Since Kraepelin (Reference Kraepelin and Barkley1919) and Bleuler (Reference Bleuler and Zinkin1950), the qualitative and quantitative lifelong changes in cognitive performance and behaviour associated with schizophrenia have been widely debated. At the core are two questions examined in the present study : (a) the extent to which persons who will later develop schizophrenia are in fact different from their peers long before the onset of psychosis; and (b) the extent and rate at which cognitive performance and behaviour change after the manifestation of psychotic symptoms. There is evidence that, before falling ill, persons with schizophrenia show a lower IQ, withdrawn social behaviour, abnormalities of conduct, and very mild neurological deficits when compared with controls (classmates, siblings or matched non-cases, or relative to population norms) (Reference David, Malmberg and BrandtDavid et al, 1997; Reference Russell, Munro and JonesRussell et al, 1997; Reference Davidson, Reichenberg and RabinowitzDavidson et al, 1999). Yet, because of methodological difficulties, researchers have been severely hampered in attempting to discover when premorbid differences begin and whether differences increase closer to, and after, the time of onset of psychosis.
METHOD
The two questions above were examined by merging data from the National Hospitalisation Psychiatric Case Register in Israel with cognitive and behavioural test scores from the Israel Draft Board Pre-Induction Register. Merging these two data sets provided complete population data for all Israeli males born during a 7-year period. Some of the cohort were hospitalised in the decade after they had received their cognitive and behavioural assessment, thus providing data on premorbid functioning. Others had already been discharged from the hospital at the time of assessment, so providing data on functioning after the onset of illness. Cases were compared with their school peers (non-cases) who had never been in hospital and were found fit for military service.
Case registry
Hospitalisation and diagnostic data were extracted from the National Psychiatric Hospitalisation Case Register of the State of Israel Ministry of Health. The register is a complete listing of all stays in psychiatric hospitals since 1950, regardless of the type and auspices (public or private) of the facility. A special department of the Ministry of Health verifies compliance of reporting, completion of forms, and consistency of information. The source of the data is the report of the board-certified psychiatrist treating the patient, who is required by law to complete a form which is entered into the case register for anyone admitted to, and discharged from, a psychiatric bed in Israel. The form includes the diagnosis according to ICD-9 (World Health Organization, 1977). Although, as previously found, diagnoses in the register are very consistence over time (Reference Rabinowitz, Slyuzberg and RitsnerRabinowitz et al, 1994), only the diagnosis given at the time of last discharge was analysed in this report. In the cohort that we examined for this report, the diagnoses on first admission and final discharge were unchanged in 73% of the cases. The local Institutional Review Board approved the study.
Draft Board behavioural and cognitive assessment
By law, Israeli males between the ages of 16 and 17 are summoned for evaluation by the Draft Board for pre-induction screening. This includes assessing individuals who would be ineligible for service based on medical, psychiatric or other grounds. It therefore provides data on the entire unselected population of Israeli males.
The assessment consists of a physical examination and review of systems, and a psychiatric history conducted by a physician. Each subject also undergoes a battery of paper-and-pencil multiple-choice tests measuring cognitive ability, which is administered to recruits in a group, and a structured individual behavioural assessment interview conducted by a trained psychometrician.
The cognitive assessment consists of four tests (Table 1) : (a) the Otis-R, a modified, Otis-type verbal intelligence test adapted from the US Army Alpha Instructions Test, which is a measure of the ability to understand and carry out verbal instructions; (b) Similarities-R, a revised version of the ‘similarities’ sub-test of the Wechsler Adult Intelligence Scale (WAIS), which assesses verbal abstraction and categorisation (i.e. the ability to understand the relationship between words, and the use of this relationship in several contexts); (c) Arithmetic-R, which assesses mathematical reasoning, concentration, and concept manipulation; this is similar to the Arithmetic sub-test in the WAIS scale, but the problems are more difficult; and (d) Raven's Progressive Matrices-R (RPM-R), a modified version of Raven's Progressive Matrices, which measures non-verbal abstract reasoning and visual-spatial problem-solving abilities (Reference LezakLezak, 1995). The four cognitive scores added together form a highly valid measure of general intelligence. In the many validation studies conducted by the Draft Board, the 95th percentile of the sum of the cognitive scores was equivalent to an IQ above 135, and the correlation of summary score and the WAIS total IQ was above 0.90 (Reference GalGal, 1986).
