Autism spectrum disorder (ASD) is characterized by persistent difficulties with social communication as well as restrictive interests and repetitive behaviors; it is currently estimated that 1 in 54 children in the United States are diagnosed with ASD (Maenner et al., Reference Maenner, Shaw and Baio2020). Although polythetic diagnostic criteria for ASD have been established (e.g., American Psychiatric Association, 2013), there is a great deal of variability in the expression and severity of these symptoms, as well as varying concurrent clinical features (e.g., anxiety), across individuals with ASD (Masi et al., Reference Masi, DeMayo, Glozier and Guastella2017). Given this heterogeneity, ASD is often described as a behavioral syndrome that entails multiple underlying causes (Jeste & Geschwind, Reference Jeste and Geschwind2014; Tordjman et al., Reference Tordjman, Cohen, Coulon, Anderson, Botbol, Canitano and Roubertoux2017). This multiple autisms model highlights the variability within the ASD population and has emerged as a useful framework for understanding the multifaceted presentations of the disorder and their possible etiological roots (Hong et al., Reference Hong, Vogelstein, Gozzi, Bernhardt, Yeo, Milham and Di Martino2020). Unfortunately, little research has been conducted to identify phenotypic subgroups with distinct characteristics and underpinnings within the ASD taxon (Masi et al., Reference Masi, DeMayo, Glozier and Guastella2017).
Concurrently, within clinical science, an effort to personalize interventions for individuals based on their presenting profiles, rather than to take a one-size-fits-all approach to treatment allocation, has emerged (e.g., Cheron et al., Reference Cheron, Chiu, Stanick, Stern, Donaldson, Daleiden and Chorpita2019; Weisz et al., Reference Weisz, Chorpita, Palinkas, Schoenwald, Miranda, Bearman, Daleiden, Ugueto, Ho, Martin, Gray, Alleyne, Langer, Southam-Gerow and Gibbons2012; Wood et al., Reference Wood, McLeod, Klebanoff and Brookman-Frazee2015). Potentially, identification of meaningful subgroups of individuals within the ASD taxon may facilitate one means of matching youth with particular treatments. The present study aims to both characterize children with ASD seeking psychotherapy for maladaptive and interfering anxiety in terms of latent subgroup membership within a broad individual differences model, and to test whether these subgroups serve as ex post facto predictors of response to two types of cognitive behavioral therapy (CBT), in the service of informing efforts to personalize treatment for children with ASD.
Heterogeneity in autism spectrum disorder
Autism is described as a spectrum disorder due to the heterogeneity of symptom types and severities that individuals exhibit (Tordjman et al., Reference Tordjman, Cohen, Coulon, Anderson, Botbol, Canitano and Roubertoux2017). This variability is expressed in individuals’ symptom profiles (e.g., ability to change communication to match context, make social inferences, and form meaningful social relationships; rigidity in behavior), verbal and intellectual ability, and comorbid symptoms (Masi et al., Reference Masi, DeMayo, Glozier and Guastella2017). For example, intellectual disability, anxiety disorders, and depressive disorders have an estimated co-occurrence rate of 33%, 42%, and 37% in the ASD population, respectively (Hollocks et al., Reference Hollocks, Lerh, Magiati, Meiser-Stedman and Brugha2019; Maenner et al., Reference Maenner, Shaw and Baio2020). In fact, given this wide range of symptom presentation, the multiple autisms model considers ASD as a broad clinical diagnosis consisting of multiple separable phenotypes (Tordjman et al., Reference Tordjman, Cohen, Coulon, Anderson, Botbol, Canitano and Roubertoux2017).
The multiple autisms model proposes that there are likely to be subgroups of individuals with ASD that vary in biopsychosocial etiology, clinical features, and life trajectory (e.g., Chamak & Bonniau, Reference Chamak and Bonniau2016; Chen et al., Reference Chen, Uddin, Guo, Wang, Wang, Wang, Duan and Chen2019; Kim et al., Reference Kim, Bal, Benrey, Choi, Guthrie, Colombi and Lord2018). While recent reviews have supported this view of ASD, none have been able to specify a definitive set of homogeneous subgroups (Hull et al., Reference Hull, Dokovna, Jacokes, Torgerson, Irimia and Van Horn2017; Masi et al., Reference Masi, DeMayo, Glozier and Guastella2017). Notably, Tordjman and colleagues (Reference Tordjman, Cohen, Coulon, Anderson, Botbol, Canitano and Roubertoux2017; also see Georgiades et al., Reference Georgiades, Szatmari and Boyle2013) asserted that ASD is a behavioral syndrome with unidentified subtypes, emphasizing the research and clinical challenges introduced by its heterogeneous nature. Several others have also highlighted the problem of heterogeneity as a serious impediment in autism research and a concerted effort has been put forth to explore this line of inquiry (Anderson, Reference Anderson2015; Hong et al., Reference Hong, Vogelstein, Gozzi, Bernhardt, Yeo, Milham and Di Martino2020; Lombardo et al., Reference Lombardo, Lai and Baron-Cohen2019).
Identifying phenotypic subgroups using an individual differences framework
Clinical subgroups can be discerned at the phenotypic level by employing multivariate methods to identify classes of individuals with similar overall profiles across a range of dispositional traits (e.g., Klopper et al., Reference Klopper, Testa, Pantelis and Skafidas2017; Patrick & Drislane, Reference Patrick and Drislane2015; Zablotsky et al., Reference Zablotsky, Bramlett, Visser, Danielson and Blumberg2018). The literature has shown that dispositional (personality) traits (a) are the product of genetic predispositions and environmental influences (Briley & Tucker-Drob, Reference Briley and Tucker-Drob2014), (b) can explain both adaptive and maladaptive thoughts and behaviors (Krueger et al., Reference Krueger, Watson and Widiger2020), and (c) remain relatively stable (Borghuis et al., Reference Borghuis, Denissen, Oberski, Sijtsma, Meeus, Branje, Koot and Bleidorn2017). Analyzing patterns of trait variability within a diagnostic group can identify clinically meaningful subgroups, which may represent taxa with differential etiologies and life trajectories, as has been found in the psychopathy literature (i.e., fearless vs. disinhibited subtypes; Patrick & Drislane, Reference Patrick and Drislane2015; Patrick et al., Reference Patrick, Fowles and Krueger2009). This approach also seems promising in identifying subgroups within the ASD taxon, a syndrome with comparable phenotypic heterogeneity, clinical severity, and developmental complexity in comparison to psychopathy.
A comprehensive and inductive approach to human individual differences is the five-factor model of personality (FFM; Costa & McCrae, Reference Costa and McCrae1992). The FFM has been considered a useful framework for clinical research because it was derived empirically from the lexicon and therefore, is agnostic to diagnostic classification and stratification. This framework captures a comprehensive array of meaningful human trait variability (e.g., including both adaptive and maladaptive personality traits; DeYoung et al., Reference DeYoung, Carey, Krueger and Ross2016) and has been used to elucidate the risk factors, etiology, symptoms, prognosis, and treatment outcomes across disorders (Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby, Brown, Carpenter, Caspi, Clark, Eaton, Forbes, Forbush, Goldberg, Hasin, Hyman, Ivanova, Lynam, Markon and Eaton2017; Lengel et al., Reference Lengel, Helle, DeShong, Meyer and Mullins-Sweatt2016).
The core symptoms of ASD, as well as common comorbid symptoms, may be partially explained by patterns of individual differences. Past studies suggest that there is a strong relationship between FFM traits and manifestations of ASD symptoms (Lodi-Smith et al., Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019; Vuijk et al., Reference Vuijk, Deen, Sizoo and Arntz2018). A recent meta-analysis by Lodi-Smith and colleagues (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) synthesized 14 FFM studies in the ASD literature, finding negative links between ASD symptom severity and all five FFM factors, with the largest effect sizes for Extraversion, Agreeableness and Emotional Stability (i.e., the inverse of Neuroticism; Fisher-z corrected correlations ranged from −.36 to −.50 for these three factors). These three FFM factors are conceptually related to social motivation, perspective-taking and empathy, and negative affect sensitivity, manifestations of which have been empirically linked with ASD and are viewed as causal or interrelated processes in the psychopathology of ASD in some models (Clements et al., Reference Clements, Zoltowski, Yankowitz, Yerys, Schultz and Herrington2018; Harmsen, Reference Harmsen2019; Hollocks et al., Reference Hollocks, Lerh, Magiati, Meiser-Stedman and Brugha2019).
