Introduction
Mental health problems make up a significant portion of the global burden of disease (Murray et al., Reference Murray, Vos, Lozano, Naghavi, Flaxman and Michaud2012) and the majority of those in need of services do not receive treatment (Bruckner et al., Reference Bruckner, Scheffler, Shen, Yoon, Chisholm and Morris2011; Kohn et al., Reference Kohn, Saxena, Levav and Saraceno2004; Wang et al., Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges and Bromet2007). The treatment gap is particularly pronounced in low- and middle-income countries (LMICs) due to challenges such as limited mental health systems, lack of professionals, shortage of financial resources and government commitment, and stigma associated with mental health disorders (Kakuma et al., Reference Kakuma, Minas, van Ginneken, Dal Poz, Desiraju and Morris2011; Saxena et al., Reference Saxena, Thornicroft, Knapp and Whiteford2007).
Although randomized controlled trials (RCTs) have demonstrated that evidence-based treatments (EBTs) for mental health problems delivered by lay providers can be effective in LMICs, scale-up and sustainability of such EBTs has been limited (van Ginneken et al., Reference van Ginneken, Tharyan, Lewin, Rao, Meera and Pian2013). One barrier to scale-up and sustainability is that despite sometimes impacting a wider range of outcomes (Craske et al., Reference Craske, Farchione, Allen, Barrios, Stoyanova and Rose2007; Dear et al., Reference Dear, Staples, Terides, Fogliati, Sheehan and Johnston2016; Titov et al., Reference Titov, Fogliati, Staples, Gandy, Johnston and Wootton2016), most EBTs were designed to predominantly focus on one primary presenting problem or diagnosis, with limited teaching on how to manage comorbidity (e.g. post-traumatic stress disorder) (Mansell et al., Reference Mansell, Harvey, Watkins and Shafran2008; McHugh et al., Reference McHugh, Murray and Barlow2009; Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary and Haydary2014a; Murray and Jordans, Reference Murray and Jordans2016; Ventevogel and Spiegel, Reference Ventevogel and Spiegel2015). However, comorbidity is common (Weisz et al., Reference Weisz, Krumholz, Santucci, Thomassin and Ng2015). This requires lay providers to be trained in and master multiple EBTs and/or create extensive referral networks to deal with the diversity of problems (Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary and Haydary2014a).
A possible solution is the use of transdiagnostic treatments, which can be used to treat a range of mental health disorders and/or problems and are designed to handle comorbidity (McHugh et al., Reference McHugh, Murray and Barlow2009). The effectiveness of transdiagnostic treatments has been studied in high-income countries (HICs) with promising results across age groups and disorders (e.g. Fairburn et al., Reference Fairburn, Cooper, Doll, O'Connor, Bohn and Hawker2009; Farchione et al., Reference Farchione, Fairholme, Ellard, Boisseau, Thompson-Hollands and Carl2012; Weisz et al., Reference Weisz, Chorpita, Palinkas, Schoenwald, Miranda and Bearman2012). Like single-disorder treatments, transdiagnostic approaches vary in their treatment design (Boustani et al., Reference Boustani, Gellatly, Westman and Chorpita BF2017). Some transdiagnostic treatments – like some single-disorder treatments – are modular, such that elements within a treatment can mostly be delivered independently of one another, with varying sequencing (Chorpita et al., Reference Chorpita, Daleiden and Weisz2005b) and include flexibility, defined as the ability to adapt and individualize during delivery (i.e. manuals do not dictate strict session-by-session content; number of sessions) (Boustani et al., Reference Boustani, Gellatly, Westman and Chorpita BF2017). Others are more linear, with a specific ordering of elements and a specified number of sessions (e.g. Problem Management Plus; Dawson et al., Reference Dawson, Bryant, Harper, Kuowei Tay, Rahman, Schafer and van Ommeren2015). While there are varying approaches conceptualizing transdiagnostic treatment (Boustani et al., Reference Boustani, Gellatly, Westman and Chorpita BF2017; Marchette and Weisz, Reference Marchette and Weisz2017; Sauer-Zavala et al., Reference Sauer-Zavala, Gutner, Farchione, Boettcher, Bullis and Barlow2017), one approach involves teaching providers a set of common practice elements from EBTs and decision rules that guide the selection, sequencing, and dosage of core and optional treatment elements based on client presentation (Chorpita and Daleiden, Reference Chorpita and Daleiden2009; Chorpita et al., Reference Chorpita, Daleiden and Weisz2005a).
