Progressive supranuclear palsy (PSP) is a movement disorder with a large-scale network disruption resulting in various signs and symptoms including cognition and gait impairment across its different variants. According to the clinical course and combination of symptoms and signs, PSP have been classified into different subtypes including PSP Richardson syndrome (PSP-RS) and PSP-Parkinsonism (PSP-P). PSP-RS is the most prevalent type followed by PSP-P. Among various clinical motor characteristics in PSP, applause sign (AS) is one of them. AS is elicited with three clap test and a positive sign is considered when a patient fails to stop after three claps as instructed Reference Dubois, Slachevsky, Pillon, Beato, Villalponda and Litvan1 (Supplementary Video 1). Although this motor perseverative behavior is reported in dementia and various Parkinsonian disorders, the frequency of this character has not been investigated in various PSP subtypes. Reference Luzzi, Fabi, Pesallaccia, Silvestrini and Provinciali2 Moreover, factors associated with this motor sign in PSP patients are yet to be fully elucidated. AS is observed in subjects with fronto-subcortical disconnections. This brain network is also responsible for gait and executive function in human. We hypothesize that PSP patients with positive AS are associated with more impaired gait and higher-order cognitive functions. Therefore, we compared the executive functions, motor signs, and gait in PSP patients with positive and negative AS.
The study was approved by the institutional ethics committee and written informed consent was obtained from all the study participants. All patients were diagnosed according to the Movement Disorder Society (MDS) criteria by a movement disorder neurologist. Reference Höglinger, Respondek and Stamelou3 Motor functions were measured using part III of the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS). Reference Goetz, Tilley and Shaftman4 Cognitive assessments were performed through Mini-Mental State Examination (MMSE). Reference Folstein, Folstein and McHugh5 Mattis Dementia Rating Scale-2 was used to examine global and higher level of cognitive function, that is, attention (ATT), initiation/perseveration (I/P), construction, conceptualization and memory (MEM). 6 Gait was also characterized using a 500 cm long electronic walkway (GAITRite®, CIR Systems Inc., Franklin , NJ, USA) which had pressure sensors embedded in it. Subjects who could walk 25 m without any aid were instructed to walk four times successively at a self-selected normal pace on GAITRite®. The first walk was meant to make the patient accustomed to the task and was excluded from further analysis. In order to interpret gait outcomes, a well-established gait model was used. Reference Lord, Galna, Verghese, Coleman, Burn and Rochester7 All the data were statistically analyzed using SPSS software package Version 20 (IBM). The normality of the data was examined using Shapiro−Wilk test. All the data were statistically analyzed using SPSS software package Version 20 (IBM). The normality of the data was examined using Shapiro−Wilk test. Accordingly, unpaired independent t-test and Mann−Whitney U test were performed for parametric and nonparametric data, respectively, to compare demographic, disease profile, and gait characteristics between PSP patients with and without AS. All data were reported as means and SD unless otherwise stated. p values of <0.05 were considered statistically significant for all the statistical tests.
Thirty-four (67% men) consecutive clinically diagnosed cases of PSP patients (mean age of 63 years; mean age of onset 61 years) were recruited from the movement disorder outpatient department of a neuroscience institute in India. As expected, the majority of them were from PSP-RS followed by PSP-P variants.
We found that 12 out of 34 PSP patients presented with positive AS. The disease duration (2.7 vs. 2.2 years, p = 0.394) was comparable between patients with positive and negative AS. Mean total score of MDS-UPDRS III was significantly higher in PSP with positive AS (Table 1). Total MMSE score were comparable between these groups, but the score of global cognitive function and higher-order cognitive functions, that is, ATT and MEM were significantly lower in positive AS cohort. Gait study revealed that step length variability was significantly greater in PSP patients with positive AS (4.02 ± 1.13 vs. 2.66 ± 1.27, p = 0.009). Besides, the difference in gait velocity in these two cohorts showed a trend of significance. PSP with positive AS walked with a slower velocity compared to negative AS group, although it did not reach a level of significance (53.76 ± 13.03 vs. 66.16 ± 16.87, p = 0.055; Table 2).