However, of the individual difference studies in ASD to date, only one study aimed to identify subgroups within the ASD taxon. This study (Schwartzman et al., Reference Schwartzman, Wood and Kapp2016) found that FFM facets accounted for 70% of the variance in autism trait scores among adults with and without ASD. Four distinct subgroups of adults with ASD were identified via cluster analysis based on their FFM facet profiles (e.g., one group had average Neuroticism and Conscientiousness facet scores, but low Extraversion and Agreeableness facet scores; another group had low scores in each of these areas). The personality profiles of these four subgroups were characterized clinically as shy/aloof (having notable features of Neuroticism and introversion), dysregulated/uncongenial (heightened Neuroticism and introversion and low Conscientiousness and Agreeableness), isolated/disaffected (high introversion plus certain self-centered components of low Agreeableness), and normative, respectively. These groups differed from each other on several demographic and criterion variables (e.g., life satisfaction), suggesting that clinically meaningful subgroups might be identified among those with ASD. It is unknown if these subgroups are replicable and have distinctive etiologies or differential future life trajectories. However, following the promising precedent set in the psychopathy literature for this approach to identifying more phenotypically homogeneous groups with unique underlying determinants and profiles of risk and resilience, identifying meaningful phenotypic subgroups could be an important step in developing informed hypotheses about separable etiologies of varying subtypes of ASD as well as personalized interventions for individuals with ASD.
Predicting treatment response
Subgroups are particularly meaningful when they confer predictive value, describing individuals not just at a specific point in time but also foreshadowing future outcomes and probable responses to varying contexts (as well as contributing to hypotheses about potential differential etiologies). A distinguishing feature in the psychopathy literature is the essentially opposite quality of the fearless and disinhibited pathways to psychopathy on the trait of Neuroticism, with correspondingly different neurobiological responses (e.g., differing levels of sympathetic nervous system arousal), with each pathway nonetheless embedded within a single clinical taxon featuring specific behavioral and psychological extremes (e.g., callousness, aggression, disavowal of societal norms, lack of emotional empathy) (Patrick & Drislane, Reference Patrick and Drislane2015; Patrick et al., Reference Patrick, Fowles and Krueger2009). However, equally notable is the differing life trajectories associated with these two psychopathy pathways (e.g., risk of substance abuse, suicidality, criminal recidivism, social attachment styles, etc.) (Anestis et al., Reference Anestis, Anestis and Preston2018; Baños et al., Reference Baños, Álvarez, Martín, Lorca, Jiménez and Trives2019; Christian et al., Reference Christian, Sellbom and Wilkinson2017; Coffey et al., Reference Coffey, Cox and Kopkin2018). There have also been some indications of possible differential response to parent management approaches among children with differing psychopathy risk profiles (e.g., relatively fearless vs. disinhibited children; Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020). While little has been studied with regard to individual difference profiles and response to structured psychological treatments, it is plausible that individuals in meaningful subgroups within a clinical taxon might respond substantially differently to varying forms of treatment.
Prediction of treatment response in the context of a randomized controlled trial (RCT) is one potentially meaningful indicator of the predictive validity of subgroups derived from individual difference variables (e.g., Mann et al., Reference Mann, Roos, Hoffmann, Nakovics, Leménager, Heinz and Witkiewitz2018). An advantage of the RCT setting is that it entails experimental control of varying contexts that are easily characterized (e.g., the differences among active treatments are known and verified in modern RCTs) and of comparable duration (e.g., psychological treatments are often several months in duration), leading to high internal validity for the purpose of initially exploring differential trajectories among subgroups. Additionally, the capacity to predict “who will respond best to which treatment” is a long-standing goal in treatment research (Vivanti et al., Reference Vivanti, Prior, Williams and Dissanayake2014; Yoder & Compton, Reference Yoder and Compton2004). Thus, prediction of treatment outcome might help probe the construct validity of empirically identified subgroups while at the same time serving as a practical contribution to advancing the personalization of care.
In the present study, we sought to empirically identify subgroups of children with ASD, paralleling the general approach taken by Schwartzman and colleagues (Reference Schwartzman, Wood and Kapp2016) to use individual differences within the FFM to discern phenotypically distinct subgroups; we then utilized these subgroup classifications to evaluate potential differences in treatment response to two types of CBT for anxiety (Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020). In light of Schwartzman and colleagues’ findings, we hypothesized that a similar number of subgroups (around four) would emerge through empirically driven classification analyses, and that they would have similar FFM characteristics to the subgroups discerned within the Schwartzman and colleagues’ study (as described above; e.g., shy/aloof). However, given the commonality of anxiety symptoms amongst the participants in this sample, we expected all subgroups would exhibit elevated indications of Neuroticism.
In the Wood and colleagues (Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020) RCT (N=167), one type of CBT treatment (BIACA; see Method below) was adapted for the characteristics of ASD, and the other was the standard-of-practice CBT treatment (Coping Cat) developed for the general population of children with anxiety disorders. While the primary outcomes in the RCT revealed that BIACA was relatively more beneficial to youth with ASD in reducing anxiety and related impairment, both types of CBT yielded high overall treatment response. Furthermore, the study did not consider the possibility of differential subgroup response.
In forming hypotheses about differential treatment response to the two CBT treatments in the Wood et al. (Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020) RCT, we assumed that subgroups characterized by low Conscientiousness, low Agreeableness, and low Extraversion (e.g., the dysregulated/uncongenial subgroup identified in Schwartzman et al., Reference Schwartzman, Wood and Kapp2016) would likely benefit most from BIACA, which has a modular approach that can more comprehensively address ASD-related challenges that may interfere with CBT treatment for anxiety. Namely, low Conscientiousness is associated with cognitive inflexibility and emotion dysregulation (Fleming et al., Reference Fleming, Heintzelman and Bartholow2016; Pocnet et al., Reference Pocnet, Dupuis, Congard and Jopp2017), and together with low Agreeableness (and low Neuroticism), is associated with externalizing characteristics (Tackett & Mullins-Sweatt, Reference Tackett, Mullins-Sweatt, John and Robins2021). Additionally, low Extraversion is associated with inhibited social and non-social reward processing (DeYoung, Reference DeYoung2015; Smillie, Reference Smillie2013). BIACA’s components of antecedent and incentive-based practices to reduce influence of aggression and noncompliance on treatment engagement, as well as its individualized reward system (based on participants’ specialized interests), are able to address these comorbid characteristics concurrently with the participants’ anxiety. On the other hand, Coping Cat was designed for youth in the general population with anxiety disorders. As such, we postulated that the more child-focused Coping Cat (which has shorter sessions and less emphasis on parent training or symptoms outside of the anxiety domain) might be a relatively better fit for children with most FFM traits (except Neuroticism) closer to the population average (e.g., the normative subgroup identified in Schwartzman et al., Reference Schwartzman, Wood and Kapp2016).
Method
Participants
The current study used data from a three-site RCT which concluded in 2017 (Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020; ClinicalTrials.gov identifier: NCT02028247). De-identified participant data, data dictionary, and variables of the main study are available through the National Database of Autism Research (NDAR; https://nda.nih.gov/edit_collection.html?id=2076). The study compared an adapted CBT treatment (BIACA) designed for children with ASD and maladaptive and interfering anxiety to a standard-of-practice CBT treatment (Coping Cat) and to treatment-as-usual (TAU). The study screened 214 children (ages 7 to 13 years old) with ASD from three major US metropolitan areas (Los Angeles, CA; Tampa, FL; Philadelphia, PA). Eligibility criteria included (a) a diagnosis of ASD (confirmed by the Autism Diagnosis Observation Schedule-Second Edition [ADOS-2; Lord et al., Reference Lord, Rutter, DiLavore, Risi, Gotham and Bishop2012] and Childhood Autism Rating Scale, Second Edition-High Functioning Version [CARS2-HF; Schopler et al., Reference Schopler, Van Bourgondien, Wellman and Love2010]), (b) maladaptive and interfering anxiety (i.e., a severity score greater or equal to 14 on the Pediatric Anxiety Rating Scale [PARS; Research Units on Pediatric Psychopharmacology Anxiety Study Group (RUPP), 2002; see below]), (c) estimated full-scale intelligence quotient>70, computed from the Vocabulary and Matrix Reasoning subscales in the Wechsler Intelligence Scale for Children-Fourth Edition (Wechsler, Reference Wechsler2003). For a comprehensive summary of the screening process, see Wood and colleagues (Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020).