Building on the work of other transdiagnostic treatment developers, including Barlow, Weisz and Chorpita, we developed a multi-problem transdiagnostic treatment that was modular and flexible specifically for lay providers in low resource settings, the Common Elements Treatment Approach (CETA; Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary and Haydary2014a).The goal was to simplify a model for lay providers by having few elements (compared with some other multi-problem, modular approaches; Weisz et al., Reference Weisz, Chorpita, Palinkas, Schoenwald, Miranda and Bearman2012) and simple language due to the need for delivery by lay counsellors. We also sought to develop a strategy where the decision making on element selection, sequence and dose could be in the hands of lay providers and their local supervisors (rather than professionals), given limited availability of mental health professionals in LMIC. Thus, CETA was developed with a small number of elements, decision rules that guide providers in decision making, and an approach to training, practice and supervision (i.e. the Apprenticeship Model) that builds supervisor and provider skills to make these decisions, with providers under supervision, and the supervisors receiving support from trainers [see Murray et al. (Reference Murray, Dorsey, Bolton, Jordans, Rahman, Bass and Verdeli2011) for more details]. Clinical decision making in CETA is based on a client's initial symptom presentation (e.g. primary presenting problem; comorbidity) and ongoing problems (symptom changes/treatment response over the course of treatment) [see Murray et al. (Reference Murray, Dorsey, Haroz, Lee, Alsiary and Haydary2014a) for more information]. In this way, CETA inherently allows for – and provides guidelines for – what Kendall and Beidas (Reference Kendall and Beidas2007) call ‘flexibility within fidelity’. Two RCTs of CETA have been completed in Iraq and Thailand using lay providers to treat torture- and trauma-affected populations (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014; Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015). In both trials, CETA was effective in reducing depression, anxiety and trauma-related symptoms compared with wait-control conditions. In Iraq (n = 149), treatment effect sizes (Cohen's d) were 2.38 for trauma symptoms, 1.56 for anxiety, and 1.78 for depression (Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015). On the Thailand–Myanmar border (n = 347), effect sizes were large for depression (d = 1.16) and trauma symptoms (d = 1.19) and moderate for anxiety symptoms (d = 0.79) and functioning (d = 0.63) (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014).
To help determine if a multi-problem and modular transdiagnostic approach would be a feasible solution in LMIC, an important question is whether lay providers are able to implement with both fidelity and flexibility. In CETA, fidelity would be operationalized as implementing and sequencing elements according to the decision rules. Flexibility is the ability of a provider – at times – to modify the selection, sequencing, and/or dose of elements based on the initial and ongoing presentation of the client. This flexibility is part of the design for modular approaches, yet whether or not providers make use of the flexibility is unclear, and was not part of the examination in either RCT.
The goal of this study was to explore the question of how a modular multi-problem transdiagnostic treatment was delivered by lay providers in the two recently completed RCTs of CETA in Iraq and Thailand, and if lay counsellors utilized the flexibility inherent in this modular type of transdiagnostic approach. We first describe days in treatment, number of sessions, and for the Thailand site, length of treatment sessions (i.e. minutes). We then examine elements delivered by providers to further understand fidelity (treatment elements indicated by presenting problem) and flexibility (dose of elements; occasional selection of optional elements). For fidelity in these studies, we would expect to see relatively similar element selection and sequencing in each site due to inclusion criteria. With a modular approach, we would expect some ‘flexibility’, or variation in use of optional elements or dosing (number of sessions for a given element) given the diverse contexts, and expected individual differences in presenting symptoms. In other words, fidelity would be demonstrated by overall similarity across providers and both sites, while flexibility would be demonstrated by some variation in elements accounting for individual client differences (e.g. needing more than one session to understand an element, more extensive trauma history). We also sought to examine if there were any differences across individual counsellors that may have contributed to the fidelity or flexibility outcomes (e.g. a lay counsellor who did not understand an element, or preferred to always use one particular element).
Methods
Background information
This study uses individual session-level data from two RCTs of CETA, one in Southern Iraq (Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015) and one on the Thailand–Myanmar border (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014). Participants in both RCTs had experienced torture or systematic violence and had elevated levels of depression and/or trauma symptoms, but there were also slight methodological differences in the two study designs. We therefore present methods for both studies separately below (where indicated) and present results for each individual study.
Iraq
The trial was conducted in three rural areas of Southern Iraq, near the cities of Hilla, Karbala and Najaf – all having experienced political violence with ongoing bombings and military presence throughout the study (for more details, see Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015). Clients were recruited by community mental health workers, and other organizations working with people affected by torture or trauma. Inclusion criteria consisted of having experienced systematic violence and scoring higher than a locally validated cut-off score on a measure of symptoms related to post-traumatic stress disorder (Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015). The treatment sessions were conducted within Ministry of Health primary health care centres, except when participants had difficulty travelling. In those instances, sessions were conducted in a convenient place for the participant (e.g. home).
Thailand
This trial was conducted in the town of Mae Sot in the northwest of Thailand along the border with Myanmar, an area with substantial refugees and migrants from Myanmar (for more details, see Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014). Many of the refugees and migrants residing in Mae Sot had experienced past trauma while fleeing Myanmar as well as ongoing daily stressors due to their illegal status in Thailand. Clients were recruited by counsellors and organizations that were working with the Burmese population in Mae Sot. To be included in the trial, participants had to have experienced at least one traumatic event and have moderate to severe depression or post-traumatic stress based on locally validated measures (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014). The intervention was delivered in homes, offices, teashops and/or other private spaces in the community that were convenient and safe (i.e. low risk of harassment by authorities) for the client.
Measures
Weekly treatment monitoring
For every participant who was randomized to the treatment condition (CETA) in the RCTs, counsellors completed a weekly Client Monitoring Form (CMF) for each session. The CMF included information on the session number, which element/s was delivered during the session, questions to assess current suicidal and/or homicidal risk, and a plan for the following session. Reporting of element delivery varied by site: in Iraq, only the primary element of focus for each session was recorded on the CMF; in Thailand, up to three elements could be recorded. The Thailand study followed the Iraq study, and therefore the study protocol was revised in this manner in order to capture more information about secondary elements reviewed or previewed, even if not the primary focus (similar to session structure of many CBT-based treatments). For example, a provider might review homework for the prior element and then move on to a new element. In Thailand the minutes of each session was recorded; this was not recorded in Iraq.
