Introduction
Dietary adequacy is crucial for children to support healthy growth and development and prevent nutrition-related diseases later in life(Reference Martins, Toledo Florencio and Grillo1,Reference Walker, Wachs and Gardner2) . However, existing international data indicate that many children fail to achieve dietary recommendations for multiple nutrients(Reference Fiorentino, Landais and Bastard3–Reference Lee and Park5). Thus, abundant research has been conducted to understand factors that could influence eating behaviours and dietary intake of children.
Recent studies suggest that dietary intake and preferences of children are influenced by gender, but findings in this regard were mixed. Lytle et al. observed similar dietary patterns for boys and girls in the USA(Reference Lytle, Seifert and Greenstein6). In Europe, several studies reported that girls tend to consume more fruits than boys and have a stronger preference for vegetables(Reference Le Bigot Macaux7–Reference Cooke and Wardle10), whereas boys tend to have a greater preference for meat, processed meat, eggs and high-sugar and energy-dense foods than girls(Reference Cooke and Wardle10). In a study conducted among Polish pre-schoolers, significant gender differences in multiple nutrients were observed, such as protein, saturated fat and carbohydrate(Reference Merkiel-Pawlowska and Chalcarz11). However, research studies investigating gender differences in nutrient intakes among school-aged children are scarce.
Children are particularly vulnerable to dietary inadequacy due to higher requirements associated with physiological development and growth(Reference Walker, Wachs and Gardner2). Furthermore, many children demonstrate a strong preference for some foods, while rejecting others(Reference Kutbi12). In particular, school-aged children tend to demonstrate independence in selecting food choices(Reference Bassett, Chapman and Beagan13). These dietary behaviours may limit dietary variety and, therefore, affect dietary adequacy. In the Middle East, children's diet has been shifted from traditional dietary patterns to a Westernised diet characterised by high intakes of fast-food, energy-dense snacks and sugar-sweetened beverages(Reference Amin, Al-Sultan and Ali14,Reference Musaiger, Hassan and Obeid15) . Alongside, nutrient inadequacies have been documented, with suboptimal intakes of fibre, iron, zinc, calcium and vitamin D and excessive intakes of sugar, fat and saturated fat(Reference Musaiger, Hassan and Obeid15). However, dietary intake studies in the Gulf countries, particularly in Saudi Arabia, are scarce. In fact, the need for dietary data in Saudi Arabia has been previously suggested(Reference Nasreddine, Kassis and Ayoub16). Hence, the present study aimed to (1) evaluate the nutrient intake of Saudi children in relation to dietary recommendations and (2) investigate gender differences in nutrient intake. Our findings will inform policies and guide intervention programmes aimed at promoting healthy dietary habits early in life.
Materials and methods
Study sample
We aimed to recruit at least 176 boys and 176 girls based on the sample size calculation method suggested by Hulley et al., with 95 % confidence level, 80 % power, mean energy intake of 1200 ± 350 kcal/d with a minimum of 10 % difference in energy intake between boys and girls (obtained from a pilot of 36 children which has been excluded from the total sample) and standardised effect size of 0⋅34(Reference Hulley, Cummings and Browner17). Data were collected between October 2020 and February 2021. Mothers of school-aged children (6–12 years old) were invited to participate in the present study using social media channels. An online link included information on study objectives and protocol and consent for participation. The mothers were requested to answer questions on the sociodemographic characteristics of the child (age, gender, region of residence, maternal and paternal education status, maternal age and employment status, and paternal involvement in child feeding). We also asked the mothers about the appropriate date and time for communication to collect the dietary data of the child. Data of healthy Saudi children aged 6–12 years were included. The exclusion criteria include non-Saudi children and children with food allergy or any medical health condition. The final analyses included data of 424 Saudi children. The present study was conducted following the guidelines laid down in the Declaration of Helsinki. The study protocol was approved by the Faculty of Applied Medical Sciences Ethics Committee of King Abdulaziz University (FAMS-EC-2020-0010). Digital informed consent was obtained from all study participants.
Dietary assessment
The assessment of dietary data was conducted using a single 24-h dietary recall within 2 weeks from survey data collection. A subsample of 168 children (39⋅6 %) was randomly selected to report three non-consecutive 24-h recalls (two weekdays and one weekend day). The within-person mean of the three 24-h dietary recalls was calculated and used along with the single 24-h recall data for the other children to estimate the mean intake of the total sample(Reference Tooze18). We aimed in the present study to evaluate nutrient intake from dietary food sources. Thus, we did not collect data pertaining to supplement use. A reminder text message has been sent to each mother a day before the scheduled time. During the telephone interview, mothers were educated on how to express the amount and type of food consumed by the child. We also shared pictures of serving tools to further assist in estimating the portion size of each food consumed. Mothers were requested to have the child and persons responsible for child feeding nearby and participate in the interview.