Table 1: Demographic and disease profile of patients with PSP
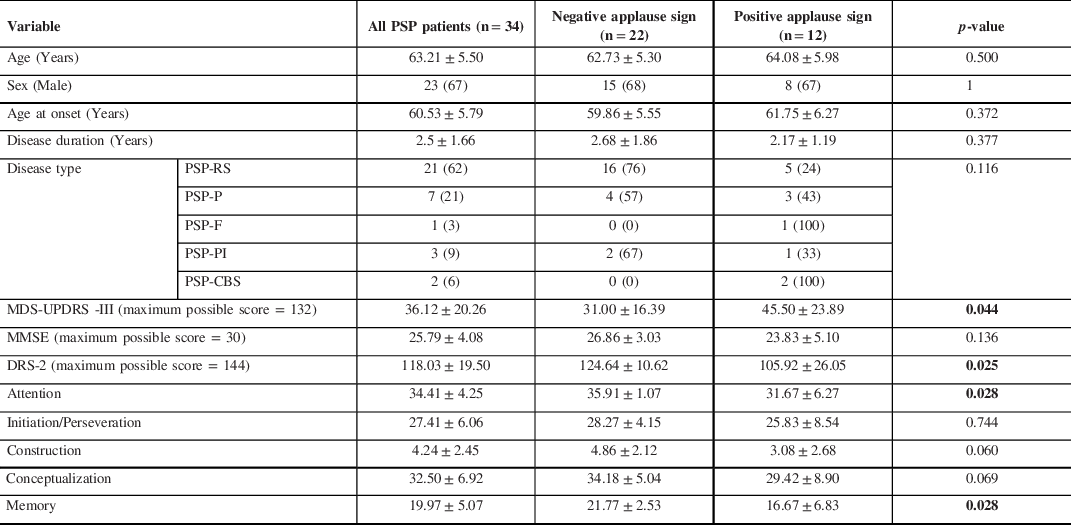
DRS-2 = Dementia Rating Scale version 2; MDS-UPDRS III = Movement Disorders Society Unified Parkinson’s Disease Rating Scale part III; n = sample size; PSP-CBS = progressive supranuclear palsy with predominant corticobasal syndrome; PSP-F = progressive supranuclear palsy with predominant frontal presentation; PSP-P = progressive supranuclear palsy with predominant Parkinsonism; PSP-PGF = progressive supranuclear palsy with progressive gait freezing; PSP-PI = PSP with predominant postural instability; PSP-RS = progressive supranuclear Palsy−Richardson syndrome.
Numerical variables are presented as mean ± standard deviation, and categorical variables as numbers with the corresponding percentage in parentheses. The p values were analyzed using two-tailed independent t-test in case of numerical variables and Fisher’s exact test in case of categorical variables. p < 0.01 considered significant (indicated in bold).
Table 2: Gait characteristics of PSP with and without applause sign

AS = applause sign; n = sample size; PSP = progressive supranuclear palsy; SD = standard deviation.
Data are presented as mean ± standard deviation. The p values were analyzed using two-tailed independent t-test. p < 0.01 considered significant (indicated in bold).
AS has been considered as a clinical sign of various disorders with fronto-subcortical disconnections including PSP. Similar to the previous report (40%), the overall frequency of AS was 35% in this study. Reference Schönecker, Hell and Bötzel8 As expected, PSP-RS was a common variant in our cohort. It is expected that PSP patients can have significantly impaired executive dysfunction due to the affected frontal brain structures. In this study, PSP patients with positive AS showed higher impairment of ATT and MEM functions compared to applause-negative group. In addition, global cognition was also poor in applause-positive PSP patients. This might suggest that higher-order cognitive functions (i.e., ATT and MEM) is essential for motor control in PSP and impairment of these cognitive domains might precipitate a motor preservative behavior like AS. We further expected a larger impairment in the I/P score in PSP patients with AS. Unlike previous report, we did not observe a significant difference in this domain between patients with and without AS.
Besides cognitive function, motor function was also found to be affected more in PSP patients with positive AS. The step length variability was more pronounced in them. Gait variability is a known measure of dynamic stability which is often impaired and found to be independently associated with impaired ATT in PSP patients. Reference Toebes, Hoozemans, Furrer, Dekker and van Dieën9,Reference Chatterjee, Choudhury and Siddique10
In our case, the unstable gait of applause-positive PSP patients could be either an independent predictor or a resultant of their impaired ATT. However, predictive analysis was not performed due to the small sample size. We also expected a significantly slower gait speed in patients with positive AS as, both ATT and MEM were associated with gait speed in this study. Possibly the study was underpowered to appreciate the mentioned difference.
PSP patients with AS presented with a more severe cognitive and motor impairment. ATT and MEM domains of cognition were most significantly affected in these patients. Gait variability was comparatively more compromised in patients with AS. Based on these findings, we propose PSP patients with positive AS need closer monitoring and therapy as compared to those without AS. The study stresses on the link between higher-order cognitive function and motor control in PSP patients.
Acknowledgements
We would like to thank all the participants who have kindly taken part in the study.
Authors’ Contributions:
Koustav Chatterjee (KC): Study concept and design, acquisition of data, analysis and interpretation, first draft of the manuscript, and critical revision of the manuscript for important intellectual content.
Supriyo Choudhury (SC): Study concept and design, data analysis and interpretation, and critical revision of the manuscript for important intellectual content.
Santosh Trivedi (ST): Acquisition of data and critical revision of the manuscript for important intellectual content.
Purba Basu (PB): Acquisition of data and critical revision of the manuscript for important intellectual content.
Hrishikesh Kumar (HK): Study concept and design, acquisition of data, analysis and interpretation, critical revision of the manuscript for important intellectual content, and study supervision.
Conflict of Interest
All the authors have nothing to declare.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/cjn.2021.216