Weekly symptom monitoring
The CMF also included a 12-item symptom monitoring assessment, with items drawn from the site-specific RCT study measures (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014; Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015) that assessed symptoms of depression, anxiety and trauma via client self-report. The CMF included the same items in each setting with the exception of two additional alcohol use items that were asked only of participants in Thailand, but were not included in calculating mental health symptom summary scores. Response options for the mental health symptom items differed in the two sites (Iraq: 0 ‘never/no’ to 3 ‘very often (more than five times per week)’); Thailand: 0 ‘none of the time’ to 4 ‘almost all the time’). Client responses on the items were also used to guide element choice during treatment. For example, high scores for a particular item(s) might result in adding an element or providing another ‘dose’ of a current element. The RCT study measures were validated locally and consisted of the Hopkins Symptom Checklist 25 (HSCL-25; Hesbacher et al., Reference Hesbacher, Rickels, Morris, Newman and Rosenfeld1980; Winokur et al., Reference Winokur, Winokur, Rickels and Cox1984) and the Harvard Trauma Questionnaire (HTQ; Mollica et al., Reference Mollica, Caspi-Yavin, Bollini, Truong, Tor and Lavelle1992) for depression and post-traumatic stress symptoms, respectively (Mollica et al., Reference Mollica, McDonald, Massagli and Silove2005). Locally developed items were added as well, based on qualitative research to identify locally relevant signs and symptoms of depression and trauma also (Haroz et al., Reference Haroz, Bass, Lee, Murray, Robinson and Bolton2014; Weiss and Bolton, Reference Weiss and Bolton2010).
Lay counsellors
CETA was delivered by local Arabic-speaking or Burmese-speaking lay counsellors with no formal training in mental health. In Iraq, most of the 12 counsellors were community health workers who had training in physical health services equivalent to nurses. The average number of clients per counsellor was 7.67 (SD = 2.42; range 5–12). The two supervisors in Iraq were bilingual (Arabic and English) psychiatrists, trained through medical school but with little experience of talk therapies. In Thailand, all 19 counsellors were individuals who left Myanmar to live in Thailand; some were lay community workers, teachers or health workers. Each counsellor had an average of 8.6 clients over the course of the study (SD = 6.19; range 1–25). There were three supervisors in Thailand: a medical doctor with no previous counselling or mental health training, and two other individuals selected due to being bilingual (Burmese and English), in a leadership role in their organization, and who performed well in the initial CETA counsellor training. The non-medical supervisors did not have any formal mental health training and had never been counsellors before.
Intervention training and supervision
The Common Elements Treatment Approach (CETA) treats a range of common mental health problems, such as symptoms related to traumatic experiences, depression, anxiety and substance use, by using a combination of nine common therapeutic elements (Table 1) (Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary and Haydary2014a).
Table 1. CETA elements

1 Engagement and Psychoeducation were often delivered together in the first session.
2 When family needed to be engaged, Psychoeducation could involve two sessions. Otherwise, the recommendation was ½–1.
3 Only included in Thailand.
In both trials, providers were trained in CETA (L.K.M., S.D.) using the apprenticeship training model (Murray et al., Reference Murray, Dorsey, Bolton, Jordans, Rahman, Bass and Verdeli2011), which includes: (1) a 10-day in-person training with didactics, modelling and substantial time for role play/practice with trainer and peer feedback, (2) weekly intervention practice in small groups run by local supervisors (1–2 months), and finally (3) provision of CETA to 1–2 clients under close supervision (weekly with group supervision meetings for 2–4 months).
During the in-person training, counsellors and supervisors were trained in treatment elements, decision rules for selecting and combining elements, sequencing of elements, and how to determine the dose of each element based on clients’ presenting problem(s). Once counsellors learned the elements, they were taught the ‘core flow’ for trauma and that it followed the order of existing evidence-based treatments (see Fig. 1). For the two RCTs from which these data are drawn, the trauma and torture focus (and related inclusion criteria) was mandated based on funding and inclusion criteria. Optional elements included Relaxation, Behavioural Activation/Getting Active, In vivo Exposure, and in the Thailand RCT, Screening and Brief Intervention (SBI) for high alcohol use. As the live training progressed, we began teaching options for ‘dosing’ the elements within the core ‘trauma’ flow. Rules were explained that if the steps within an element were not finished, the counsellor would complete the remaining steps the following session; or if a client did not do the homework or did not understand the element, the element may need to be focused on for another session (also increasing dose). In addition, trainees were read client vignettes (e.g. ‘a client has another traumatic event in their life that is causing problems in their life’), with the goal being that trainees would think through treatment for this client, and determine that another session of exposure was needed (see Fig. 2, Vignette 1). In the live training, counsellors were then introduced to the idea of adding elements based on variability in presenting problems of clients. They were trained to use several criteria to make these decisions: (a) scores on the clinical assessment at intake, (b) what the client does and says in session (affect and behaviour), and (c) consultation with supervisor. The developers of CETA created an Element Decision Making Table (EDMT), which took the items on the client monitoring score and put them under primary problem areas (see example in Fig. 3). If a client indicated symptoms of depression related to not engaging in pleasurable activities, their score on the Getting Active scale might be 7/9, indicating that a counsellor may want to add Getting Active element (see Fig. 2, Vignette 2).