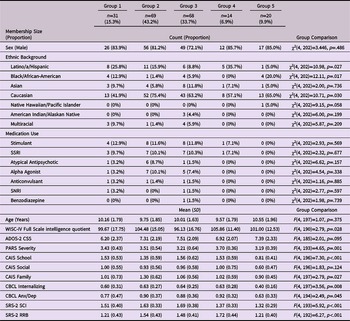
eTable 1 presents descriptive and diagnostic information for the sample. Of the 214 children that were screened, 202 had sufficient FFM data for the initial latent profile analyses. Of these 202 participants, 161 were assigned to a CBT treatment condition (BIACA, n=74; CC, n=70; TAU, n=17; note that there were six participants assigned to a CBT treatment condition but did not have FFM data). The TAU group was not included in the prediction of treatment outcome analyses since TAU interventions were highly heterogeneous.
Treatment conditions
Eligible children were randomized to receive either standard-of-practice CBT (Coping Cat [CC]; Kendall & Hedtke, Reference Kendall and Hedtke2006), adapted CBT (Behavioral Interventions for Anxiety in Children with Autism [BIACA]; Wood & Wood, Reference Wood and Wood2013), or TAU. The computer-generated randomization procedure stratified on treatment site, verbal intelligence quotient (≥90 vs. <90), and ADOS-2 score. The two CBT conditions are described briefly here; for greater detail, see Wood and colleagues (Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020).
Standard-of-practice CBT (CC)
In the standard-of-practice CBT condition, the participants met with a trained therapist for 16 weekly 60-minute therapy sessions (Kendall & Hedtke, Reference Kendall and Hedtke2006), which represents a well-established CBT approach for treating anxiety disorders in the general population of children (Lenz, Reference Lenz2015). The main features include emotion recognition, identifying anxious cognition and using corresponding coping strategies such as reappraisal, exposure tasks, and self-reinforcement. Therapists employ modeling, role-play, contingent reinforcement, and use of homework assignments. Parent involvement includes a regular 15-minute check-in at the start of each session and two meetings with the therapist.
Adapted CBT (BIACA)
In the adapted CBT condition, participants had 16 weekly 90-minute therapy sessions split evenly between children and their parents (Wood & Wood, Reference Wood and Wood2013). The intervention program is a compendium of evidence-based practices for school-aged youth with ASD and utilizes a personalized, modular format to address anxiety, dysregulated behavior, and core autism symptoms. In this intervention, the therapist and family work together to encourage the participant to face fears and use pro-social behaviors across settings (e.g., home, school, community). Key evidence-based behavioral practices in BIACA include exposure therapy, positive reinforcement with a comprehensive incentive system, antecedent management, and friendship skills training. Concepts are taught via multimodal stimuli (e.g., telling stories, drawing cartoons) and guided Socratic questioning.
Measures
Parents and children participated in assessments prior to randomization and at the end of treatment. Assessments took approximately three hours and were carried out by independent evaluators (IEs). IEs and families were unaware of study hypotheses; IEs were also unaware of participants’ treatment condition. Measures relevant to the current study are described in detail below.
Hierarchical Personality Inventory for Children (HiPIC)
The HiPIC (Mervielde & De Fruyt, Reference Mervielde, De Fruyt, Mervielde, Deary, De Fruyt and Ostendorf1999) is a parent-report measure based on the FFM. The HiPIC was conducted during the screening assessment. The HiPIC is comprised of 144 items grouped into 18 facets, hierarchically organized under the five FFM higher-order factors. Parents are instructed to indicate the degree to which each statement has characterized their child’s behavior over the past year. A 5-point Likert-type scale was used, ranging from barely characteristic (1) to highly characteristic (5). The five factor names in the HiPIC differ slightly from the FFM standard terminology due to the focus on a youth target population. In the HiPIC, the Benevolence factor represents the FFM construct of Agreeableness; the Imagination factor represents the FFM construct of Openness to Experience; and the Emotional Stability factor represents the inverse of the Neuroticism FFM construct. There was no change in terminology for the HiPIC factors representing FFM Extraversion or Conscientiousness.
The HiPIC has demonstrated a robust factor structure and high internal consistency across various studies, including in clinical samples (De Clercq & De Fruyt, Reference De Clercq and De Fruyt2012; Decuyper et al., Reference Decuyper, Colins, De Clercq, Vermeiren, Broekaert, Bijttebier, Roose and De Fruyt2013; Hampson et al., Reference Hampson, Vollrath and Júlíusson2015; Miers et al., Reference Miers, Blöte, De Rooij, Bokhorst and Westenberg2013). Following Schwartzman and colleagues (Reference Schwartzman, Wood and Kapp2016), in the present study, the 18 HiPIC facets were used to identify latent personality subgroups within the sample. Cronbach’s alpha values for these facets ranged from .729 (Concentration) to .904 (Altruism). Using the data of a large sample of Flemish children provided by the HiPIC authors, raw scores on the HiPIC scales were converted into gender and age-normed decile scores to permit characterization as high, normative, low, etc. (see below).
Primary and secondary treatment outcome measures
The PARS is an IE-rated measure used to assess child anxiety symptom severity (RUPP, 2002). In this RCT, it served as the primary outcome measure, exhibited sensitivity to treatment, and was only administered to the parents (Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020). IEs make ratings on seven dimensions (e.g., severity of distress associated with anxiety symptoms) using a 0-5 severity scale (0 for none, 1-5 for minimal to extreme) and the mean of these ratings served as the summary score for the PARS. The PARS has strong psychometric properties (RUPP, 2002), including among children with ASD (Storch et al., Reference Storch, Wood, Ehrenreich-may, Jones, Park, Lewin and Murphy2012).
The Child Anxiety Impact Scale (CAIS; Langley et al., Reference Langley, Falk, Peris, Wiley, Kendall, Ginsburg, Birmaher, March, Albano and Piacentini2014), Child Behavior Checklist (CBCL; Achenbach & Rescorla, Reference Achenbach and Rescorla2001), Social Responsiveness Scale-2 (SRS-2; Constantino & Gruber, Reference Constantino and Gruber2012), and Clinical Global Impressions-Improvement Scale (CGI-I; Guy, Reference Guy1976) served as secondary outcome measures, which demonstrated sensitivity to treatment in this RCT (Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020). The CAIS, CBCL, and SRS-2 were completed by parents pre- and post-treatment; higher scores are indicative of more impairment/symptoms. The primary RCT utilized all three CAIS subscales (School, Social, Family), two CBCL subscales (Internalizing, Anxiety/Depression), and the two Diagnostic and Statistical Manual of Mental Disorders (5th edition) oriented SRS-2 scales (Social Communication and Interaction, Restricted Interests and Repetitive Behavior). The CGI-I was administered by an IE at post-treatment and was a measure of treatment response. Interrater reliability for the PARS and CGI-I in this sample were acceptable (see Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020).
Data analyses
Latent profile analysis
The first research aim was to identify possible subgroups in school-aged children with ASD based on FFM profiles. To do so, a latent profile analysis (LPA) of HiPIC facet scores was conducted using Mplus 8 (Muthén & Muthén, Reference Muthén and Muthén2017). LPA is a form of finite mixture modeling that identifies latent subgroups based on patterns of continuously distributed scores within the sample. This statistical method employs an iterative maximum likelihood estimation approach, which attempts to determine a best-fitting model through parameter estimations that minimize the deviance between observed and model-estimated values. It has been used to identify subgroups in various clinical taxa, including social anxiety disorder (Peyre et al., Reference Peyre, Hoertel, Rivollier, Landman, McMahon, Chevance, Lemogne, Delorme, Blanco and Limosin2016), postpartum depression (PACT Consortium, 2015), posttraumatic stress disorder (Galatzer-Levy et al., Reference Galatzer-Levy, Nickerson, Litz and Marmar2013), and schizophrenia (Tsai & Rosenheck, Reference Tsai and Rosenheck2013).
