stance towards feelings and thoughts; and (v) Non-reactivity to Inner Experiences (NonReact; seven items), which is the tendency to allow thoughts and feelings to come and go without getting carried away by or caught up in them. The items were rated on a 5-point Likert-type scale ranging from 1 (never or very rarely true) to 5 (very often or always true), with higher scores indicating higher levels of mindfulness. The internal consistency of the FFMQ and its subscales was high (Cronbach’s α: FFMQ total=0·91, Observing=0·72, Describing=0·94, ActAware=0·89, NonJudge=0·90, NonReact=0·84).
Psychological flexibility
Psychological flexibility was assessed using the general Acceptance and Action Questionnaire II (AAQ-II)( Reference Bond, Hayes and Baer 38 ) and the Acceptance and Action Questionnaire for Weight (AAQW)( Reference Lillis and Hayes 15 ). The AAQ-II is a seven-item Likert-type questionnaire that assesses the ability to accept aversive internal experiences and to pursue goals in the presence of these experiences. Some items target emotional acceptance or avoidance while others address the tendency to become entangled in thoughts, to take them literally, or, conversely, to see them simply as thoughts; still others ask about the ability to take value-based actions in the presence of difficult thoughts, or about the tendency to become behaviourally inactive or avoidant. The questions of the AAQ-II are based on statements like ‘I worry about not being able to control my worries and feelings’ and ‘My thoughts and feelings do not get in the way of how I want to live my life’. The items were rated on a 7-point Likert-type scale ranging from 1 (never true) to 7 (always true), with higher scores indicating lower levels of psychological flexibility and thus higher levels of experiential avoidance. The internal consistency for the AAQ-II was excellent, with a Cronbach’s α of 0·91.
The AAQW( Reference Lillis and Hayes 15 ) is a twenty-two-item Likert-type scale that measures acceptance levels of weight-related thoughts and feelings and the degree to which they interfere with valued actions (e.g. ‘I try hard to avoid feeling bad about my weight or how I look’). The items were rated on a 7-point Likert-type scale ranging from 1 (never true/not at all believable) to 7 (always true/completely believable), with higher scores indicating lower levels of psychological flexibility and thus higher levels of experiential avoidance. The questions of the AAQW are based on statements like ‘When I evaluate my weight or my appearance negatively, I am able to recognize that this is just a reaction, not an objective fact’ and ‘I need to feel better about how I look in order to live the life I want’. The internal consistency for the AAQW was excellent, with a Cronbach’s α of 0·90.
Sense of coherence
Sense of coherence (SOC) was measured with the thirteen-item Orientation to Life Questionnaire (SOC-13)( Reference Antonovsky 39 , Reference Antonovsky 40 ). The scale consists of three dimensions: Comprehensibility (five items, e.g. ‘Do you have very mixed-up feelings and ideas?’), Manageability (four items, e.g. ‘How often do you have feelings that you’re not sure you can keep under control?’) and Meaningfulness (four items, e.g. ‘How often do you have the feeling that there’s little meaning in the things you do in your daily life?’). The participants were asked to answer the questions on a 7-point semantic differential scale from 1 (never) to 7 (always), with the total sum ranging from 13 (lowest SOC) to 91 (highest SOC). The internal consistency for the SOC-13 was good, with a Cronbach’s α of 0·87.
The measures were written in Finnish. The SOC-13 has been indicated to have good validity in Finnish studies( Reference Suominen, Blomberc and Helenius 41 , Reference Suominen, Helenius and Blomberg 42 ). The IES was translated and back-translated by experts in nutrition and eating behaviour. AAQ-II, AAQW and FFMQ scales were translated by a group of researchers with long experience in acceptance-, mindfulness- and value-based interventions. Previous studies with these measurements have shown comparable results to studies using the original scales( Reference Sairanen, Tolvanen and Karhunen 43 , Reference Lappalainen, Langrial and Oinas-Kukkonen 44 ).
Statistical analysis
The statistical analyses were conducted using the software Mplus version 7 and the statistical software package IBM SPSS Statistics version 20. The parameters were estimated using the full information maximum likelihood method (MLR estimation in Mplus). In the data, missing values (0–12·8 %) were assumed to be missing at random (MAR).