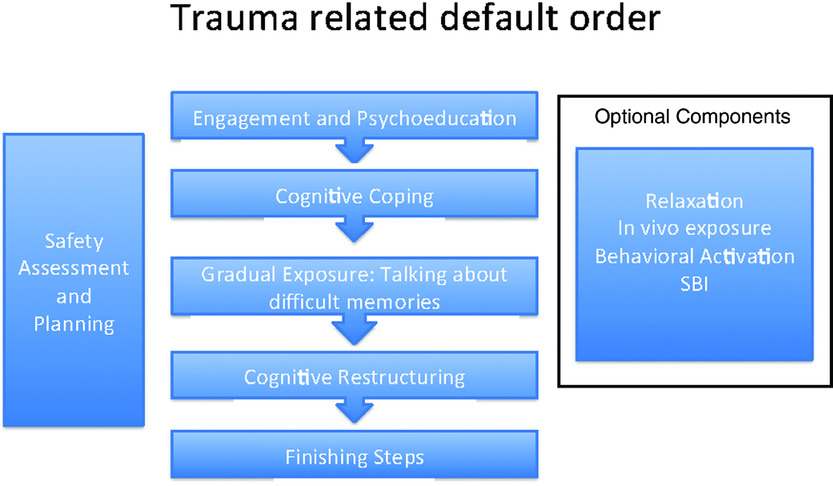
Figure 1. Element flow chart for clients who have experienced a traumatic event and have trauma-related symptoms. Counsellors can add in Relaxation, Behavioural Activation, and/or SBI (in Thailand), as needed. They also can choose the dose of each core element.
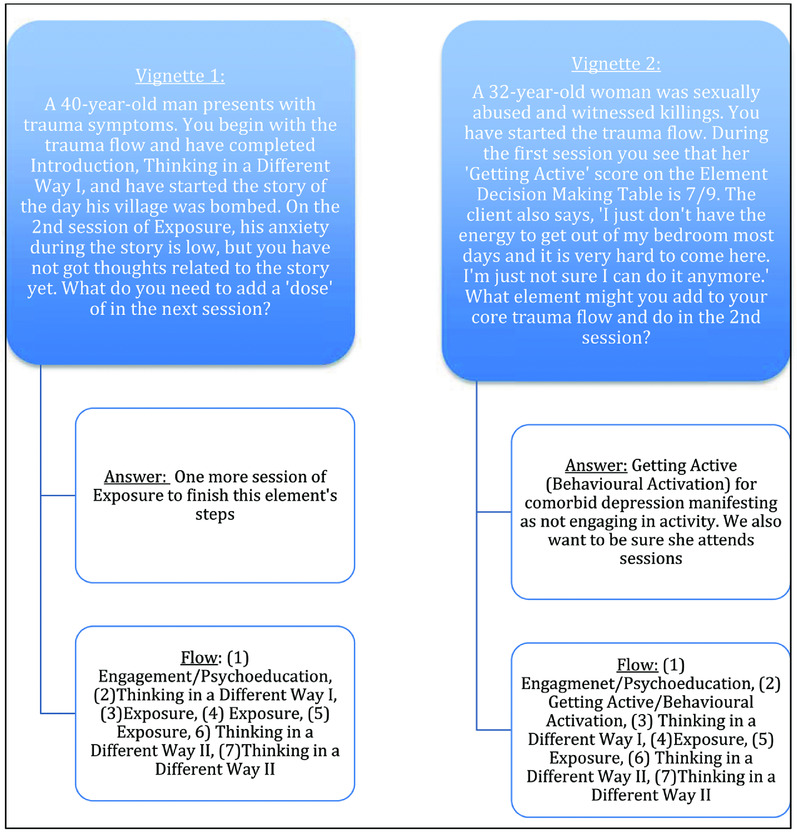
Figure 2. Vignette examples to learn element decision making

Figure 3. Abbreviated Element Decision-making table example
During the training, the local supervisors participated in additional training in supervision practices. This training included additional information on the apprenticeship model (Murray et al., Reference Murray, Dorsey, Bolton, Jordans, Rahman, Bass and Verdeli2011) how to lead a supervision group, how to coach providers in role plays, and objective reporting to the CETA trainer. Trainers also spent time explaining decision-making rules, and what would indicate ‘interference’ and thus addition of an element, or additional dosing of an existing element. At the end of the live training, all counsellors and supervisors were required to complete a CETA specific knowledge test in order to ‘graduate’ from the live training, an indication of some level of competency. This exam tests counsellors’ knowledge of specific elements and decision rules that guide intervention delivery. Counsellors who ‘graduated’ began practice groups run by local supervisors. These groups included additional role-plays of all elements, and decision-making practice. Counsellors also took on 1–2 ‘practice’ cases.
Counsellors who performed well with their initial 1–2 ‘practice’ cases, as determined by the local supervisors and trainers, were assigned clients as part of the RCTs, while those who needed more practice took on an additional case prior to seeing trial clients. Throughout both RCTs, supervisors met weekly with counsellors in a group (except in instances of safety risk), and United States-based trainers had individual weekly Skype calls with each supervisor. During supervision, counsellors provided descriptions of what happened with every case and plans for the following week.