Table 1 Description of cognitive tests included from military screening
| Description of test | Description of items (Reference KidumKidum, 1991) |
|---|---|
| Verbal intelligence | |
| (I) Otis-R, a modified Otis-type verbal intelligence test adapted from the US Army Alpha Instructions Test. It measures the ability to understand and carry out verbal instructions. | Word problems requiring strict adherence to detailed instructions. Sample items : 1. Connect the first letter of each third word in this sentence, if the word has a meaning, write it down, otherwise write the word nonsense…. 2. Connect the first letter of the first word in the list in front of you with the second letter of the third word with the third letter of the fourth word and the fourth letter of the second word and write down the word formed. |
| (2) Similarities-R, a revised version of the WAIS (Wechsler Adult Intelligence Scale) ‘similarities’ sub-test, which assesses verbal abstraction and categorisation (i.e. the ability to understand the relationship between words, and the use of this relationship in several contexts). Unlike the Wechsler test, subjects are requested not only to identify the semantic or causal relationships between the test items but also to apply them to target items. | Analogies and other word problems. Sample items : Skinny relates to thin, as short relates to— Money is to wallet as picture is to— Frying pan is to frying as cookie sheet is to— |
| Non-verbal intelligence | |
| (1) Raven's Progressive Matrices-R (RPM-R), a modified version of Raven's Progressive Matrices, which measures non-verbal abstract reasoning and visual-spatial problem-solving abilities (Reference LezakLezak, 1995). | A series of visual pattern-matching and analogy problems. The test requires conceptualisation of spatial, design and numerical relationships. |
| (2) Arithmetic-R, similar to the ‘arithmetic’ sub-test of the WAIS. | General arithmetical reasoning skills, concentration and concept manipulation. Has more items than the WAIS ‘arithmetic’ scale and is more difficult. |
The behavioural assessment, carried out by a trained psychometrician in the form of a structured interview, includes four sub-scales (Table 2) : (a) social functioning, which assesses social potency and social closeness; (b) individual autonomy, which assesses personal autonomy, maturity and self-directed behaviour; (c) organisational ability, which assesses compliance with timetables, self-mastery and self-care; and (d) physical activity, which assesses involvement in extra-curricular physical activities. The reliability and validity of these measures have been extensively tested by the Draft Board, and population-based norms are available for each of the tests (Reference Tubiana and Ben-ShakharTubiana & Ben-Shakhar, 1982; Reference GalGal, 1986).