Dietary data were entered into a nutrient analysis software (Nutritics version 5.09, Dublin, Ireland) to evaluate intakes of energy, macro- and micronutrients based on Arabic foods and popular Saudi/Gulf recipes. If a food recipe was not available, information was inserted manually based on standardised recipes and later validated by two registered dietitians. Nutrient intakes of the subsample that reported three 24-dietary recalls (n 168) were later used to determine proportions of children who met the dietary recommendations. Given that no specific nutrient recommendations have been established for the populations in the Gulf countries, nutrient intakes of the children were compared with the U.S. and Canada's Dietary Recommended Intakes (DRIs), which have been published by the Food and Nutrition Board of the Institute of Medicine. In fact, the U.S./Canada DRIs have been widely used across the multi-ethnic populations(Reference Morales-Suárez-Varela, Rubio-López and Ruso19–Reference Retondario, Silva and Salgado21). Mean intakes of phosphorus, magnesium and vitamins E, C and B12 within the Estimated Average Requirements (EARs) were used to determine proportions of children with adequate nutrient intake. Mean intakes of dietary fibre, sodium, potassium, calcium and vitamin D at or above the adequate intakes (AIs) were used to determine if the children were meeting the AI(22,23) . Furthermore, mean intakes of cholesterol and saturated fat (>300 mg and >10 % of total energy intake, respectively) were used to identify proportions of children exceeding the recommendations of the American Academy of Pediatrics(Reference Committee on nutrition24).
Statistical methods
Descriptive statistics were expressed as frequency (percentage), median (interquartile range) and mean ± standard deviation. The Mann–Whitney test was used to compare the intakes of nutrients for children reporting single 24-h dietary recall with the intake of children reporting three 24-h dietary recalls and to examine differences in energy and nutrient intakes by gender. The χ 2 test was used to evaluate gender differences in sociodemographic characteristics and proportions of children with nutrient intake at or above the DRI requirements (EAR or AI). To evaluate gender differences in sociodemographic characteristics, α = 0⋅050 was used to infer significance. Bonferroni adjustments for multiple testing in dietary intake was performed; gender differences in dietary intake were determined to be significant at α = 0⋅003, whereas gender differences in proportions of children meeting the DRI requirements were set at α = 0⋅007. All statistical analyses were performed using two-sided tests carried out by the Statistical Packages for Social Sciences (SPSS) version 24.0 (Armonk, NY, USA).
Results
Sociodemographic characteristics of children
Approximately half of the children were boys (49⋅5 %, n 210). Sociodemographic characteristics of the sample are presented in Table 1. The mean age of boys and girls included in the present study were 8⋅58 ± 1⋅86 and 8⋅76 ± 1⋅84 years old, respectively. Three-quarters of the mothers (75⋅2 %, n 319) and two-thirds of fathers (63⋅2 %, n 268) had a college degree or higher. The majority of fathers were involved in child feeding (76⋅9 %, n 223). No significant gender difference was observed in the proportion of children by the groups of sociodemographic variables (P > 0⋅050).
Table 1. Number (proportion) of children by gender and sociodemographic characteresticsa

a Data are presented as number (proportion).
Dietary intake of children
Intakes of nutrients for children reporting single 24-h dietary recall and children reporting three 24-h dietary recalls were all similar (P > 0⋅050). The mean energy intake of the total sample was 1312 ± 348 kcal, with a median intake of 1247 kcal (1079–1482 kcal). Mean energy intake of boys aged 6–8 years old (1329 ± 342 kcal) did not statistically significantly differ than that of girls (1298 ± 333 kcal), P = 0⋅645 (Fig. 1). Similarly, the mean energy intake of boys aged 9–12 years old (1366 ± 372 kcal) did not statistically significantly differ than that of girls (1261 ± 341 kcal), P = 0⋅055.

Fig. 1. Distribution of estimated energy intake by age and gender (n 424): (a) estimated energy intake of boys by age; (b) estimated energy intake of girls by age.
Macronutrients’ contribution to total energy intake by children's age and gender are presented in Fig. 2. No significant difference was observed in the mean proportions of macronutrient intakes between boys and girls (P > 0⋅003), as shown in Table 2. Similarly, mean intakes of macro- and micronutrients were not found to be statistically significantly different in boys than girls (P > 0⋅007).