Established decision rules were used to determine the best fitting model (Masyn, Reference Masyn and Little2013). Analysis included both inferential (e.g., likelihood ratio tests) and information-heuristic (e.g., information criterion values) relative fit comparisons. Based on the extant statistical literature, the Bayesian Information Criterion (BIC; Schwarz, Reference Schwarz1978), sample-size adjusted BIC (SBIC; Sclove, Reference Sclove1987), and the bootstrapped likelihood ratio test (BLRT; McLachlan & Peel, Reference McLachlan, Peel, McLachlan and Peel2000) were selected as the most reliable indicators of model fit (Chen et al., Reference Chen, Luo, Palardy, Glaman and McEnturff2017; Tein et al., Reference Tein, Coxe and Cham2013); however, the Akaike Information Criterion (AIC; Akaike, Reference Akaike1973) was also provided for completeness. To aid interpretability of the extracted latent profiles, HiPIC normed decile scores were translated into simplified descriptive categories: a decile score of 1-2 (i.e., those whose scores are at or below the 20th percentile) was labeled “very low,” 2.001-3.2 as “low,” 3.201-7.799 as “normative,” 7.8-8.999 as “high,” and 9-10 as “very high” (i.e., those whose scores are between the 80th and the 100th percentiles). These ranges were chosen to resemble commonly used clusters of scores on a normal curve (e.g., > 1 SD) but with a somewhat narrower “normative” range in order to also highlight children with slightly higher or lower scores than the normative sample mean that are still within ±1 standard deviation of the mean, for descriptive purposes. Within a FFM construct, some facets represent one end of the continuum (e.g., Anxiety is reflective of high Neuroticism) and some represent the other end (e.g., Self-Confidence is the inverse of Neuroticism); in all cases, the decile scores and simplified descriptive categories reflect comparisons with the normed sample at the facet level (e.g., “high” Anxiety = high Neuroticism whereas “high” Self-Confidence = low Neuroticism). LPA subgroups were preliminarily labeled based on distinctions in personality profiles and framed in contrast to the average personality profile of the ASD population as identified in Lodi-Smith and colleagues’ (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) meta-analysis (high Neuroticism, low Extraversion, low Agreeableness, low Conscientiousness, low Openness to Experience). However, it should be noted that these names only partially capture the full profile of individual differences expressed by each subgroup, and as such, the subgroups will be primarily referred to numerically (e.g., Group 1) in this paper.
In order to ascertain the predictive power of the empirically identified subgroups versus continuous trait scores, we conducted a preliminary analysis featuring parallel sets of hierarchical multiple regression models with post-treatment measure scores as outcome variables. Specifically, the outcome measures were regressed on the identified subgroups and continuous personality factor scores, respectively, to compare the two models. In both models, stage 1 included pre-treatment score and treatment condition (CC [0] vs BIACA [1]) as predictors. In the subgroups model, stage 2 included the identified personality subgroups (dummy-coded as binary categorical variables) while stage 3 included their interaction terms with treatment condition. In the factor scores model, stage 2 included all five continuous factor scores simultaneously, while stage 3 included their interaction terms with treatment condition.
Analysis of covariance (ANCOVA) and logistic regression models
A two-way factorial ANCOVA model was employed to investigate main effects of LPA-based subgroups, treatment condition, and their interaction, on the post-treatment outcomes reported in Wood and colleagues (Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020). Pre-treatment scores served as covariates in the models. Additionally, a binary logistic regression model with an analogous design was conducted for CGI-I outcomes (response vs. no response) at post-treatment (i.e., CGI-I was regressed on subgroup, treatment condition, and their interaction term, in which Group 1 within the CC condition served as the reference group) Footnote 1 . It should be noted that in the original study (Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020), participants in the TAU condition continued their usual services and no specific treatment recommendations were given (i.e., they were not assigned CBT). Given this study’s goal to evaluate the predictive validity of personality subgroups on CBT treatment response, the present analyses only included participants in the CC and BIACA treatment conditions. However, for the sake of completeness, these same analyses (but also including the TAU participants) are reported as well (see Appendix A in Online Supplement).
For models that yielded a statistically significant main effect for subgroup or interaction between subgroup and CBT treatment condition, contrasts were conducted to probe the nature of the findings. Main effect contrasts compared outcome measures between subgroups regardless of treatment condition and simple contrasts compared outcome measures between subgroups within each treatment condition. The simple contrasts tested were guided by inspection of the outcome measures’ estimated marginal means (EMMs) for each treatment condition-by-subgroup cell. It should be noted that all analysis scripts are publicly available (https://osf.io/qzesn/?view_only=27299e97a8b54596a71c40c606ae457d).
Results
Descriptive statistics for the HiPIC scores for the overall sample, as well as the two CBT treatment groups, are provided in eTable 2. Note that descriptive statistics for outcome measures at pre- and post-treatment are provided in Wood and colleagues (Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020); specific descriptive statistics for these measures in relation to the LPA-based subgroups are presented below.
Identifying subgroups of children with ASD using the FFM
Latent profile analysis
A LPA of the participants’ HiPIC facet decile scores is summarized in Table 1. Each model was processed with 200 initial stage random starts and 50 final stage optimizations to ensure that a global maximum log likelihood value was obtained and replicated. Results indicate that a five-class solution best fit the data with significant reductions in the BIC and SBIC through five classes. In comparison, the six-class solution demonstrated a moderate increase in the BIC and a marginal decrease in the SBIC. Similarly, the BLRT was significant (p<0.001) up to the five-class solution, while the test was nonsignificant for the six-class solution (p=0.208). Entropy value for the five-class solution (.940) suggests high classification accuracy. Specifically, 88.12% of participants had a posterior probability of over 90% for a single class and only nine participants did not have at least 70% for their assigned class. Mean posterior probability for the five classes were 96%, 97%, 95%, 98%, and 98%, respectively.
Table 1. Model Fit Indices for One- to Seven-class Solutions in the Latent Profile Analysis using HiPIC Facet Decile Scores
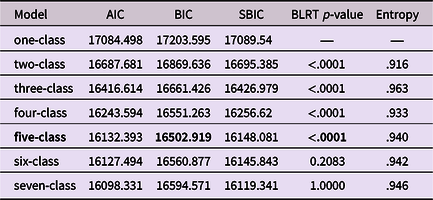
Note. HiPIC = Hierarchical Personality Inventory for Children. AIC = Akaike Information Criterion, BIC = Bayesian Information Criterion, SBIC = Sample-size adjusted Bayesian Information Criterion, BLRT = Bootstrapped Likelihood Ratio Test.
Class (subgroup) characteristics
Table 2 presents the subgroups’ demographic and clinical characteristics (e.g., pre-treatment scores), and Table 3 summarizes each subgroup’s Ms, SDs, and interdecile ranges for the HiPIC decile scores (qualitative descriptions of the subgroups’ FFM facet profiles, as described in the Method section, are provided in Table 4). Group 1 included about 15% of the sample; Groups 2 and 3 each included over a third of the sample; and Groups 4 and 5 each included less than 10% of the sample. General trends across subgroups are described first (for efficiency, subgroups are referred to as a singular entity and the term “average score” is omitted but implied). Then, the subgroups’ unique attributes and descriptive labels are provided.
Table 2. Demographics and Clinical Pre-treatment Scores for Identified Personality Subgroups
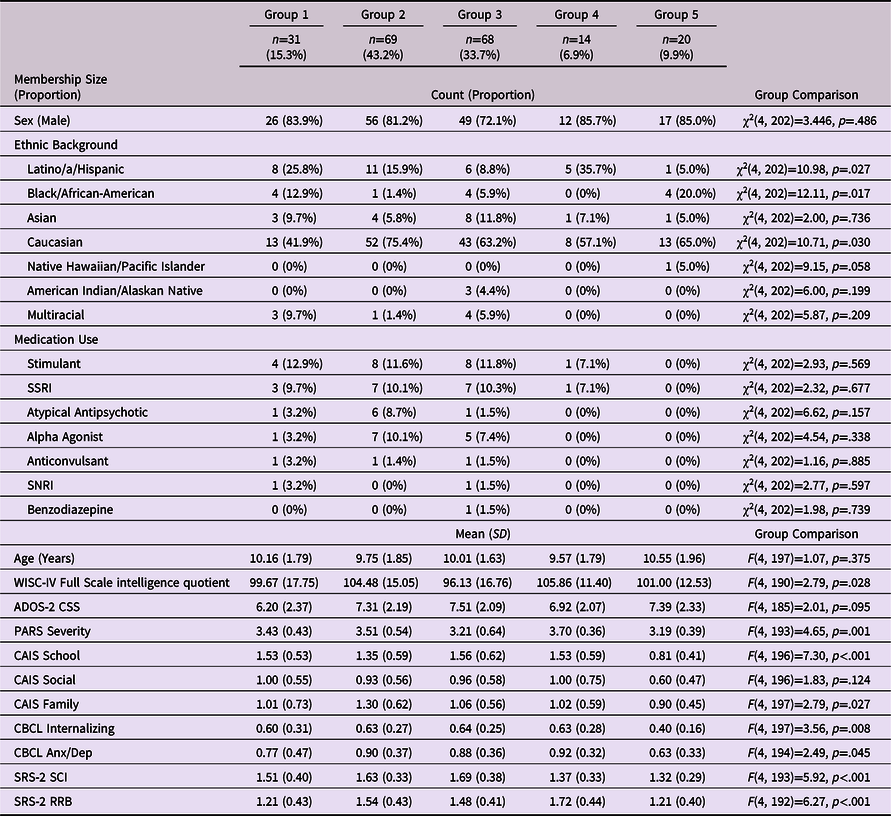
Note. SSRI = selective serotonin reuptake inhibitor, SNRI = serotonin-norepinephrine reuptake inhibitor, WISC-IV = Wechsler Intelligence Scale for Children-Fourth Edition, ADOS-2 CSS = Autism Diagnostic Observation Schedule-2 Calibrated Severity Score, PARS = Pediatric Anxiety Rating Scale, CAIS = Child Anxiety Impact Scale, CBCL = Child Behavior Checklist, Anx/Dep = Anxious/Depressed, SRS-2 = Social Responsiveness Scale-2.