Table 2 Description of behavioural assessments

| Behavioural | Description of test (Reference ReebReeb, 1968; Reference Tubiana and Ben-ShakharTubiana & Ben-Shakhar, 1982) | Description of items (Reference KidumKidum, 1991) |
|---|---|---|
| Social functioning | Ability to make and keep friends. Scale points are : (1) very poor=complete withdrawal; (2) poor=weak interpersonal contacts; (3) adequate=can form relationship with individuals and in a group; (4) good=good interpersonal relationships; (5) exceptional=superior interpersonal relatedness. | Sample items : How many good friends do you have ? Do you have a girlfriend ? Do you generally prefer to be with or without a group of companions ? How often do you go out on Friday evenings ? Do you tend to be the centre of the party ? |
| Individual autonomy | Autonomy in taking action and making decisions. Scale points are : (1) being totally dependent on others; (2) mostly dependent on others; (3) does not act alone; (4) generally able to act alone; and (5) works by themselves in most areas and autonomous in all areas. | A series of situations requiring action is presented and the respondent is asked how they would deal with the situation. Some of the situations relate to group pressure and interaction with groups. |
| Physical activity | Extent of involvement in physical activity. Scale points are : (1) no energy for physical activity; (2) lacks push for physical activity; (3) attributes no importance to physical activity; (4) if needed, will exert self; and (5) very physically active. | Respondents are asked about an inventory of physical activities ranging from age-typical to more strenuous activities. |
| Organisational ability | Adherence to a schedule and keeping order. Scale points are : (1) disorganised; (2) usually disorganised; (3) usually not, but can be, organised; (4) usually organised; and (5) always organised. | Sample questions : How often are you late for school ? How often are you late when you meet friends ? Do you consider yourself organised ? Who tidies up your room ? How disorganised is your room ? |
Case register merging
Using the Israeli equivalent of social security numbers, data from the psychiatric case register were merged with data from the army Draft Board register, using a special algorithm developed to protect the confidentiality of subjects (Reference RabinowitzRabinowitz, 1998). The merger covered all males who had first been admitted to a psychiatric hospital for a psychotic illness between 1985 and 1991 and whose diagnosis on their last discharge was schizophrenia, during the period ending 1 January 1996.
The score of each case was compared with the mean score of matched non-cases. Matched non-cases were the school classmates of cases who had the same army testing month, were found eligible for military service and who did not appear in the National Psychiatric Hospitalization Register. Matching cases to non-cases by high school attended at the time of testing, was an attempt to control for educational and social opportunities : additional details on matching of cases and non-cases are presented in Davidson et al (Reference Davidson, Reichenberg and Rabinowitz1999).
Study population
The merger identified 994 males who had been in hospital with a diagnosis of schizophrenia by the age of 26. The calculated risk for schizophrenia in the entire male population by this age was 0.52%. This is close to the predicted risk of 0.61% by age 40 (Reference Jones, Rodgers and MurrayJones et al, 1994) and compatible with the incidence of schizophrenia found in other studies (Reference Bromet, Dew, Eaton, Tsuang, Tohen and ZahnerBromet et al, 1995). The 994 cases had 12 076 classmates with the same army testing month who were noncases; thus, for every case there was an average of 12.1 matched non-cases.
From the 994 cases, 201 were excluded because they were older than the mandated testing age at the time of testing. Many of the excluded subjects were new immigrants who were not in the country at age of mandatory testing. In addition to contaminating the homogeneous age at testing, it would have been imposible to know whether the first admission in the psychiatric registry was in fact their first psychiatric admission. An additional 54 subjects who had been admitted to hospital more than 1 year prior to army testing were also excluded, as : (a) it was difficult to find suitable matched non-cases for them, as many of them did not attend regular schools; (b) there was considerable variation in time since hospitalisation (mean 1302 days (s.d.=1067), median 931); and (c) there was a disproportionate amount of missing data on most measures. Fifty-seven additional cases were excluded from the analysis because of missing data on every measure. In 104 of the cases included, data were missing on at least one measure. The present analysis thus focused on 692 males with a register diagnosis of schizophrenia, who were tested at ages 16 and 17 as mandated and who had been admitted to the hospital not more than 1 year prior to testing.
Statistical analysis
To explore the differences between the cases and matched non-cases, a difference score was calculated by subtracting the score of matched non-cases from that of the corresponding case for each measure. A positive value was obtained when the case scored higher than the matched non-cases. A negative value was obtained when the case scored lower than the non-cases.
To explore the relationship between the time of testing and time of first admission, a ‘time from testing until first admission’ variable was created by subtracting the year of first admission from the year of testing. A value of zero means that the first admission to psychiatric hospital was 1-365 days prior to testing. A value of 1 indicates that admission was within the first year (1-365 days) after testing, a value of 2 indicates that admission was within the second year, and the other positive values were similarly derived.