Intervention effects were analysed using the hierarchical linear model (HLM) and effect sizes. Intervention effects, as well as indirect effects, were analysed by first comparing the ACT face-to-face and mobile interventions with each other. If no difference was observed over time between these two ACT intervention groups, then they were combined and together compared with the control group. If the ACT intervention groups showed different effects, then they were separately compared with the control group. The effect sizes were calculated by comparing the mean difference in change (d i −d c ) between the intervention groups (subscript i) and the control group (subscript c), using the equation:
 $${\rm Cohen’s}\,d\,{\equals}\,{{d_{i} {\minus}d_{c} } \over {{1 \over 3}\mathop{\sum}\limits_{j\,{\equals}\,1}^3 {sd_{j} } }};\,\quad d_{x} \,{\equals}\,\left( {\bar{y}_{{{\rm fup}}} {\minus}\bar{y}_{{\rm pre}} } \right);\,\quad x \,{\equals}\,\left{i\,{\rm or}\,c}$$
.
$${\rm Cohen’s}\,d\,{\equals}\,{{d_{i} {\minus}d_{c} } \over {{1 \over 3}\mathop{\sum}\limits_{j\,{\equals}\,1}^3 {sd_{j} } }};\,\quad d_{x} \,{\equals}\,\left( {\bar{y}_{{{\rm fup}}} {\minus}\bar{y}_{{\rm pre}} } \right);\,\quad x \,{\equals}\,\left{i\,{\rm or}\,c}$$
.Where:
![]() $$\bar{y}_{{{\mathop{\rm fup}\nolimits} }} $$
=mean of the variable in the follow-up measurement;
$$\bar{y}_{{{\mathop{\rm fup}\nolimits} }} $$
=mean of the variable in the follow-up measurement;
![]() $$\bar{y}_{{{\mathop{\rm pre}\nolimits} }} $$
=mean of the variable in the pre measurement;
$$\bar{y}_{{{\mathop{\rm pre}\nolimits} }} $$
=mean of the variable in the pre measurement;
![]() ${1 \over 3}\mathop{\sum}\nolimits_{j{\equals}1}^3 {sd_{j} } $
=mean of the standard deviation of the pre, post and follow-up measurements; and
${1 \over 3}\mathop{\sum}\nolimits_{j{\equals}1}^3 {sd_{j} } $
=mean of the standard deviation of the pre, post and follow-up measurements; and
sd=standard deviation.
In the first measurement, the difference was divided by the pooled sd. A between-group effect size of 0·2 was considered clinically small, 0·5 medium and 0·8 large( Reference Cohen 45 ).
The mediation analyses were conducted using the latent difference score (LDS) mediation model( Reference MacKinnon 46 ). Figure 1 shows the LDS model, where the effects of the ACT interventions on intuitive eating (change from pre to follow-up, ΔIES) are mediated by the change in psychological flexibility during the interventions as assessed with the AAQW (ΔAAQW). The product of the a and b coefficients in the LDS model comprises the mediation effect. In the measurement model, three parcels (e.g. A1–A3) were used to estimate the latent factors representing the true score without measurement error. By constructing three measured indicators (parcels) for each latent variable (i.e. psychological flexibility and intuitive eating), we followed the recommendation of Russell et al.( Reference Russell, Kahn and Spoth 47 ).
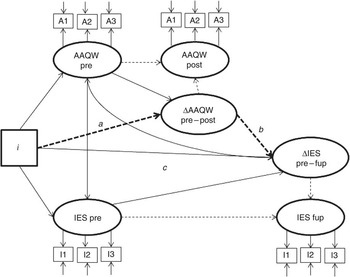
Fig. 1 The latent difference score mediation model, where the intervention effect on the IES (change from pre to fup) is mediated by the AAQW (change from pre to post). Note: i=0 for control group; i=1–2 for intervention groups (IES, Intuitive Eating Scale; AAQW, Acceptance and Action Questionnaire for Weight; pre, pre-intervention; post, post-intervention; fup, follow-up; regression coefficients marked as - - - - -> in the model are fixed to 1)
The LDS model was chosen because the focus was on variance in within-individual changes in true scores and on mean intervention effects. The LDS approach made it possible to focus on change (e.g. ΔAAQW) in each construct rather than only on levels (e.g. AAQW). Thus, we are suggesting that changes in behavioural processes (psychological flexibility, mindfulness skills and sense of coherence) are more important than, for example, psychological flexibility per se.