Element decision-making
Training on decision-making of element selection, order and dose included some general rules. When a counsellor wanted to add both Relaxation and Behavioral Activation, the counsellor was guided to start with the optional element they believed would address the problem affecting the client the most. After delivery of that element, the counsellor would re-assess need via weekly monitoring scores and asking the client directly. A second decision rule was that the optional elements (Relaxation, Behavioral Activation, and SBI) were delivered after Psychoeducation and before Cognitive Coping (see Fig. 1) if need was determined at the start of treatment. If the need for one of these elements emerged during treatment, they could be added later in the flow. The general recommended dose (i.e. number of sessions) for each element was based on the literature on evidence-based treatments and our desire for treatment to be as brief as possible (see Table 1), but could be flexible based on client presentation and the client's understanding or progress on each element. Decision-making skills were taught through repeated practice of applying the criteria to different client vignettes. Working in small groups, trainees participated in an exercise in which they responded to these vignettes (client descriptions and assessment scores like Fig. 2) by selecting likely elements from a stack of cards of all CETA elements (multiple cards for each element), and then putting them in order with dosing. Trainers provided feedback and asked questions regarding rationale. Trainees also were presented with information on client response after specific elements and/or homework completion/non-completion, and then asked if they would adapt their plan, and if so, how (e.g. often needed to add one more session for an element).
In the trials, initial decision-making was done by lay counsellors, and then checked by the local supervisor and subsequently by the trainer. As long as a counsellor could explain the rationale for an element, order, or dose based on the assessment and/or the client's responses and/or behaviours and it was in line with the training, supervisors and trainers supported their decisions. Many of the counsellors made decisions that were consistent with supervisor opinion, even immediately following the training (evidence of very early learning) and others improved gradually. Some continued to need re-direction at times during the study. If a counsellor did not deliver an element correctly, the supervisor would discuss the error, role-play the correct implementation with the counsellor, and then have the counsellor re-administer the element in the following session with the client. Correction by outside trainers was minimal. For approximately the first 3 months after the training, the trainers would correct provider/supervisor decisions 20% of the time or less. Beyond the first 3 months, only one supervisor in each site continued to require corrections.
CETA participants
The current study analysed data from 92 client participants in Iraq and 145 in Thailand who received CETA from lay counsellors as part of a randomized trial. Descriptive information for all participants included in the current analysis is in Table 2. Trial eligibility differed slightly by site: in Iraq, participants experienced torture, imprisonment, or conflict-related trauma and had elevated symptoms of post-traumatic stress; in Thailand, participants witnessed or experienced at least one traumatic event related to repressive activities by the Myanmar government and met depression and/or post-traumatic stress inclusion criteria [see Bolton et al. (Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014) and Weiss et al. (Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015) for more detail]. The current analysis includes only those individuals who met inclusion criteria, were randomized to the treatment arm in both sites, and completed treatment. Treatment completion was defined as receiving the ‘finishing steps’ or wrap-up session. We restricted the sample to treatment completers because the current analysis is focused on characterizing how CETA was delivered by lay providers across the course of treatment. For non-completers, counsellors lost the ‘choice’ of giving some elements (and dose for those elements), and inclusion of these cases would incur bias in frequency statistics for elements that occur later in the course of treatment.
Table 2. Demographics and treatment needs

1 Possible scores on the symptom monitoring assessment subscales ranged from 0 ‘never/no’ to 3 ‘very often (more than five times per week)’ in Iraq and from 0 ‘none of the time’ to 4 ‘almost all the time’ in Thailand.
In Iraq, six participants were excluded from analysis because they were non-completers (7% of the n = 98 included in analysis sample); one additional participant was excluded from analyses due to non-initiation of treatment. In Iraq all non-completers were men and their average age was 50.2 years (SD = 8.3). Non-completers had an average of 8.7 weekly sessions (SD = 3.2; range 4–14). Only one person (16.7% of non-completers) dropped out before completing eight weekly treatment sessions and five out of the six clients dropped out after receiving a session of Cognitive Restructuring. In Thailand, twenty-three participants (12.6% of the 182 included in analysis sample) were defined as non-completers. An additional 14 in Thailand were excluded from analysis due to missing all weekly data on what elements were delivered (7.7% of the 182 who enrolled). In Thailand, 14 of the non-completers (n = 23) were female (60.9%) and the average age was 36.4 years (SD = 12.4). Non-completers spent an average of 4.4 weekly sessions in treatment (SD = 3.1; range 1–11). Roughly half of non-completers dropped out after completing five sessions (n = 11; 47.8%).
Analyses
Because element delivery was recorded differently at the two sites, session data are not comparable and are presented as separate studies. We calculated descriptive statistics (frequencies, means, standard deviations, range) for variables of interest, including average amount of time spent in treatment (in days), average number of total clinical sessions, and average length of treatment sessions (in minutes; results from Thailand study only).
Analyses examined how much variance in dosage for each element (i.e. number of sessions focused on an element) may have been attributable to counsellor-level characteristics versus client-level differences using multi-level models (clients nested within counsellor). We obtained intra-cluster correlation coefficients (ICCs, also known as variance partition coefficients in this context) from these models, and present them as percentage of total variance in number of sessions at the counsellor level. Our counsellor- and supervisor-level sample sizes were too small to examine whether specific individual characteristics (e.g. counsellor age, caseload size, supervisor education level) predicted variance at the counsellor level, or whether supervisor differences predicted variance in dose (e.g. counsellors nested within supervisors).