To examine our first research question, regarding differences in cognitive and behavioural assessments between persons who will later manifest schizophrenia and normal non-cases, paired-samples t-tests were performed by comparing the matched non-cases, after removing those 30 cases who had been tested after first admission and who had thus already been diagnosed as having schizophrenia. Bonferroni correction was used to control for multiple comparisons (0.05/8, P<0.006). These differences were then converted to effect size scores for easy comparison. This was done using the formula for differences between paired observations, in which the difference between means is divided by the within-population standard deviation and then divided by the square root of one minus the paired correlation of cases and non-cases (Reference CohenCohen, 1976).
The second set of analyses examined the main research question regarding the size of the difference scores, reflecting the extent to which cases differed from non-cases, and whether these would be inversely related to the time interval between testing and admission to hospital. Differences between all cases (those assessed both prior to, and after, first admission) and matched non-cases were compared by aggregating them on time from testing to admission. This was done by using the nine time intervals previously described (range 0-1 years prior to admission, to 8 years after). One-way analysis of variance was used to test for significance in mean differences as a function of time until admission, and a trend analysis was used to test for linearity of differences as a function of time. In an attempt to rule out the possibility that differences found relating to time before admission actually reflected differences in the age of first admission to hospital, the same one-way analysis of variance was done, using age of first admission as a dependent variable.
RESULTS
Cases v. non-cases
Table 3 presents the mean scores for the entire population and those obtained by the cases and their matched non-cases. Cases scored significantly worse on all measures than did their matched non-cases, and the latter scored lower than the population norms. The case/non-case differences remained significant even after the Bonferroni correction (P<0.006). The last column of the table presents effect size scores, to enable the magnitude of these differences to be compared. As seen, on the cognitive measures, the differences in effect size between cases and non-cases ranged from 0.58 to 0.40. The range for behavioural measures was wider, from an effect size difference of 1.25 on social functioning to 0.23 on organisational ability.
Table 3 Population norms (s.d.) for tests and comparison of means (s.d.) between cases (i.e. persons who have been hospitalised for schizophrenia) assessed prior to first admission and their matched non-cases (i.e. persons with no psychiatric hospitalisation) (n=662)

| Population norms | Cases v. matched non-cases | |||
|---|---|---|---|---|
| Paired-samples | t-tests | Effect size | ||
| Cognitive | ||||
| Similarities-R | 19.8 (6.9) | 16.4 (7.9) | t=7.3 | 0.40 |
| 18.4 (5.6) | d.f.=591 | |||
| P<0.001 | ||||
| Raven's Progressive | 21.1 (6.0) | 15.9 (7.6) | t=10.7 | 0.58 |
| Matrices-R | 18.6 (5.3) | d.f.=661 | ||
| P<0.001 | ||||
| Otis-R | 14.2 (3.4) | 12.0 (4.1) | t=9.8 | 0.56 |
| 13.4 (2.7) | d.f.=591 | |||
| P<0.001 | ||||
| Arithmetic-R | 13.3 (5.2) | 10.9 (5.4) | t=7.7 | 0.46 |
| 12.4 (3.7) | d.f.=591 | |||
| P<0.001 | ||||
| Behavioural | ||||
| Social functioning | 3.0 (0.7) | 2.5 (0.84) | t=14.1 | 1.25 |
| 3.0 (0.40) | d.f.=586 | |||
| P<0.001 | ||||
| Individual autonomy | 3.1 (0.68) | 2.9 (0.79) | t=5.2 | 0.56 |
| 3.1 (0.36) | d.f.=586 | |||
| P<0.001 | ||||
| Physical activity | 3.0 (0.8) | 2.5 (0.95) | t=7.8 | 0.47 |
| 2.8 (0.64) | d.f.=586 | |||
| P<0.001 | ||||
| Organisational ability | 3.0 (0.8) | 2.8 (0.86) | t=3.7 | 0.23 |
| 2.9 (0.43) | d.f.=586 | |||
| P<0.001 | ||||
After establishing that there were large differences between cases and non-cases on cognitive and behavioural functioning, we returned to our main question : whether these differences are progressively larger in individuals tested closer to the time when they are first admitted to hospital and continue to increase after that.