*Of the 214 participants in the original data set, 12 cases were missing HiPIC data and excluded from the present study’s analyses.
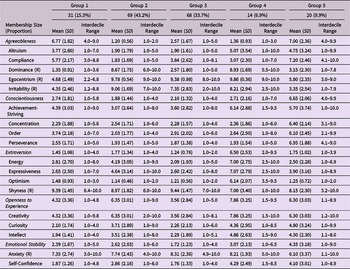
Table 3. HiPIC Facet Decile Scores for Identified Personality Subgroups
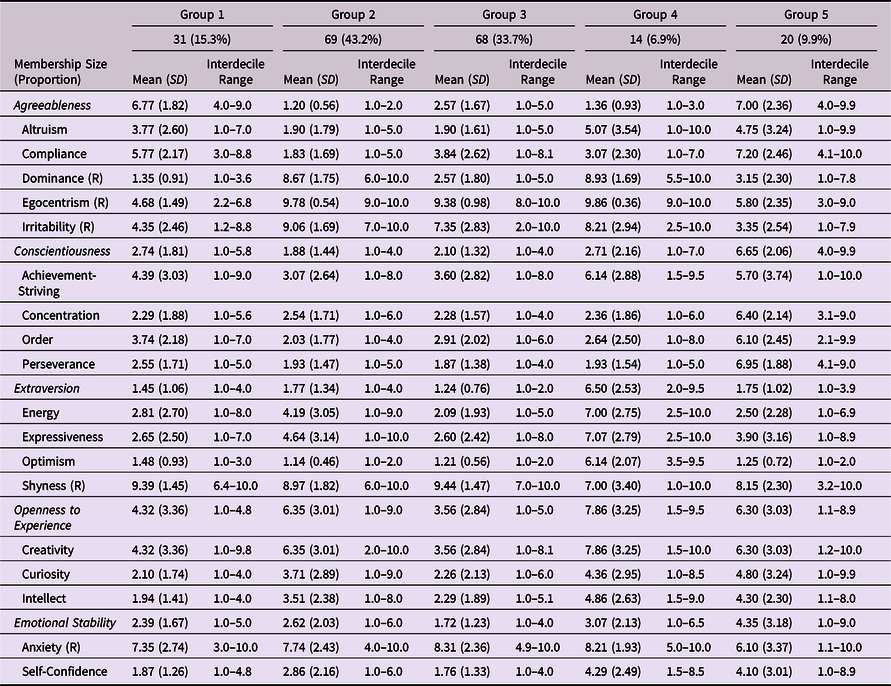
Note. (R) indicates the facet is reverse-scored for its respective FFM factor. HiPIC = Hierarchical Personality Inventory for Children.
Table 4. HiPIC Facet Profiles for Identified Personality Subgroups
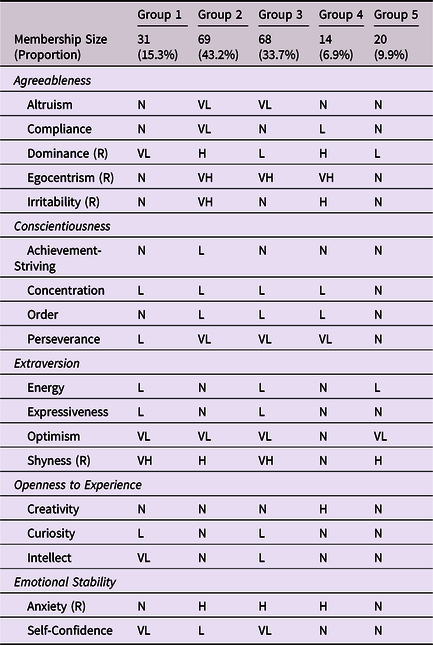
Note. Rankings are according to a simple classification system based on the subgroups’ raw decile scores, in comparison to a normative Flemish youth population. (R) indicates the facet is reverse-scored for its respective FFM factor. HiPIC = Hierarchical Personality Inventory for Children. VL = very low (1-2), L = low (2.001-3.2), N = normative (3.201-7.799), H = high (7.8-8.999), VH = very high (9-10).
One notable feature of the five subgroups is that none scored in the high or very high range (see HiPIC in Method, above, for details of these descriptive range categories) on any facet indexing Extraversion (note that the high and very high average scores on the Shyness facet of Extraversion represents the opposite of Extraversion; see Table 4). Very low to normative-range Extraversion seems to be a consistent characteristic of this entire sample, with a particular trend for very low Optimism in four of the subgroups. A second meaningful feature of the subgroup scores is that in spite of the commonality of experiencing maladaptive and interfering acute anxiety in one or more domains (i.e., the study recruitment emphasis), the two HiPIC Neuroticism facets, Anxiety and Self-Confidence, were not consistently indicative of very high trait anxiety across subgroups (and, as with Extraversion, no subgroup scored high or very high in the direction of Emotional Stability [the opposite of Neuroticism] on either facet, either). Third, a similar trend was seen with Conscientiousness facets; no subgroup scored high or very high on any facet within this construct, but three of the subgroups scored very low on a particular facet of Conscientiousness: Perseverance. Fourth, the Agreeableness construct exhibited the greatest variability of the five FFM constructs, with, for example, three of the subgroups scoring low or very low on a facet, Dominance, that represents the inverse of Agreeableness (i.e., they scored high or very high on Agreeableness in this domain), whereas the other two subgroups scored high on this facet (i.e., they were low on Agreeableness in this domain). Agreeableness also had the greatest proportion of extreme facet scores (i.e., very low or very high; 32%). Agreeableness captured both substantial between-subgroup variability and within-subgroup variability (e.g., Group 3, n=68, had low Dominance [i.e., a score indicative of high Agreeableness], normative Compliance and Irritability [i.e., scores indicative of average Agreeableness], but also very low Altruism and very high Egocentrism [i.e., scores indicative of very low Agreeableness]).
Whereas a common pattern for many of the participants was constrained positive affect and sociability, and a tendency towards experiencing or expressing negative affect, the subgroups varied considerably from one another on these and other overarching trait themes. The subgroups’ uniqueness and provisional descriptive labels are provided below, focusing primarily on how the groups differ from one another and also the general ASD population profile identified in Lodi-Smith and colleagues’ (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) meta-analysis. Due to the complexity of the findings for five subgroups derived from multiple FFM facets, interpretive links to the personality literature are offered in the following subgroup descriptions to aide conceptualization; a broader consideration of subgroup patterns is then provided in the Discussion section.
Group 1
Group 1 presented with a reserved and reluctant personality profile, highlighted by key elevations on trait indicators of shyness and social passivity including Shyness (very high) and Self-Confidence (very low), as well as Dominance (very low). Notably, this subgroup had normative Anxiety scores; perhaps the children’s clinically impairing negative affect was mainly comprised of social reticence and poor self-appraisals. It is also important to recall that very low Dominance is a trait indicator of very high Agreeableness, even if that trait also implies passivity and peripheral status in some social situations. In models of personality, Extraversion and Openness to Experience have been described as indicators of plasticity and the capacity for exploration and appetite for novelty (of experiences and ideas, respectively; Feist, Reference Feist2019); the consistently low and very low facet indicators in these two factors are suggestive of a preference for sameness (and, relatedly, reluctance to explore unknown circumstances and resistance to change). Relative to the general personality profile exhibited in the ASD population as found by Lodi-Smith and colleagues (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) (high Neuroticism, low Extraversion, low Agreeableness, low Conscientiousness, and low Openness to Experience), Group 1 can be distinctly characterized as having generally normative Agreeableness and Neuroticism.