Results
Length of treatment
Among treatment completers, the duration of treatment and number of sessions attended are shown in Table 3. CETA was delivered to participants in an average of 9.9 sessions (SD = 1.8) over 93 days in Iraq and an average of 8.3 sessions (SD = 1.5) over 62 days in Thailand. Length of individual sessions was not collected in Iraq; in Thailand, sessions were 60 minutes on average (range: 41 to 93).
Table 3. Time in treatment, number of total clinical sessions, and length of treatment

Elements delivered and ‘dose’
Table 4 depicts the individual CETA elements that were delivered, the number of participants who received them, and dose (or number of sessions) of receipt for each element. As described earlier, in both RCTs, counsellors began with a ‘core flow’ due to participants’ common experience of trauma and trauma-related symptoms (see Fig. 1). Table 4 shows 100% provider compliance in both sites on delivery of core flow elements. Overall, optional elements (Relaxation, Behavioural Activation, In vivo Exposure, and, for Thailand, SBI) were delivered for a moderately small percentage of cases in both sites. Relaxation was added for 26.1% of the cases in Iraq and for only 4.2% of the cases in Thailand. Behavioural Activation was added for 13.0% in Iraq and 18.4% in Thailand. SBI was added for only 7.1% of the cases in Thailand. In vivo Exposure was delivered to only one client in Iraq and to no clients in Thailand.
Table 4. Treatment elements delivered

Different methods were used for data collection about treatment elements for Iraq and Thailand and, therefore, these data are not comparable.
1 n = 4 participants from Thailand who were considered treatment completers did not have session element data recorded. TDW, Thinking in a Different Way.
Some elements were delivered in one session fairly consistently in both sites including Psychoeducation, Relaxation, Behavioural Activation/Getting Active and Wrap-up. Delivery of Cognitive Coping/Thinking in a Different Way ranged from one to four sessions in both sites, with an average of 1.86 in Iraq and 1.77 in Thailand, slightly lower than the suggested minimum two-session dose. Imaginal exposure ranged from one to seven sessions, with a slightly higher mean number of sessions in Iraq (2.72) compared with Thailand (2.38). Cognitive Restructuring (completed after Imaginal Exposure) had a mean dose of 2.54 in Iraq and 2.14 in Thailand.
Table 5 depicts the ICCs for the delivery and dose for each element in a multi-level model framework, with client nested within counsellor. These statistics indicate the percentage of variance in number of times each element was delivered clustered at the counsellor, rather than client, level. If dosage was distributed the same by all counsellors, these ICCs would be low (near 0%); if dosage was specific to counsellors (e.g. certain counsellors selected an optional element frequently and others used it rarely), ICCs would be high. In Iraq, dose for Psychoeducation (which all clients received at least once) was more strongly attributable to counsellor-level variance (55.4%) than client-level, suggesting that certain counsellors were more likely to deliver Psychoeducation twice rather than once. In Iraq, the remaining elements had a relatively restricted range of variation due to counsellor-level variance (ICC range: 9.5 to 16.7) and were largely predicted by client-level variance. In Thailand, dose for Cognitive Coping – a necessary element that all clients received at least once – was strongly associated with counsellor-level variance (67.7%). To explain this large ICC, two out of three supervisors oversaw counsellors that delivered Cognitive Coping for an average of 2.1 sessions (range 1–4). However, counsellors under supervision with a third supervisor delivered Cognitive Coping in one session for all clients in their care. The remaining elements had a wide range of variation due to counsellor-level factors (ICC range: 2.1 to 22.0), but the wide confidence intervals around these estimates indicated that most elements largely varied at the client level due to client differences and/or measurement error.
Table 5. Percentage of variance in number of times each element delivered attributable to counsellor (n = 12 in Iraq; n = 19 in Thailand), for treatment completers only

Different methods were used for data collection about treatment components for Iraq and Thailand and, therefore, these data are not comparable.
1 Sample sizes precluded examination of percentage of variance in the number of times these components were delivered.
Figure 4 depicts the sequencing in which each element was delivered, across all participants by site. The bars represent the percentage of participants receiving each element, by session number. The horizontal axis represents potential sessions 1–13, left to right. The grey bar represents the session in which that element was delivered to the highest proportion of participants who remained in treatment. The ‘mean % of sessions’ column indicates the average percentage of sessions spent on the element. The figure reveals consistency in delivery of the ‘core flow’ treatment elements, or fidelity, in both sites. Psychoeducation was delivered most often in the first session, and occasionally in the second session, and then was not used again as a primary element. Cognitive Coping/Thinking in a Different Way I often began in the second session, typically reaching its peak in the third session such that the majority of clients received Cognitive Coping/Thinking in a Different Way I by session 3. Relaxation and Behavioural Activation/Getting Active, when used, were most commonly delivered in the second session. Imaginal Exposure began in the third or fourth sessions, reaching peak delivery (most clients receiving this element) by session 5 in both sites. Cognitive Reprocessing/Thinking in a Different Way II began as early as session 5 for some clients, was provided in a greater dose, and was typically the last element counsellors reported providing until end of treatment. Across both sites the elements delivered with the highest dose were Imaginal Exposure (27–28% of sessions), Cognitive Restructuring/Thinking in a Different Way II (25–26% of sessions), and Cognitive Coping/Thinking in a Different Way I (20–21% of sessions).