Time-related differences in cognitive functioning
A significant linear time difference between the scores of cases and non-cases was found on the RPM-R, shown in Fig. 1. As can be seen, the difference between the scores of cases and non-cases on the RPM-R was greater, the shorter the time between testing and admission and continued to increase after first admission as shown by the increase from scale point 1 (i.e. admission 1-2 years after testing) to scale point 0 (i.e. admission prior to testing). The one-way analysis of variance revealed significant differences (combined F=2.31, d.f.=8.683, P=0.02) with a significant linear term (F=5.2, P=0.02) and quadratic term (F=5.0, P=0.02). Additional analysis found that the linear trend in Fig. 1 diminished when the data were analysed without year 0 (i.e. assessed during the year after first admission to a psychiatric hospital) (linear term F=2.3, P=0.13, quadratic term F=4.5, P=0.03, combined F=2.6, P=0.01). For the other three cognitive measures, the results did not support time-related differences (combined : Arithmetic-R, F=0.72, P=0.67, d.f.=8.608; Similarities—R, F=0.76, d.f.=8,608, P=0.64; Otis-R, F=0.59, P=0.79, d.f.=8,608).

Fig. 1 Difference in scores on Raven's Matrices of non-cases v. patients with schizophrenia (n=692).
Additional analyses tested the possibility that the differences found relating to time until admission actually reflect an effect of the age at first admission to hospital, that is, that admission earlier in life was associated with worse performance. For this purpose, one-way analyses of variance were performed using the age at first hospitalisation, instead of time until first admission, for stratification. These analyses found no significant differences on the cognitive measures associated with age at first admission to hospital, thus suggesting that observed differences could not be attributed to that age (combined : RPM-R, F=1.2, d.f.=10,681, P=0.27; Arithmetic-R, F=0.93, d.f.=10,606, P=0.51; Similarities-R, F=0.96, d.f.=10,606, P=0.48; Otis-R, F=1.17, d.f.=10,606, P=0.31).
Time-related differences in behaviour
Differences between cases and non-cases relative to time until admission were found in the Social Functioning sub-scale and are illustrated in Fig. 2. The one-way analysis of variance revealed a significant linear term (combined F=2.7, P=0.007, linear term F=10.9, P=0.001) and no significant deviations from linearity. To rule out the possibility that the trend in Fig. 2 is due to the large decline at year 0 (i.e. psychiatric admission during the 365 days prior to testing), an additional analysis was done without year 0. This analysis showed that the linear trend diminished only slightly when year 0 was removed (combined F=2.2, P=0.03, linear term F=6.9, P=0.009, no significant non-linear terms).
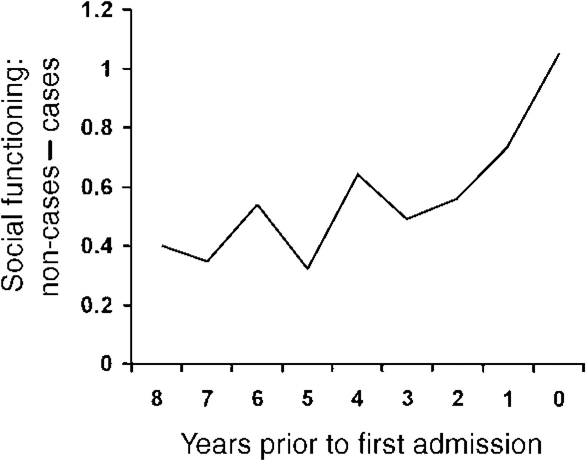
Fig. 2 Difference in social functioning between non-cases and patients with schizophrenia (n=606) (data missing in 86 cases).