Group 2
Group 2, the largest subgroup of the five, was distinguished by multiple trait indicators of very low Agreeableness (e.g., very low Altruism and Compliance, very high Egocentrism and Irritability) – the most of all of the subgroups. Relatedly, traits of Conscientiousness were uniformly low, with Perseverance rated as very low in this subgroup. Agreeableness and Conscientiousness are sometimes viewed as complementary personality expressions of underlying emotion regulation capacity (the former around the social interaction arena, and the latter around the less-social arenas of life such as schoolwork; Eldesouky & English, Reference Eldesouky and English2019). The constellation of low Agreeableness and Conscientiousness facets suggest a dysregulated and socially antagonistic disposition that is likely to feature externalizing behavior (Tackett & Mullins-Sweatt, Reference Tackett, Mullins-Sweatt, John and Robins2021). However, Group 2 is also characterized by its normative-range traits of Openness to Experience (e.g., Curiosity). In fact, this serves as the defining trait for this subgroup in contrast to Lodi-Smith and colleagues’ (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) prototypical ASD personality profile, thus yielded a distinct subgroup characterization as normative Openness to Experience, highlighting a potential personality-based strength for this subgroup. Together with low Agreeableness, Openness to Experience can include a tendency towards nonconformity and the ability to challenge or defy unfair systems and authority figures (vs. agreeably complying with them; McAdams, Reference McAdams2015). Of course, the very high Egocentrism and very low Altruism characterizing this subgroup may serve as a barrier to forming social bonds, but transgressive figures can be catalysts for change, as well (i.e., positive noncompliance; Tsai, Reference Tsai2015).
Group 3
Group 3 shared numerous characteristics with Group 2 and was nearly the same size, but exhibited unique features including a less antagonistic profile of traits related to Agreeableness; negative emotion more focused on the self than against others; and a more introverted (low energy, less exploratory) set of traits. The most distinctive feature of Group 3 is its very high Egocentrism and very low Altruism (two facet indicators of very low Agreeableness) in conjunction with low Dominance (i.e., indicating high Agreeableness) and normative-range Compliance and Irritability (also facets of Agreeableness). As a quintet, these facets of Agreeableness paint a mosaic of self-centeredness (and lack of awareness/responsiveness to others’ mental states) otherwise devoid of the hostile and transgressive characteristics of Group 2. As with Group 1, there is a combination of very high Shyness and very low Self-Confidence (as well as high Anxiety), that, in combination with the low Extraversion facets, is reflective of notable social reticence/anxiety (e.g., low social motivation in conjunction with low self-worth and a fear of rejection). However, as is often noted in personality literature, the pragmatic value of anxiety proneness can be sensible judgment, that is, the awareness of the risks and realities of everyday life and the wherewithal to make practical decisions to achieve acceptable (if not always exciting) outcomes (e.g., DeYoung, Reference DeYoung2015). As with Group 2, facets of Conscientiousness, especially Perseverance, were low, indicating challenges with organization and goal persistence in non-preferred situations. Notably, the primarily low to very low scores across the facets (or high to very high scores for reverse-scored facets) generally resemble the average personality profile found in the ASD population (Lodi-Smith et al., Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019).
Group 4
The smallest subgroup was Group 4, but it was distinct from the others in many ways, the most notable of which was its normative levels of Extraversion across all four facets. Like Groups 2 and 3, this subgroup was characterized by very high Egocentrism (from the Agreeableness construct) and very low Perseverance (as well two other indicators of low Conscientiousness). Some other indicators of low Agreeableness were also characteristic of Group 4 (similar in some ways to Group 2 but less pronounced; e.g., Altruism was in the normative range). Anxiety was high, but not very high, and Creativity was also high (in the context of normative range additional facets related to Openness to Experience). In comparison to the Lodi-Smith and colleagues (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) average personality profile, this FFM facet profile – while relatively rare in this sample – is distinguished by normative Extraversion and above-average Creativity.
Group 5
The fifth subgroup was also a relatively small subset of the entire sample and was only characterized by only one very low facet score (Optimism, an indicator of Extraversion). In general, other facets in the Extraversion factor trended towards introversion and shyness, as well. Group 5 otherwise exhibited normative scores in other FFM areas, with a low score in Dominance serving, as in two other subgroups, as an indicator of social passivity as well as (in parallel) above-average Agreeableness. It is notable that in a sample of children with comorbid anxiety, both facets of Neuroticism were in the normative range for Group 5. Relative to the Lodi-Smith and colleagues’ (Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) personality profile, only Extraversion scores were comparable, whereas Group 5 had normative-range scores on facets representing the remaining four factors. Overall, this subgroup could be described as having a normative personality profile that is inclined to introversion.
Predicting treatment outcome
Results for our preliminary analysis (comparing empirically identified personality subgroups versus continuous factor scores as predictors in hierarchical multiple regressions) can be found in eTable 3. Across both sets of models, stage 1 (pre-treatment and treatment condition as predictors) indicated significant F change and stage 2 (personality subgroups or continuous factor scores as predictors) did not. For two outcome measures, PARS and CAIS School, the subgroup-by-treatment condition interaction terms added significant explained variance to the model (R-square change of .088 and .111, respectively, ps≤.01). In contrast, continuous factor scores and their interaction with treatment condition did not significantly add explained variance to the model for any outcome measure.
ANCOVA and logistic regression models
Of the 202 participants who were categorized into a personality subgroup above, children who were not randomized to an intervention (e.g., did not meet inclusion criteria; n=41) or who were assigned to a “treatment-as-usual” condition (n=17) were excluded from these models. In addition, participants missing pre- or post-treatment outcome measure data were excluded from analyses using pairwise deletion (Ns range: 111–121).
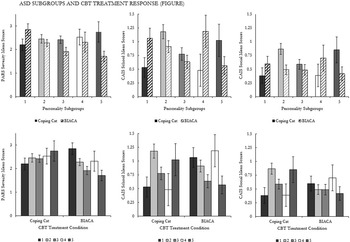
Pre- and post-treatment means and standard deviations for the five personality subgroups crossed with the two treatment conditions are presented in eTable 4. The interaction between personality subgroup and treatment condition was significant for PARS Severity, F(4, 110)=2.635, p=.038, the CAIS School subscale, F(4, 102)=3.077, p=.019, and the CAIS Social subscale, F(4, 105)=2.471, p=.049 (see Table 5). No significant effects were found the CAIS Family subscale, the CBCL subscales, and the SRS-2 subscales (see Table 5). The binary logistic regression model for the CGI-I was nonsignificant (omnibus test p=.124); it should be noted that the number of non-responders for both CBT conditions was minimal (see Wood et al., Reference Wood, Kendall, Wood, Kerns, Seltzer, Small, Lewin and Storch2020).
Table 5. ANCOVA Results for Response to Treatment by Personality Subgroups and Treatment Condition, Controlling for Pre-treatment Scores
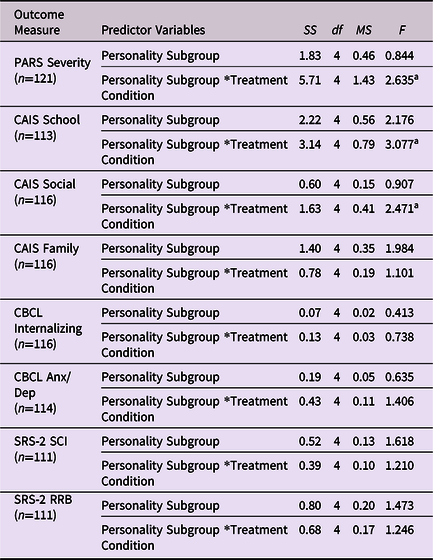
Note. Response to treatment is assessed through one primary outcome measure (PARS) and three secondary outcome measures (CAIS, CBCL, SRS-2). Cases from the TAU condition and cases missing pre- or post-treatment outcome measures data were excluded from analyses. “Personality Subgroup*Treatment Condition” serves as the interaction term used in the ANCOVA models. PARS = Pediatric Anxiety Rating Scale, CAIS = Child Anxiety Impact Scale, CBCL = Child Behavior Checklist, Anx/Dep = Anxiety/Depression, SRS-2 = Social Responsiveness Scale-2, SCI = Social Communication and Interaction, RRB = Restricted Interests and Repetitive Behavior. SS = sum of squares, df = degrees of freedom, MS = mean square, F = F-ratio.
a p < .05
Simple contrasts
Guided by inspection of the EMMs, simple contrasts for the PARS revealed lower post-treatment anxiety severity in BIACA versus CC for Group 3 (p=.034, 95% CI [0.04, 0.97], d Cohen=.579) and Group 5 (p=.033, 95% CI [0.08, 1.99], d Cohen=1.040) subgroups (see Figure 1; EMMs are grouped by personality subgroups [top row] and by CBT treatment condition [bottom row] for ease of comparison). Similarly, for the CAIS Social subscale, Group 2 had lower post-treatment EMMs, indicating fewer social difficulties, in BIACA as compared to CC (p=.005, 95% CI [0.12, 0.64], d Cohen=.492). Conversely, for the CAIS School subscale, Group 1 had lower post-treatment EMMs, indicating less maladjustment in school, for CC as compared to BIACA (p=.037, 95% CI [0.03, 1.04], d Cohen=.716).