Figure 4. Sequencing of element delivery, across all participants by setting
Discussion
This paper examined the use of a modular, transdiagnostic treatment, CETA, delivered by lay counsellors in two distinct LMIC, Iraq and Thailand. Although CETA represents a simplified modular transdiagnostic approach (e.g. fewer elements, simplified decision rules put in the hands of providers), it was unknown what actual delivery would look like, and if lay counsellors would utilize the flexibility inherent in this type of transdiagnostic approach.
Overall, our results show that lay counsellors demonstrated high levels of fidelity to the ‘core flow’ (i.e. 100% provider compliance in delivery of core elements), yet also took advantage of the available flexibility. They added optional elements – albeit infrequently – and delivered elements with some variation in sequencing and some variation in dose. For nearly all elements, we found that the number of times each element was delivered was more greatly associated with the client than the counsellor, supporting the hypothesis that few counsellors favoured or avoided delivering certain elements. This suggests that counsellors (with supervision) demonstrated both fidelity and flexibility in delivery of CETA (Kendall and Beidas, Reference Kendall and Beidas2007) in both sites. These results also suggest that a common elements approach can be delivered by lay counsellors with supervision in very different low-resource and contextually challenging (ongoing conflict, illegal immigration) settings, while maintaining the basic structure of recommended elements for presenting problems.
The choice lay providers made in dosing of each element represents what is common in many short-term (e.g. 8–12 session) EBT, in which most elements are delivered in 1–2 sessions. For example, Psychoeducation is often taught to be delivered in one session. Cognitive Coping and Restructuring (Thinking in a Different Way I and II) as well as Imaginal Exposure with adults usually happens over multiple sessions. So, local counsellor–supervisor teams were able to successfully implement individual elements within the typical time frames. This could be partly due to the lack of formal mental health training among most CETA providers. Specifically, CETA providers may have followed the decision rules with more fidelity because they do not have knowledge of other treatment strategies to implement instead of or in addition to CETA. Alternatively, successful implementation could be be due to the apprenticeship model of training and supervision in which lay counsellors are monitored and supported in real time with each treatment session plan discussed a priori, reviewed, and corrected as needed.
The total number of sessions (Iraq 9.9; Thailand 8.3) suggests that large effect sizes in the trials (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey and Robinson2014; Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen and Dorsey2015) were obtained with less than the average 12-session EBT models. This may be particularly important for lower-resource settings where attending 12 sessions has been cited as a potential barrier due to challenges such as transportation and time away from livelihood-generating activities (Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary and Haydary2014b; Patel et al., Reference Patel, Chowdhary, Rahman and Verdeli2011). Future studies should continue to evaluate the cost/benefit ratio of treatments that are shorter and/or more simple with longer (8–12 sessions), already evaluated treatments for certain mental health problems or severity levels.
In Iraq it seemed that local counsellor–supervisor dyads based decisions on client presentation for all elements except for Psychoeducation. There was a cultural adaptation made by local counsellors in Iraq to add a session where a family member(s) is brought into session to hear an explanation of the treatment and give their support. This was necessary because some women required permission from husbands and/or other family members in order to participate in treatment. It could be that some counsellors valued this cultural modification, or universally used it as engagement more than others, regardless of client presentation or characteristics. In Thailand, there was a high proportion of additional variance clustering at the counsellor level in the dosing of Cognitive Work (Thinking in a Different Way I and II). Anecdotally, some counsellors reported Cognitive Coping was particularly useful for clients, and thus they may have spent more time on this element than other counsellors. Cognitive Work can also be a challenging element for counsellors, and dosing may have been related to a need to repeat the session when a supervisor felt that delivery was sub-standard.
The fact that dosage of elements seemed to vary more by counsellor in Thailand versus Iraq may in part be due to experience of the supervisors. In Iraq, the supervisors were psychiatrists, while in Thailand none of the supervisors had formal mental health training. Using their pre-existing expertise integrated with CETA training, supervisors in Iraq may have been able to give more clear directions about element selection, sequencing, and dosing. Not having supervisors with formal mental health training in Thailand, compared with Iraq, may have resulted in additional time needed for some elements for certain counsellors that were less skilled or had to repeat something due to error in delivery. Differences in variation of dosage may also be due to different methods between sites – in Iraq only the primary element was listed, whereas in Thailand, up to three elements could be listed for any one session.
Three elements were delivered frequently in both sites (Cognitive Coping/Thinking in a Different Way I, Imaginal Exposure and Cognitive Restructuring/Thinking in a Different Way II) totalling a percentage use of 72.2% in Iraq and 74.6% in Thailand. Given the significant and large effect sizes from both of these trials, future studies should examine the independent contribution of these three elements to client symptom change. Very few counsellors used Relaxation in Thailand, potentially because the counsellors did not see a need given that the study population was predominantly Buddhist, which has a well-established meditation practice. The SBI element (for alcohol use) also was used infrequently despite significant reporting of alcohol use as a problem during a formative qualitative study. This could be due to low self-report of alcohol use related to cultural beliefs.
Treatment duration was longer in Iraq than in Thailand. During the study, there were a number of bombings in Iraq, which led to frequent security check-points and limited ability to travel for counsellors and clients. This could have led to the extended time in treatment overall due to missed sessions during treatment. More participants dropped out of treatment in Thailand compared with Iraq. Although treatment non-completers were relatively similar to treatment completers in Thailand, there are several possibilities for this higher drop-out rate. During the course of the trial, major democratic changes occurred inside Myanmar and many people in the Thailand border area began returning to their country of origin. Other possible explanations include lack of symptom improvement, dissatisfaction with treatment, or other extenuating circumstances which may have led participants to terminate treatment early.