We followed the recommendation of Zhao et al.( Reference Zhao, Lynch and Chen 48 ) in the analysis of mediation. They have presented that the only requirement to demonstrate mediation is a significant indirect effect (a×b, see Fig. 1). It may be possible to establish an indirect effect despite no total direct effect( Reference Zhao, Lynch and Chen 48 ). The product of a and b may be significant even if the coefficients on their own are not( Reference MacKinnon, Lockwood and Hoffman 49 ). Mplus allows users to define any function of parameters (a×b) as a model parameter and in addition provides bias-corrected bootstrap CI for such parameters. CI are based on 1000 bootstrap resamples. Indirect effects are deemed statistically significant at the 0·05 level if the 95 % CI for the estimate of indirect effects does not include zero.
The fit of the models was evaluated using the following goodness-of-fit measures provided by the Mplus program( Reference Muthén 50 ): RMSEA (root-mean-square error of approximation, with values of 0·06 or less indicating a good fit); SRMR (standardized root-mean-square residual, with values less than 0·08 indicating a good fit); CFI (Bentler’s comparative fit index, with values of 0·95 or higher indicating a good fit); and TLI (Tucker–Lewis index, with values higher than 0·95 indicating a good fit)( Reference Hu and Bentler 51 ).
Results
Intervention effects
Changes in intuitive eating and weight during the interventions and at the 6-month follow-up measurement point are described in Table 1. Eating for Physical rather than Emotional Reasons, a component of intuitive eating, increased significantly in the ACT face-to-face and mobile groups compared with the control group (P=0·003). The increase was significant from the pre- to post-intervention measurement (P=0·001), but not from the post-intervention to follow-up measurement (P=0·718). The interventions did not have significant effects on the other two subscales of intuitive eating (Unconditional Permission to Eat and Reliance on Internal Hunger and Satiety Cues), nor on the total score of the IES or on weight in comparison with the control group.
Table 1 Changes in outcome measurements for the acceptance and commitment therapy (ACT) intervention (face-to-face and mobile) groups and control group. Between-group effect sizes and between-group analyses compare ACT interventions with the control group
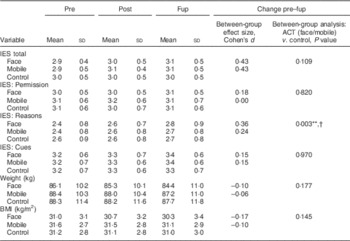
Pre, pre-intervention; post, post-intervention; fup, follow-up; IES, Intuitive Eating Scale; Permission, Unconditional Permission to Eat subscale; Reasons, Eating for Physical rather than Emotional Reasons subscale; Cues, Reliance on Internal Hunger and Satiety Cues subscale.
Means and sd were calculated using Mplus software version 7 with full information maximum likelihood estimates for the parameters. A between-group effect size of 0.2 was considered clinically small, 0·5 medium and 0·8 large( Reference Cohen 45 ).
**P<0·01.
† Difference in change scores from pre to post was significant at the P<0·05 level. Difference in change scores from post to fup was not significant at the P<0·05 level.
Changes in process measurements during the interventions and their follow-up are described in Table 2. Psychological flexibility for weight (AAQW) improved significantly in the ACT face-to-face and mobile groups during the respective interventions compared with the control group (P<0·001). In addition, participants’ tendency for Observing (subscale of FFMQ) increased significantly in both ACT groups in comparison to the control group from the pre- to the post-intervention measurement (P=0·001).
Table 2 Changes in process measurements for the acceptance and commitment therapy (ACT) intervention (face-to-face and mobile) groups and control groups. Between-group effect sizes and between-group analyses compare ACT Interventions with the control group
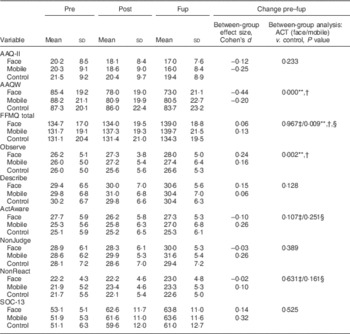
Pre, pre-intervention; post, post-intervention; fup, follow-up; AAQ-II, Acceptance and Action Questionnaire II; AAQW, Acceptance and Action Questionnaire for Weight; FFMQ, Five Facet Mindfulness Questionnaire; Observe, Observing subscale of FFMQ; Describe, Describing subscale of FFMQ; ActAware, Acting with Awareness subscale of FFMQ; NonJudge, Non-judgement of Inner Experiences subscale of FFQM; NonReact, Non-reactivity to Inner Experiences subscale of FFMQ; SOC-13, sense of coherence measured with the thirteen-item Orientation to Life Questionnaire.