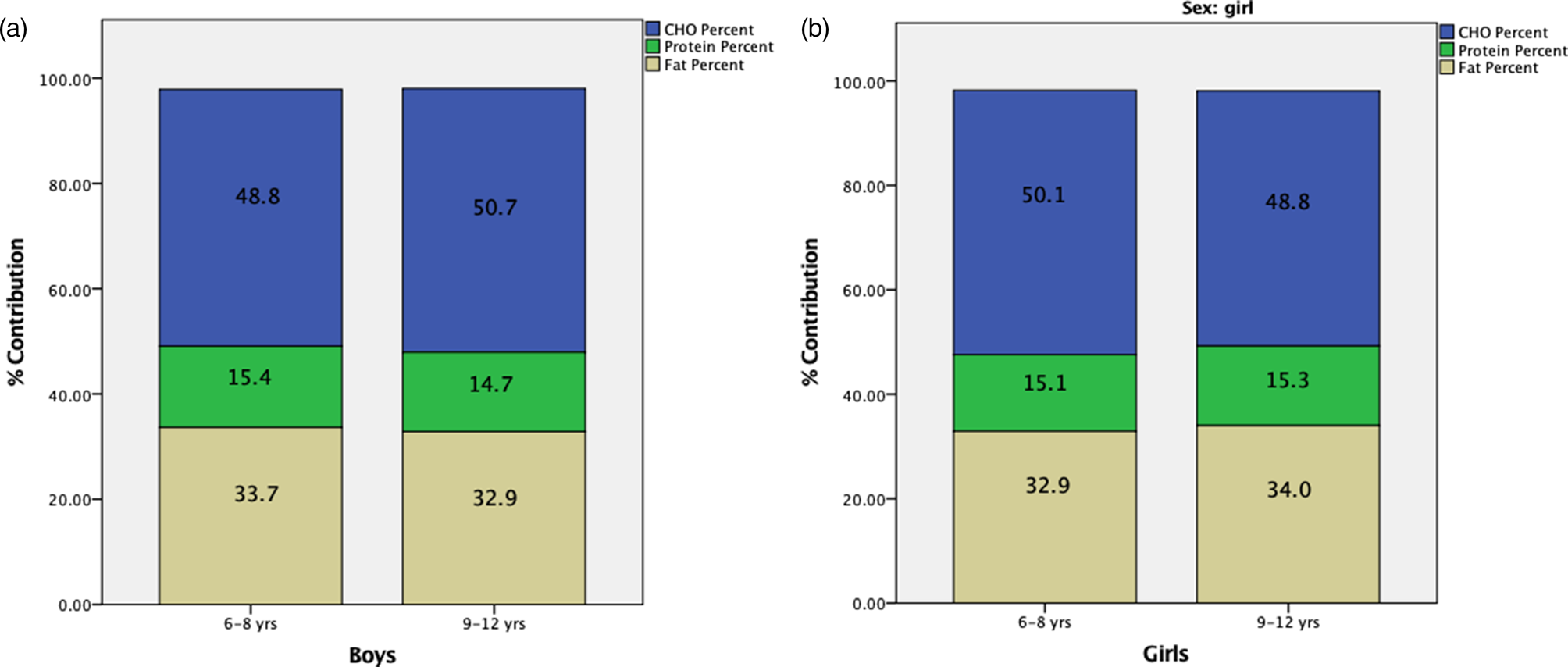
Fig. 2. Macronutrients’ contribution to total energy intake by child gender and age (n 424): (a) contribution of macronutrients of boys by age; (b) contribution of macronutrients of girls by age.
Table 2. Dietary intakes of children stratified by child age and gender

Significance was set at α = 0⋅003 based on Bonferroni correction.
Assessment of children's nutrient intakes in relation to DRI requirements
To estimate the number of children meeting the EAR or the AI requirement of each nutrient, only data of children who reported multiple dietary recalls were included (Table 3). Thus, the total sample included 168 children, wherein 50 % of the sample consisted of boys (n 84). No gender differences in proportions of children meeting the DRI requirements were observed (P > 0⋅007).
Table 3. Differences by gender in the number (proportion) of children meeting the DRI requirements, based on a subset of the sample (children reporting three 24-h recalls)

AI, adequate intake; DRI, Dietary Recommended Intake; EAR, estimated average requirement.
Significance was set at α = 0⋅007 based on the Bonferroni correction.