Limitations
There are several limitations of this study. First, both RCTs were restricted to an inclusion criterion of someone who had experienced torture/trauma. This led to the implementation of CETA with an initial ‘core flow’ that matched most EBTs for trauma-related problems. Our analyses would be more generalizable if RCT study inclusion criteria were broader. Still, there was variation in individual client presentation, with comorbid symptoms of trauma, depression and anxiety at baseline. Thus, despite being a trauma-affected sample, the analyses illustrate how lay providers could use a modular transdiagnostic approach to work with comorbidity – comorbidity being the ‘rule’, rather than the exception (Weisz et al., Reference Weisz, Krumholz, Santucci, Thomassin and Ng2015).
Second, these data are from two rigorous RCTs, which included intensive supervision and fidelity tracking. Counsellors were encouraged to make initial decisions about treatment delivery, which were then reviewed by a local supervisor and a CETA trainer. As it was a collaborative process, we were not able to distil independent counsellor decisions from those that were based on a recommendation by the supervisor and/or trainer. Given the limited number of supervisors, it is possible that all decisions about selection, sequencing and dosage were ultimately made at the supervisor level. Given the depth of training and skill noted in decision-making even during the live training, and our anecdotal experience as trainers on weekly calls with supervisors (who reported counsellors’ decision-making), we believe that counsellors played a substantial role in the decisions for CETA delivery. Ongoing supervision is critical to any psychological intervention, and regardless of who made the actual decision, what was ultimately delivered in the session was up to the local counsellor/supervisor teams. Although trainers reviewed each case weekly with the local supervisor, our anecdotal experience was that corrections were minimal, particularly after the first 3–5 months.
Third, small sample sizes at the counsellor level created wide confidence intervals and lack of precision in ICCs. Supervisor sample sizes were prohibitively small, allowing only for descriptive analysis. Similarly, clients were not randomly assigned to counsellors, which might upwardly bias counsellor-level ICCs for element dosage. However, these ICCs were relatively small for nearly all elements; therefore, cross-counsellor fidelity to the core flow may be even better than represented in these results.
Conclusions and future directions
This paper describes the implementation of a modular transdiagnostic treatment approach designed for use by lay counsellors in low resource settings, in two culturally different settings. Our analysis suggests that lay counsellors were able to learn decision-making processes based on client presentation and adjust treatment as needed. These results suggest delivery with fidelity (delivery of core elements) and flexibility (optional elements or dosing variation) when lay counsellors received supervision locally, and overseen by CETA trainers. Individual tailoring, in adding optional elements and flexibility in dose of elements, did not result in significantly longer treatment, as average treatment length was less than 10 sessions in each site. Despite variability in measurement, research methods and context, lay counsellors in both studies delivered this common elements treatment approach with fidelity and acceptable flexibility, demonstrating generalizability of findings across settings and methods of inquiry.
As modular transdiagnostic interventions are increasingly encouraged and utilized in LMIC, research should continue to ‘unpack’ lay counsellor delivery of these interventions. In particular, it is important to understand how counsellors make decisions about delivery based on client-level data, what counsellor-level factors might predict better decision-making, and how often counsellors make appropriate decisions independently, versus required adjustments from a supervisor or trainer. Supervision and support in the trials from which these data are drawn was high. Future research should also investigate how different and varying intensity supervision structures might co-vary with counsellor decision making in terms of achieving fidelity to core elements and appropriate flexibility.
Main points
(1) Transdiagnostic approaches are being increasingly used and studied, and CETA is a cognitive behaviourally based common elements approach developed for, evaluated and used in low and middle income countries.
(2) CETA is modular, flexible and addresses multiple problems allowing elements to be chosen based on individual client need and can vary throughout implementation in order and/or dose.
(3) There is still much to learn about how best to individually tailor modular transdiagnostic approaches to provide a degree of fidelity to existing evidence-based models along with flexibility in delivery, to obtain effective results.
(4) Lay providers in low or middle income countries are able to deliver CETA and learn the clinical decision making when supervision was provided.
Acknowledgements
We would like to acknowledge the vital support of the clinical providers, supervisors, project staff and patients who participated in this study. We particularly wish to thank both current and former staff at USAID – Victims of Torture (VOT) for their commitment to evidence-based programming as the basis for effective services.
Conflicts of interest
The authors have no conflicts of interest with respect to this publication.
Ethical statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, and its most recent revision. All authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the APA. No ethical approval was needed as this was a sub-analysis of completed and already published trials.
Financial support
This work was supported by the USAID Victims of Torture Fund (P.B., L.K.M., E.H., J.A.; grant no. DFD-A-00-08-00308-00).
Learning objectives
(1) To understand the use of transdiagnostic treatments in low and middle income countries.
(2) To understand how modular transdiagnotic treatments like CETA are used clinically.
(3) To understand the use of various elements of the CETA modular approach in two diverse contexts by lay providers.
(4) To comprehend the importance of examining which elements may function as mechanisms of action towards symptom remission.












Comments
No Comments have been published for this article.