Means and sd were calculated using Mplus software version 7 with full information maximum likelihood estimates for the parameters. A between-group effect size of 0·2 was considered clinically small, 0·5 medium and 0·8 large( Reference Cohen 45 ).
**P<0·01.
† Difference in change scores from pre to post was significance at the P<0·05 level. Difference in change scores from post to fup was not significant at the P<0·05 level.
‡ Between-group analysis comparing ACT face-to-face with the control group.
§ Between-group analysis comparing ACT mobile with the control group.
Mindfulness skills (FFMQ total) and its subscales Acting with Awareness and Non-reactivity to Inner Experiences improved more in the ACT mobile group than in the ACT face-to-face group (P=0·018, 0·021 and 0·043, respectively). Accordingly, they were separately compared with the control group. In the ACT mobile group, the FFMQ total increased significantly more compared with control from the pre- to the post-intervention measurement (P=0·002). Changes in Acting with Awareness and Non-reactivity to Inner Experiences were not significant in either of the ACT groups compared with the control group.
Mediation analysis
We were interested in whether changes in process variables (AAQ-II, AAQW, SOC-13, FFMQ and its subscales) during the active intervention period (from pre to post) mediated the long-term changes (from pre to follow-up) in intuitive eating and weight. All LDS mediation models showed an excellent fit to the data (RMSEA=0·000–0·072, SRMR=0·030–0·072, CFI=0·974–1·000 and TLI=0·959–1·014).
The estimates and 95 % CI of standardized indirect effects (a×b) in the LDS models are described in Table 3 (see Fig. 1). There were no significant differences in indirect effects between the ACT face-to-face group and the ACT mobile group; subsequently, the ACT groups were compared jointly with the control group. The 95 % CI for indirect effects – via the AAQW – on (i) weight (BMI), (ii) intuitive eating total and its subscales, (iii) Eating for Physical rather than Emotional Reasons and (iv) Reliance on Internal Hunger and Satiety Cues did not include zero. Thus, the LDS models suggested that the effect of the ACT interventions on those variables was mediated by the change in weight-related psychological flexibility (AAQW). The unstandardized regression coefficients (a, b and c) of the significant mediation models are presented in Table 4. There were no statistically significant direct effects (c; P<0·05; see Fig. 1) when the indirect path (a and b) was included in the model, indicating indirect-only mediation concerning all significant indirect effects( Reference Zhao, Lynch and Chen 48 ). The estimates for statistically significant indirect effects ranged from 0·05 to 0·08, indicating small effects (effect size >0·02( Reference Cohen 45 )).
Table 3 Estimates (and 95 % CI) for standardized indirect effects (a×b) from the latent difference score models, where the acceptance and commitment therapy (ACT) intervention (face-to-face and mobile) groups are compared with the control group
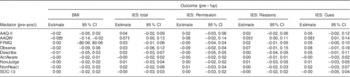
Pre, pre-intervention; post, post-intervention; fup, follow-up; IES, Intuitive Eating Scale; Permission, Unconditional Permission to Eat subscale; Reasons, Eating for Physical rather than Emotional Reasons subscale; Cues, Reliance on Internal Hunger and Satiety Cues subscale; AAQ-II, Acceptance and Action Questionnaire II; AAQW, Acceptance and Action Questionnaire for Weight; FFMQ, Five Facet Mindfulness Questionnaire; Observe, Observing subscale of FFMQ; Describe, Describing subscale of FFMQ; ActAware, Acting with Awareness subscale of FFMQ; NonJudge, Non-judgement of Inner Experiences subscale of FFQM; NonReact, Non-reactivity to Inner Experiences subscale of FFMQ; SOC-13, sense of coherence measured with the thirteen-item Orientation to Life Questionnaire.
† Indirect effects are deemed statistically significant at the 0.05 level if the 95 % CI for the estimate of indirect effects does not include zero.