The results did not, however, support time-related differences in individual autonomy (F=0.96, d.f.=8,597, P=0.47), physical activity (F=3.1, d.f.=8,597, P=0.002; linear F=0.52, P=0.47) and organisational ability (F=1.33, d.f.=8,597, P=0.22). Age at first admission was not significantly related to differences in behavioural measures (ANOVA : combined : social, F=1.00, d.f.=10,595, P=0.41; individual autonomy, F=0.74, d.f.=10,595, P=0.69; physical activity, F=1.7, d.f.=10,595, P=0.08; organisational ability, F=1.5, d.f.=10,595, P=0.13).
Additional analysis examined the relationship between time until admission and position on the 5-point social functioning scale (1=very poor (very withdrawn) to 5=exceptional (most socially adapted)). This revealed a consistent monotonic relationship. Cases who showed better social functioning were further away from admission than cases with poorer social functioning : specifically, the 80 cases who obtained a score of 1 (very poor) were on average 3.6 (s.d.=2.0) years from admission, those rated as having poor social functioning (n=218; score 2) were 3.7 (s.d.=2.1) years away; those with adequate social functioning (n=254; score 3) 4.2 (s.d.=2.2) years, and those who had good social functioning (n=52; score 4) were 4.4 (s.d.=2.2) years away (only two of the cases had a score of 5 (exceptional social functioning) and hence could not be analysed). This distribution showed a significant linear trend (combined F=3.9, P=0.009, linear term 10.2, P=0.001, no significant non-linear terms).
DISCUSSION
The results are consistent with previous work indicating that there are premorbid differences in cognitive and social functioning between persons who will develop schizophrenia and those who will not. The most pronounced difference we found was in social functioning. There was a clear linear relationship between impairment in social functioning and the time that elapsed until, and time after, first admission to hospital. This indicates that impending admission to hospital is associated with very poor social functioning, even if any overt symptoms which would lead to a diagnosis of schizophrenia are absent. A less pronounced linear relationship was found for the RPM-R, which is a highly valid measure of general intelligence. The study results also suggest that the differences found in time until admission were not related to differences in age at onset.
Comparison with previous studies
The differences we found between cases and non-cases on the cognitive measures of intelligence ranged in effect size scores from 0.40 to 0.58. Looking at previous studies in this area, we were able to calculate effect size scores comparing cases and non-cases for six (Reference Schwartzman and DouglasSchwartzman & Douglas, 1962; Reference Albee, Lane and ReuterAlbee et al, 1964; Reference OffordOfford, 1974; Reference Done, Crow and JohnstoneDone et al, 1994; Reference Jones, Rodgers and MurrayJones et al, 1994; Reference Russell, Munro and JonesRussell et al, 1997). These differences ranged from an effect size of 1 (one standard deviation) (Reference OffordOfford, 1974) to as low as 0.35 (Reference Schwartzman and DouglasSchwartzman & Douglas, 1962), with values in the other studies ranging from 0.52 (Reference Albee, Lane and ReuterAlbee et al, 1964; Reference Done, Crow and JohnstoneDone et al, 1994) to 0.82 (Reference Jones, Rodgers and MurrayJones et al, 1994). The results of the present study were in the middle range of these values; although it is possible that cognitive measures used in this study were not those most inclined to show decline, and that other measures would have shown more decline.
The evidence thus suggests that, despite inevitable differences in measures and ages of the study subjects, persons who later develop schizophrenia show scores on intelligence tests, premorbidly, from one-third to one standard deviation lower than those of non-cases.