Over two-thirds of the children (78⋅0 %) had an adequate usual intake of vitamin B12 (n 131), and over half of the sample had AIs of vitamin C (68⋅5 %, n 115) and phosphorus (56⋅0 %, n 94). On the other hand, our data indicated that low proportions of children were having adequate usual intakes of magnesium (45⋅8 %, n 77) and vitamin E (9⋅52 %, n 16).
The majority of children in our sample (92⋅9 %, n 156) met the AI for sodium and 50⋅6 % met the AI for vitamin D (n 85). Only small proportions of children met the AI for calcium (5⋅36 %, n 9), potassium (2⋅98 %, n 5) and fibre (1⋅19 %, n 2). Cholesterol and saturated fat intake exceeded the limits of 300 mg and 10 % of total energy intake by 13⋅7 % (n 23) and 80⋅4 % (n 135) of the sample, respectively.
Discussion
It is well recognised that dietary adequacy is indispensable to promote the growth and development of children. This study aimed to evaluate the nutrient intake of Saudi children and investigate gender differences in relation to dietary recommendations. Dietary intakes of boys and girls were similar. Many children had inadequate usual intakes of vitamin C and E, phosphorus and magnesium, and most children had usual intake below the AI for calcium, potassium and fibre. On the other hand, high intakes of cholesterol and saturated fat were observed. These findings suggest an urgent need to identify barriers to high-quality diet and to develop evidence-based interventions to promote optimal dietary efficacy.
Although previous studies indicated that food choices and dietary patterns might vary by child's gender(Reference Le Bigot Macaux7–Reference Cooke and Wardle10), our data showed similar nutrient intakes for boys and girls. According to existing data, unhealthy food choices are highly prevalent among Saudi children, demonstrated by daily consumption of sweets, sugar-sweetened beverages and energy-dense foods(25). As such, it is possible that the lack of variability in nutrient intake is due to similarities in dietary habits or patterns. Further studies are needed to understand dietary behaviours of Saudi children. Specifically, future research may explore determinants of nutrient intake and food choices among Saudi children.
Across ages and genders, macronutrient distribution was consistent with the recommended ranges(26). Carbohydrate was the main source of energy, followed by fat and protein. The American Academy of Pediatrics recommends that children's intake of cholesterol and saturated fat should be below 300 mg and 10 % of total energy intake, respectively(Reference Committee on nutrition24). In accordance with international data(Reference Amin, Al-Sultan and Ali14,Reference Musaiger, Hassan and Obeid15) , high cholesterol and saturated fat intakes were observed among children in our sample. These observations support the previously reported data that show high consumption of fast food among Saudi children(Reference Amin, Al-Sultan and Ali14,Reference Musaiger, Hassan and Obeid15) .
In the present study, most children had inadequate fibre intake and consumed low amount of potassium. Dietary fibre and potassium could be obtained from the consumption of whole grains, fruits and vegetables, which are often associated with high-quality diet and dietary variety(Reference Vadiveloo, Dixon and Mijanovich27). Dietary fibre has been particularly recommended for its health promotion characteristics(Reference Haack and Byker28). However, most Saudi children do not achieve the optimal amount of fruit and vegetables. A study conducted among 725 children in Saudi Arabia reported that 69 and 71 % of the sample were not consuming fruits and vegetables, respectively, on a daily basis, whereas only 0⋅9 % were meeting the recommendations of fruit and vegetable consumption(29).
The home food environment has a paramount effect on the consumption of fruits and vegetables among children(Reference Yeh, Ickes and Lowenstein30). The limited availability and accessibility to fruits and vegetables at home can be a major determinant of low fruits and vegetable intake(Reference Yeh, Ickes and Lowenstein30). Additionally, the low price per calorie for unhealthy food options, such as sugary foods and drinks in high-income countries, may also limit the consumption of healthy food options, such as fruits and vegetables, compared to unhealthy foods(Reference Headey and Alderman31).