Figure 1. PARS (Pediatric Anxiety Rating Scale) Severity, CAIS (Child Anxiety Impact Scale) School, and CAIS Social estimated marginal mean scores of personality subgroups in Coping Cat (standard-of-practice CBT) and BIACA (adapted CBT) treatment conditions (top: grouped by personality subgroup; bottom: grouped by CBT treatment condition). Error bars presented are ±1 standard error.
Simple contrasts within treatment conditions yielded similar findings (see Figure 1). Within the BIACA condition, Group 1 had higher post-treatment PARS and CAIS School EMMs (indicating more difficulties) than Group 3 (PARS: p=.003, 95% CI [0.33, 1.52], d Cohen=1.362; CAIS School: p=.047, 95% CI [0.01, 0.86], d Cohen=.701) and Group 5 (PARS: p=.001, 95% CI [0.48, 1.79], d Cohen=.864; CAIS School: p=.043, 95% CI [0.02, 0.98], d Cohen=1.172). Within the CC condition, Group 2 had higher CAIS School and CAIS Social post-treatment EMMs (with higher scores indicating greater adaptive difficulties) than Group 1 (CAIS School: p=.004, 95% CI [0.21, 1.09], d Cohen=.969; CAIS Social: p=.006, 95% CI [0.14, 0.83], d Cohen=.740), Group 3 (CAIS School: p=.023, 95% CI [0.06, 0.75], d Cohen=.424; CAIS Social: p=.041, 95% CI [0.01, 0.55], d Cohen=.187), and Group 4 (CAIS School: p=.030, 95% CI [0.07, 1.33], d Cohen=1.361; CAIS Social: p=.040, 95% CI [0.02, 0.94], d Cohen=.299).
Discussion
The empirically identified subgroups of children with ASD in this sample resembled the subgroups identified in a cluster analytic study of adults with ASD (Schwartzman et al., Reference Schwartzman, Wood and Kapp2016) in numerous ways, particularly the nearly universal indicators of shyness and a lack of cheerfulness (indicators of low Extraversion) across subgroups, the inconsistent patterns of high Neuroticism scores in some but not all subgroups, and the presence of a large subgroup with a dysregulated and defiant FFM profile (i.e., Group 2) with indicators of low Agreeableness and low Extraversion in conjunction with low Conscientiousness. The similarity of the identified subgroups from these two distinct samples of individuals with ASD is notable as one featured adults recruited via the internet for a descriptive study, and the other featured children recruited for concurrent interfering anxiety in a clinical trial of CBT. Subgroup membership was linked with differential CBT treatment response, in which Groups 3 and 5 responded better to BIACA on the primary outcome measure. Subgroup membership also impacted treatment outcome on a secondary outcome measure, with Group 2 responding better to BIACA and Group 1 responding better to CC. All told, these results offer initial evidence of the predictive validity of the subgroup typology and suggest that personalizing intervention components based on phenotypic profiles among children with ASD could be a promising approach to treatment allocation.
In the FFM literature, the Extraversion construct is best understood as a broad manifestation of reward sensitivity that simultaneously entails tendencies toward positive affectivity, pursuit of nonsocial rewarding goals and activities, as well as sociability/social reward seeking (DeYoung, Reference DeYoung2015). In the present study, the identified subgroups shared the commonality of low Extraversion across multiple facets, particularly Shyness and (low) Optimism, the former of which includes components of social reticence (e.g., difficulty getting used to new people) and social withdrawal (e.g., remaining quiet in social situations) and the latter of which is largely a measure of cheerfulness (e.g., making others laugh; feeling content, laughing off problems). A similar pattern was also seen in the empirically identified subgroups of adults with ASD reported in the study by Schwartzman and colleagues (Reference Schwartzman, Wood and Kapp2016), in which no subgroups were above average in Extraversion, and three of four subgroups were low in this trait. Low Extraversion has been the strongest of the FFM correlates of ASD symptomatology across studies (Lodi-Smith et al., Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019). Even when using subgrouping methodology as employed in the present study, shyness and a lack of cheerfulness were nearly ubiquitous features of each identified subgroup. Two of the three largest subgroups in this sample also showed trends of low verbal expressiveness and low energy, the other two facets of Extraversion assessed with the FFM measure employed herein. If manifestations of certain indicators of low Extraversion, particularly shyness and a lack of cheerfulness, were nearly universal traits in children with ASD with similar developmental and clinical characteristics to those in this study, even across subgroups, the meaning of this central/core feature might reasonably be queried. The simplest explanation for this is that low Extraversion is a common trait pattern amongst youth with ASD and comorbid anxiety, and this characteristic may be linked to the manifestation of certain core and associated phenotypic features of ASD (e.g., difficulties in social and communication interaction, internalizing symptoms).
However, while social communication challenges are defined as central to the ASD diagnostic taxon (APA, 2013), the affective elements that comprise shyness (e.g., anxiety/behavioral inhibition in less predictable social situations) and a lack of cheerfulness (low positive affectivity) are not diagnostic features of ASD as currently defined. The social motivation model of ASD emphasizes circumscribed social reward seeking as a fundamental determinant of ASD (Chevallier et al., Reference Chevallier, Kohls, Troiani, Brodkin and Schultz2012; Clements et al., Reference Clements, Zoltowski, Yankowitz, Yerys, Schultz and Herrington2018). The pattern of results here suggests that low trait reward sensitivity may not be limited to the social domain for children with ASD and similar clinical profiles to those in this sample. It may extend to broader aspects of emotion processing, including the temperamental antecedent and animating feature of Extraversion – positive affectivity (DeYoung, Reference DeYoung2015). It is well known in personality psychology that traits themselves are just emotional and behavioral tendencies, hardly precluding, for example, positive affect from manifesting strongly in certain situations even when being minimal in others (Mischel et al., Reference Mischel, Shoda and Mendoza-Denton2002). Appetitive emotions likely underlie talents and strengths (DeYoung, Reference DeYoung2015) as well as circumscribed interests and related behaviors among individuals with ASD (Bottini, Reference Bottini2018); the present findings would suggest that, complementary to those important aspects of goal-directed affect and behavior in children with ASD, positive affect and social confidence may also be less characteristic for many similar children with ASD in numerous other daily life contexts (e.g., aspects of school and family life) than for children not affected by ASD. Reward sensitivity has been an emphasis in recent neuroimaging research in ASD (Clements et al., Reference Clements, Zoltowski, Yankowitz, Yerys, Schultz and Herrington2018) and the present findings underscore the potential relevance of that aspect of emotion processing to a broader understanding of the neurobiological underpinnings of ASD.
Despite entailing a sample of children with both ASD and impairing anxiety, not every identified subgroup exhibited particularly high mean indices of Neuroticism, which is the FFM locus of broad trait negative affectivity. There are at least two likely explanations of this otherwise incongruous finding. First, a fraction of the children likely experienced more specific social anxiety than general or multifaceted anxiety as measured in the indicators of Neuroticism in the FFM measure that we employed (the HiPIC). This social anxiety may have been captured by the Shyness facet (embedded in the Extraversion factor of the HiPIC), which, as discussed above, was characteristically high for all of the identified subgroups in this sample. It should be noted that in some models of anxiety and autism, the greater difficulties encountered in many social settings for children with ASD are due to the features of autism (e.g., perspective taking difficulties impair judgment regarding expected social behaviors, leading to more social reprisals and rejections; Wood & Gadow, Reference Wood and Gadow2010), leading to a predictable basis for rational social anxiety – a higher risk or threat of unwanted outcomes in some social settings. Second, and not exclusive of the first explanation, it may have been that some of the children in the sample had developed focal anxious reactions to a stressful setting or settings in spite of not having the prototypical temperamental “diathesis” (i.e., high Neuroticism) preceding the onset of acute anxiety. In diathesis-stress models of anxiety disorders, a high degree of stress is sometimes sufficient to trigger an anxiety disorder despite a fairly modest diathesis (e.g., moderate or average trait anxiety; Mineka et al., Reference Mineka, Williams, Wolitzky-Taylor, Vrshek-Schallhorn, Craske, Hammen and Zinbarg2020). Socially fraught settings might produce this level of stress for some children with ASD, and other chronic demands that exceed coping resources could as well (e.g., organizational or stimulation-tolerance demands in the school setting; Wood & Gadow, Reference Wood and Gadow2010). The cluster analytic study of FFM profiles in adults with ASD by Schwartzman and colleagues (Reference Schwartzman, Wood and Kapp2016) found that only two of the four identified subgroups had high Neuroticism scores, despite the high mean Neuroticism score for the sample as a whole, again illustrating how treating individuals with ASD as a homogeneous group may obscure potentially important phenotypic differences.