Table 4 Unstandardized regression coefficients a, b and c (and P values) of the mediation models in which the Acceptance and Action Questionnaire for Weight (AAQW; pre–post) mediated the effect of the acceptance and commitment therapy Interventions on the outcome variables

Pre, pre-intervention; post, post-intervention; fup, follow-up; IES, Intuitive Eating Scale; Reasons, Eating for Physical rather than Emotional Reasons subscale; Cues, Reliance on Internal Hunger and Satiety Cues subscale.
Mindfulness skills (FFMQ and its subscales), general psychological flexibility (AAQ-II) and sense of coherence (SOC-13) did not mediate any intervention effects on intuitive eating and weight.
Discussion
The present study is one of the first to examine processes of change in psychological approaches to adaptive eating behaviour and weight management. Despite the promising results related to intuitive eating, few studies have attempted to explain the processes encouraging adaptive eating behaviour and previous studies on intuitive eating have been mainly observational in nature. Thus, the focus of the present study was on exploring mechanisms of change in intuitive eating and weight in the ACT intervention groups compared with the control group of participants having overweight.
First, the present results indicate that Eating for Physical rather than Emotional Reasons increased in the ACT-based intervention groups. The present findings support the theoretical assumption that ACT reduces avoidance behaviour, such as emotional eating. Considering the association between emotional eating and obesity( Reference Hudson and Williams 13 ), these results suggest that ACT-oriented interventions can have a positive impact on weight management and disordered eating. These results are in line with previous studies that have indicated that mindfulness practice reduces emotional and external eating( Reference Alberts, Thewissen and Raes 31 ), as well as binge eating( Reference Kristeller and Hallett 52 ). In the present study, the ACT mobile intervention also improved mindfulness skills (FFMQ total) and both ACT interventions enhanced Observing (subscale of FFMQ).
Second, the mediation analysis indicated that the intervention effects on weight and intuitive eating behaviours, Eating for Physical rather than Emotional Reasons and Reliance on Internal Hunger and Satiety Cues were mediated by change in weight-related psychological flexibility (AAQW) in the ACT interventions. Thus, the ACT interventions increased psychological flexibility (AAQW), which in turn promoted weight loss and eating based on bodily cues of hunger and satiety. In contrast, weight-related psychological flexibility was not found to mediate the interventions’ effect on Unconditional Permission to Eat. This may be due to the fact that ACT interventions emphasized more mindful eating than content reflected by the subscale of Unconditional Permission to Eat. Moreover, it could be speculated that ACT-based interventions might change the impact of emotional reactions to eating patterns.
The present findings support the idea that ACT-oriented interventions for lifestyle changes improve individuals’ ability to continue with valued activities even when confronted with negative emotions and thoughts related to weight, and this process mediated changes in eating regulation and weight. In accordance with our findings, population-specific measures of psychological flexibility have been significant mediators in many different areas, including with respect to smoking cessation( Reference Gifford, Kohlenberg and Hayes 23 ), diabetes self-care( Reference Gregg, Callaghan and Hayes 24 ), prejudice( Reference Lillis and Hayes 27 ), seizures and quality of life in epilepsy cases( Reference Lundgren, Dahl and Hayes 25 ), adaptive functioning in chronic pain patients( Reference McCracken, Vowles and Eccleston 53 – Reference Wicksell, Ahlqvist and Bring 55 ) and weight-related issues( Reference Lillis, Hayes and Bunting 18 , Reference Weineland, Hayes and Dahl 56 ).
Mindfulness skills (FFMQ) and sense of coherence (SOC-13), as well as the general measure of psychological flexibility (AAQ-II), were not found to mediate changes in weight or intuitive eating behaviour. These measures (FFMQ, SOC-13, AAQ-II) are not specific to weight or to eating issues. Thus, this might imply that change processes associated with weight management and eating regulation are better assessed by specific measures targeted to describe weight-related thoughts, feelings and actions. Further, the fact that weight-specific psychological flexibility mediated weight change and intuitive eating might suggest that interventions should target weight-specific behavioural patterns (such as the avoidance of feelings related to weight and body image) and they should include specific exercises or skill training aimed at dealing with weight-related avoidance.
Correspondingly, Webb and Hardin found that body image flexibility, reflecting the willingness to approach aversive body image-related internal content with mindful acceptance in order to continue to move in valued life directions, partially mediated the relationship between adhering to internalized weight-stigmatizing beliefs and the likelihood of practising intuitive eating in a weight-diverse sample of college women( Reference Webb and Hardin 57 ). Body image flexibility has also explained the relationship between self-compassion and intuitive eating( Reference Schoenefeld and Webb 58 ). Together with our results, these findings suggest that the willingness to approach aversive thoughts, emotions and physiological sensations regarding the body with mindful acceptance may have an important role in promoting intuitive eating (i.e. values-driven behaviour).