AIs of dietary calcium and vitamin D in children are important for normal bone mineralisation and rickets prevention(Reference Stallings32). In the present study, the mean calcium intake appeared to be very low compared to the AI for calcium. Very large proportions of school-aged children consuming an inadequate amount of calcium were also observed in several studies(Reference Fiorentino, Landais and Bastard3,Reference Abizari, Buxton and Kwara33,Reference Al-Musharaf, Al-Othman and Al-Daghri34) . A sample of Saudi elementary school children had a mean calcium intake that represented ≤60 % of the RDA requirement and a mean vitamin D intake of approximately 23 % of the RDA(Reference Al-Musharaf, Al-Othman and Al-Daghri34). Another study investigated the association of calcium intake with children's diet observed a significant positive strong correlation with the consumption of milk and dairy products, whereas a very weak correlation with non-dairy beverages was reported(Reference Storey, Forshee and Anderson35). Further, a study by Alsubaie showed that approximately 32 % of children aged between 7 and 12 years did not consume milk or dairy products on a daily basis, whereas only 1⋅9 % were adherent to dairy intake recommendations(29). On the other hand, the mean usual intake of vitamin D among children in the present study exceeded the AI, suggesting that the expected prevalence of inadequacy is low(22). Nonetheless, high prevalence of vitamin D deficiency has been frequently documented. For instance, a study conducted by Mansour and Alhadidi evaluated the prevalence of vitamin D deficiency among Saudi children in Jeddah, Saudi Arabia, and reported a prevalence of 54⋅9 %(Reference Mansour and Alhadidi36). Given that diet of the Saudi population has been frequently reported to be low in vitamin D(Reference Al-Musharaf, Al-Othman and Al-Daghri34,Reference Mumena and Kutbi37) , supplementation of vitamin D may require further consideration.
Food sources of phosphorus and magnesium include a variety of protein foods, such as meats, poultry, seafood, eggs and legumes. However, the dietary data indicate inadequate intake of these nutrients among children of the older age group (9–12 years old), whereas the younger group (6–8 years old) were exceeding the EAR for dietary phosphorus and magnesium. This is most likely due to the higher requirements for the older group which make it more difficult to achieve(38). Similar findings have been reported by Nasreddine et al., of which large proportions of children in Saudi Arabia did not meet the respective requirements for these nutrients(Reference Nasreddine, Kassis and Ayoub16).
Due to its negative impact on physical and cognitive development in children, undernutrition associated with suboptimal intake of micronutrients must be addressed(Reference Walker, Wachs and Gardner2). Dietary adequacy can be achieved by consuming a balanced diet containing diverse foods, which may increase the potential to obtain a variety of nutrients(Reference Ruel39,Reference Zhao, Yu and Tan40) . Thus, intervention programmes to promote dietary variety may improve the nutritional status of children. Providing milk and dairy products and calcium-fortified foods and beverages may help children to achieve the optimal intake of calcium and phosphorus. When adequate calcium is not achieved, health professionals must consider recommending calcium supplements to maintain bone health. Additionally, fibre intake among children was found to be insufficient, whereas high intakes of saturated fat and cholesterol were observed. Interventions should focus on reducing intakes of highly processed foods and snacks, fried and fast foods, and processed meats and encourage the consumption of fibre-rich foods such as fruits and vegetables, whole grains, nuts and seeds. Children may also benefit from nutrition-based curriculum programmes to promote fruit and vegetable intakes and enhance children's diet.
The present study is one of the first to evaluate the dietary intake of Saudi children and gender differences, responding to the gap in the literature and guiding future research and intervention programmes. Even though dietary assessment has been conducted using phone interviews, studies suggest that telephone-administered dietary data produce acceptable estimates of nutrient intakes(Reference Posner, Borman and Morgan41). However, the study is limited by the convenient sampling technique, as only participants who have access to social media were recruited. Thus, our finding could be only generalisable to children of mothers with access to social media platforms. Based on current data, 96 % of the Saudi population has internet access, and 25 million Saudis are active users of social media(42,43) . Yet, future studies with systematically randomly sampled children are needed to determine the generalisable to all Saudi children.
Conclusion
In summary, nutrient intakes of children were similar and did not vary by gender. The dietary data showed micronutrient inadequacies in Saudi children, with suboptimal intakes of key nutrients including fibre, calcium and phosphorus. Our findings should guide future research to further investigate barriers for optimal micronutrient intakes among Saudi children and factors. Results of the present study can serve as baseline data for fortification programmes and will inform policy-makers and other stakeholders, including funding agencies and non-governmental organisations, to address barriers to optimal nutrition and to develop culturally tailored evidence-based intervention programmes aimed at enhancing the nutritional health of Saudi children.
Acknowledgments
The author thanks all members of the Dietary Intake of Saudis project for their contribution to data collection. The author specially thanks Fatima Abdulhakeem annd Najwan Jannadi from the Nutrition Assessment Lab for their support during dietary data entry.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Informed consent was obtained from all subjects involved in the study.
The data used to support the findings of this study are available from the corresponding author upon request.
The author declares no conflict of interest.