There are several interpretations of the results reported here regarding the greater differences between cases and non-cases among cohorts closer to hospital admission. Consistent with the developmental hypothesis of schizophrenia, it could be postulated that late adolescence is associated with the manifestation of a pre-existing but dormant pathological process, which might have genetic, perinatal or environmental components. It could also be postulated that late adolescence puts increasingly more social and intellectual demands on an individual who already carries the vulnerability for psychosis. The progressive interaction between mounting demands and vulnerability leads predisposed individuals to cross a clinical threshold that divides those with abnormal but non-psychotic behaviour and those with psychosis (Reference Hollis, Taylor, Keshavan and MurrayHollis & Taylor, 1997).
The results appear to suggest that continuous decline in social functioning is prominent, and that there is also a decline in putative aspects of cognitive functioning. Because the data were cross-sectional, and not longitudinal, it is not possible to know whether the increase in the difference between cases and non-cases as the time to first psychotic hospital admission becomes shorter are due to a decline in functioning as individuals come closer to psychotic manifestation, or to a cohort effect. It would be almost impossible to collect longitudinal data on an entire unselected national population as is represented in this cross-sectional study.
Strengths and limitations
The major strength of this study was that it offered a unique opportunity, not afforded in previous studies, to examine differences between a population of cases and one of matched non-cases, using prospective data on both cognitive and behavioural measures. One major limitation is that the behavioural measures, although they have been validated in Israel in large cohorts, are not identical to the standardised measures commonly used. Also, the study only included males. Additionally, a small group of the non-cases may eventually become cases or be admitted to hospital for other psychiatric disorders. Given the low prevalence rate of schizophrenia and severe psychiatric disorders, it is unlikely that more than a handful of the 12 076 non-cases will eventually be admitted to hospital for a psychiatric disorder. Thus, the inclusion of non-cases who later in life become cases is not likely to have a significant impact on the results.
Another limitation is that we were not able to examine when premorbid differences begin to show, since our assessments were at age 16-17, whereas many previous studies have shown cognitive and social deficits well before that age. Also, given the delay of about 1 year from the time of onset of psychotic symptoms to admission to hospital (Reference Loebel, Lieberman and AlvirLoebel et al, 1992), it is possible that some of the persons whom we believed to be premorbid were actually already actively psychotic. Moreover, the diagnoses used are registry diagnoses, made by the treating psychiatrist based on signs, symptoms and history - not research diagnoses. Thus, concerns regarding the validity and reliability of the diagnoses are pertinent. Specifically, as has been suggested since the early 1980s, it is possible that some clinicians, particularly in long-term psychiatric hospitals, tend to assign a diagnosis of schizophrenia to patients for whom research diagnostic criteria based on a structured interview would have resulted in a diagnosis of bipolar affective disorder (Reference Lipton and SimonLipton & Simon, 1985) and this in spite of the wide acceptance of the DSM-III and DSM-IV and of the ICD-9 criteria. Furthermore, recent evidence has challenged the dichotomous Kraepelinian distinction between schizophrenia and affective disorders (Reference CrowCrow, 1998), and this challenge holds true in particular for chronically ill in-patients.
In conclusion, the results confirm previous studies that persons who later suffer from schizophrenia do have premorbid cognitive and behavioural deficits. The differences found in the time elapsing between testing and first admission to hospital indirectly support the belief that the decline in social functioning and cognition progresses as the symptoms of psychosis become manifest, and thereafter.
CLINICAL IMPLICATIONS AND LIMITATIONS
CLINICAL IMPLICATIONS
-
▪ There are premorbid behavioural and cognitive deficits associated with schizophrenia.
-
▪ The premorbid deficits become greater as the psychotic exacerbation is approached, and increase further during the early course of schizophrenia.
-
▪ The deterioration is manifest more clearly in social functioning than in intelligence.
LIMITATIONS
-
▪ Use of cross-sectional data.
-
▪ Use of non-standard behavioural measures.
-
▪ Use of registry diagnoses, not research diagnoses.
ACKNOWLEDGEMENT
J.R. was supported in part by a Young Investigator Award from US National Alliance for Research on Schizophrenia and Affective Disorders.








eLetters
No eLetters have been published for this article.