Three subgroups in this sample – accounting for over half the children – exhibited high Egocentrism facet scores, likely reflecting less developed awareness or simulation of others’ perspectives and feelings, corresponding with the well-documented mentalizing difficulties for many people with ASD (e.g., Kana et al., Reference Kana, Maximo, Williams, Keller, Schipul, Cherkassky and Just2015). Yet, facets of agreeableness (of which Egocentrism is one) as a whole were highly variable within and across subgroups. Three of the subgroups were characterized by low or very low Dominance (i.e., scores that reflect high agreeableness including both social passivity and the tendency to “go with the flow”), and in one case (Group 3), this was the case even in the context of very high Egocentrism and very low Altruism (in both cases reflecting low agreeableness). This complex but informative pattern of findings underscores the value in examining the facets or aspects underlying the five personality factors in this type of research in ASD. As exemplified in the Results section, the broader FFM literature is helpful in illuminating some of the patterns seen in specific subgroups. Whereas Group 1 exhibited an overall tendency towards low plasticity, as represented by concurrent low Extraversion and low Openness to Experience (e.g., DeYoung, Reference DeYoung2015), Group 4 exhibited the opposite pattern. To the extent that plasticity facilitates flexibility with or orientation towards novelty, it is possible that these subgroups might differ substantially with regard to Restricted Interests and Repetitive Behaviors (RRBs) and composure in changing circumstances, potentially offering one psychological mechanism accounting for some of the notable variability in RRB severity among children with ASD (Leekam et al., Reference Leekam, Prior and Uljarevic2011).
In the present study, Group 5’s FFM profile resembled the Schwartzman and colleagues (Reference Schwartzman, Wood and Kapp2016) study’s “normative” subgroup, which had FFM facet scores that were comparable to the normative sample’s mean scores. However, differences in statistical approach and sample characteristics make a direct comparison of the two studies’ subgroups difficult. Even so, the two studies together provide evidence for a subgroup of individuals with ASD who do not exhibit a particularly distinctive profile of personality traits for their respective age groups (other than moderate introversion in the case of the present sample).
Certain subgroups responded better to one type of CBT treatment versus the other. This was most evident in Groups 3 and 5, in which those in the BIACA condition derived more benefit on the primary outcome measure than those in CC. BIACA also appeared to benefit those in Group 2 relatively more in terms of social impairment outcomes. While the present study does not offer a direct explanation of the mechanisms in which subgroups had differential treatment response to the two CBT conditions, insight can be garnered from the personality profiles. Possibly, an advantage of BIACA lies in its greater emphasis on addressing concurrent regulatory challenges (e.g., noncompliance, aggression) and development of theory-of-mind skills in the service of improving social adaptation in the contexts in which social anxiety is experienced. Key features demonstrated in Group 2 (high externalizing, as demonstrated by high Neuroticism, low Agreeableness, low Conscientiousness), Group 3 (limited perspective-taking [very high Egocentrism and low Conscientiousness]), and Group 5 (mild introversion) should be considered when treating anxiety symptoms in the ASD youth population within a CBT treatment structure.
In contrast, those in Group 1 responded better to CC on a measure of school-based impairment. A possible explanation of the latter finding may be that CC can be particularly effective when used with children with ASD who are relatively compliant. These traits minimize distractions and maximize learning opportunities within the structured nature of this condition, while the interactive approach of BIACA as well as its parent-training components may be compensating features for individuals without these traits.
These findings build upon the successful applications of the individual differences framework within clinical research (Lengel et al., Reference Lengel, Helle, DeShong, Meyer and Mullins-Sweatt2016). Personality traits map onto clinical characteristics beyond personality disorders (Krueger et al., Reference Krueger, Watson and Widiger2020; Lodi-Smith et al., Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019) and have implications for clinical outcomes (Bagby et al., Reference Bagby, Quilty, Segal, McBride, Kennedy and Costa2008; Gorwood et al., Reference Gorwood, Rouillon, Even, Falissard, Corruble and Moran2010; Joyce et al., Reference Joyce, McKenzie, Carter, Rae, Luty, Frampton and Mulder2007). A recent meta-analysis highlights this association, finding that all five domains in the FFM were associated with treatment outcomes (Bucher et al., Reference Bucher, Suzuki and Samuel2019). In line with this emerging subfield of clinical research, the present study serves as initial evidence of the utility of the FFM in psychotherapy treatment design and selection for youth with ASD.
Limitations
Although the present study was successful in identifying subgroups and related differential treatment response in a sample of children with ASD, several methodological limitations must be acknowledged. For one, the subgroups’ reliability across multiple samples remains to be seen; subgroups are not always replicated (Lanza & Rhoades, Reference Lanza and Rhoades2013). This concern is amplified by the present sample size. Although 202 participants served as a sufficient number for the LPA, it is likely that some treatment outcome moderator analyses lacked the statistical power to identify significant interaction effects, which is why these analyses should be viewed as exploratory and hypothesis-generating in nature. In addition, the study only included verbal children with intelligence quotients above 70 and impairing anxiety, and the sample was less diverse in terms of race, ethnicity, and socioeconomic status than the general population of children with ASD.
An additional limitation is that personality data were only collected via parent-report. While Schriber and colleagues (Reference Schriber, Robins and Solomon2014) demonstrated that individuals with and without ASD had comparable self-parent agreement on a FFM personality measure, given the potential discrepancies in parent versus child reports (Funder, Reference Funder1995; Karver, Reference Karver2006), it should be noted that the collected personality data may not fully capture a comprehensive picture of the participants’ personality profiles, especially in context of internal thoughts and feelings (Vazire, Reference Vazire2010). Thus, both self- and parent-report personality data may be informative in understanding subgroups in ASD in future research.
Conclusion
No definitive claims can be made about whether these FFM profiles reflect meaningful and replicable subtypes of ASD or predictors of treatment response. However, the present findings can be seen as seeds of future inquiry on both fronts. These findings suggest LPA may be useful in identifying relatively homogeneous subgroups in the ASD population. Additionally, the present study suggests that optimal treatment interventions might be elucidated based on individual difference profiles. The well-differentiated subgroups based on the FFM that were identified in this sample illustrate how many, and perhaps most, children within the population of those with ASD may deviate substantially from the average composite FFM profile of high Neuroticism and low Agreeableness, Extraversion, and Conscientiousness, and Openness to Experience reported in the literature (e.g., Lodi-Smith et al., Reference Lodi-Smith, Rodgers, Cunningham, Lopata and Thomeer2019). Substantially different FFM profiles among subgroups of those with ASD may have been largely invisible due to the common practice of focusing on the group means of individuals diagnosed with ASD compared with the group means of individuals without this diagnosis.
Ongoing research at the intersection of personality and ASD may help elucidate whether similar FFM-based subgroups continue to be replicated in other samples; eventually, the distinctions between these subgroups should be tested with other levels of evidence, such as through genetic and neuroscience methods. Additionally, recent research has demonstrated that personality traits can change as a result of clinical interventions (Roberts et al., Reference Roberts, Luo, Briley, Chow, Su and Hill2017). Future studies should examine whether individuals may change group membership in the context of empirically identified personality subgroups as a result of CBT, and whether some children demonstrate meaningful and distinct personality change over the course of intervention. Future research could also test if differences in treatment response related to FFM-based subgroups translate to other treatments for autism (e.g., applied behavioral analysis) and anxiety (e.g., mindfulness-based intervention; antidepressants). The ascertainment of phenotypically unique subgroups could potentially shed light on some of the varying manifestations of ASD, consistent with models of multiple autisms, and offer clues about their respective etiologies, as well as facilitate new research on the psychopathology and life trajectories of individuals with these varying phenotypic patterns.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S0954579421001115
Acknowledgments
We thank Dr. Connie Kasari (University of California, Los Angeles) and Dr. Matthew J. Madison (University of Georgia) for their expertise and feedback on this study.
Author contributions
Drs. Cho and Wood designed and carried out the study. Dr. Ferrer verified the analytic methods. All authors except Dr. Ferrer were involved in the collection of data. All authors were involved in the preparation and revision of the manuscript.
Funding statement
The present study utilized secondary data from a project supported by the National Institute of Child Health and Human Development (grant number: R01-HD090098).
Conflicts of interests
Dr. Kendall reports that he and his spouse receive royalties/income from the sales of materials about the treatment of anxiety in youth. All other authors report no conflict of interest.
Ethical standards
The present study utilized secondary data from a randomized, controlled trial (Wood et al., 2020), which was conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.