The promise of mediation analysis is that it can identify fundamental processes underlying human behaviour that are relevant across behaviours and contexts. The present study found similar intervention effects and mediating processes for the ACT mobile stand-alone intervention (minimal contact) as for the ACT face-to-face group intervention, which supports the assumption that these particular behavioural processes are essential in supporting adaptive eating attitudes and weight management. In regard to affecting psychological flexibility and mindfulness skills, these results also suggest that skill training plays a more important role than face-to-face coaching. This hypothesis needs to be tested in future studies.
Limitations
The most significant limitation of the current study is that the processes were measured partly in parallel. Thus, the temporal precedence of the mediator cannot be established, making it difficult to separate cause and effect. Unfortunately, a lack of assessment points during the active treatment phase precluded a detailed examination of the directionality of change. Moreover, the time periods of the present study, about 2 months for the process measurements and 8 months for the outcomes, may have been too short for some mediation effects to take place. For example, adopting mindfulness skills and utilizing them to improve eating behaviours and increase weight loss more significantly may need more time.
Another significant limitation of our study is the use of self-report measures to assess the psychological constructs of interest. Thus, we cannot be sure that observed changes in processes actually reflect ‘true’ changes in target constructs – they may simply reflect social demand or expectations of the treatment. It is also important to note that intuitive eating is a cognitive construct that may be related to eating habits, but more studies are needed to verify that. The present results support this connection by showing similar mediation effects on both BMI and intuitive eating. Still, future studies should aim to include behavioural, experimental and observer-rated processes of acceptance/experiential avoidance and eating behaviour. Also, a variety of approaches have been proposed for the assessment of mindfulness and there have been debates about the issue of measuring this construct( Reference Bishop, Lau and Shapiro 59 , Reference Brown and Ryan 60 ). Thus, further research using other validated measures of mindfulness is recommended.
Moreover, the inclusion of multiple mediation analyses leads to an increased risk of type 1 error. However, AAQW mediated intervention effects systemically on all outcome variables, except for Unconditional Permission to Eat, whereas other process variables (AAQ-II, SOC-13, FFMQ and its subscales) did not have any significant indirect effects. Moreover, it is important to note that the observed effect sizes of the intervention effects as well as the indirect effects were small, and thus the clinical significance of the observations is unclear. Further research is warranted to investigate the effects and mechanisms of ACT-based interventions on eating behaviours. There are possibly also other important variables mediating intervention effects on intuitive eating and weight. Finally, it is important to note that our sample consisted predominantly of overweight women experiencing psychological stress, who were willing to make changes to improve their lifestyle. The participants were also relatively highly educated. Therefore, the generalizability of the results to the other populations must be tested in future studies.
Conclusions
In conclusion, our research provides evidence that ACT-oriented interventions might improve overweight persons’ skills in dealing with emotions related to eating. Our data also imply that weight-related psychological flexibility mediates changes in weight and intuitive eating, especially in eating based on physical reasons and reliance on hunger and satiety cues, in overweight persons experiencing psychological stress. Thus, these findings support the idea that ACT-oriented interventions for lifestyle changes improve individuals’ ability to continue with valued activities even when confronted with negative emotions and thoughts related to weight, and this process mediates changes in eating regulation and weight. More generally, the present results suggest that one way to increase adaptive eating behaviour is to enhance psychological flexibility related to weight issues. Studies are needed to investigate whether interventions targeted to enhance weight-related psychological flexibility lead to better long-term weight maintenance as compared with current weight-loss programmes.
Acknowledgements
Financial support: This study was supported by the SalWe Research Program for Mind and Body (Tekes – the Finnish Funding Agency for Technology and Innovation; grant number 1104/10). Tekes had no role in the design, analysis or writing of this article. Conflict of interest: The authors have no competing interests to declare. Authorship: All authors participated in designing the study, carrying it out and commented on the manuscript. A.T. and E.S. participated in doing statistical analysis. E.S. and R.L. had the main responsibility in writing the article and formulating the research questions. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethics Committee of the Central Finland Health Care District. Written informed consent was obtained from all subjects/patients.








