According to the 2017 Global Burden of Disease study, headache is the second most prevalent disorder as well as the second leading cause of years lost to disability. 1,2 Diagnosis and management of common headache disorders is critically important for physicians, irrespective of specialty. Reference Lipton and Stewart3 Yet headache disorders remain under-diagnosed, misdiagnosed, and undertreated, resulting in poor patient satisfaction, poor patient outcomes, opioid misuse, medication overuse, as well as unnecessary imaging studies and emergency department visits. Reference Lipton and Stewart3,Reference Ford, Foster, Stauffer, Ruff, Aurora and Versijpt4
Headache didactics are offered in many neurology residency programs across the country, but one study found that only 19 neurology programs in the United States offered a headache clinic to their residents. Reference Ahmed and Faulkner5 The same study showed that there is discordance between program and chief residents’ views as to whether residents are adequately prepared to manage a population of patients who suffer from primary headache disorders at the time of graduation. Reference Ahmed and Faulkner5 Dedicated clinical experiences from experts in their respective fields can be an invaluable experience for learners, and ongoing exposure to this field of headache should be encouraged during a resident’s training prior to graduation.
University of Toronto’s postgraduate training program in neurology is one of the largest training programs in North America, with a total of 35 postgraduate trainees covering 4 core quaternary acute and ambulatory care hospitals across Toronto. Clinical rotations in headache medicine became available in 2013 after Dr Christine Lay founded the Centre for Headache at Women’s College Hospital and since its inception, the number of trainees undertaking the formalized headache elective has grown. The clinic serves a large catchment area and sees over 1,200 patients per year. Reference Lay, Lawler and Lagman-Bartolome6
The goal of this quality improvement study was to evaluate the association between a clinical rotation in headache medicine and the self-reported knowledge in managing headache disorders in non-neurology trainees, and core clinical competencies of neurology trainees. We hypothesized that resident trainees regardless of specialty will subjectively improve their headache knowledge and management of common headache disorders. We also hypothesized that neurology residents will objectively improve their common headache knowledge post-rotation.
This is a single-group pre-post design, quality improvement study that was conducted at the Centre for Headache at Women’s College Hospital, Toronto. The study enrolled all residents rotating through the clinic regardless of specialty or duration but excluded residents who had previously rotated through the clinic. Residents were in various stages of their training at the University of Toronto, as well as outside institutions. Written informed consent was obtained and resident enrollment began in October 2018 and ended March 2020 (due to the COVID-19 pandemic, many outpatient rotations were halted with residents re-deployed to inpatient settings).
In Canada, the neurology residency program is a direct-entry 5-year program. Adult and pediatric neurology residents participated in the quiz portion of the study that comprised postgraduate trainee years (PGY) 1-5. We excluded other residents such as family medicine, anesthesia, obstetrical, and internal medicine residents from the quiz as the questions were based on the competencies designed by the neurology program and not necessarily in-line with other programs objectives.
Assessment tools were pretested with 2 staff and 10 residents and revised based on feedback.
Resident Questionnaire: All participants were asked their gender, level of training, and specialty. Residents were asked pre- and post-rotation questions anonymously about their knowledge of headache disorders, headache medications, and therapy. Other areas of interest were comfort level in doing nerve blocks and Onabotulinum toxin injections. An improvement was determined based on whether a resident’s score increased by 1-point on a 4-point Likert grading scale (1 is “poor” and 4 is “excellent”) post-headache rotation. Residents were also asked if their interest in headache medicine had changed, whether they would pursue a fellowship in headache (yes/no) and if they would recommend this elective to their colleagues (yes/no).
Resident Quiz: The quiz was based on the core competencies proposed by the Royal College of Physicians and Surgeons of Canada 7 and the University of Toronto adult neurology program. It consisted of 10 multiple-choice questions. Residents were not able to record the questions, nor were they provided the answers or feedback. They were asked to refrain from sharing the questions with their colleagues to maintain the integrity of the questions. The quiz was developed by the author and reviewed by faculty with formal headache medicine training. If a resident improved their quiz score post-headache rotation that was deemed as a positive outcome.
Paired Wilcoxon rank sum test was used for comparison of pre- and post-scores, statistically significant differences as p < 0.05.
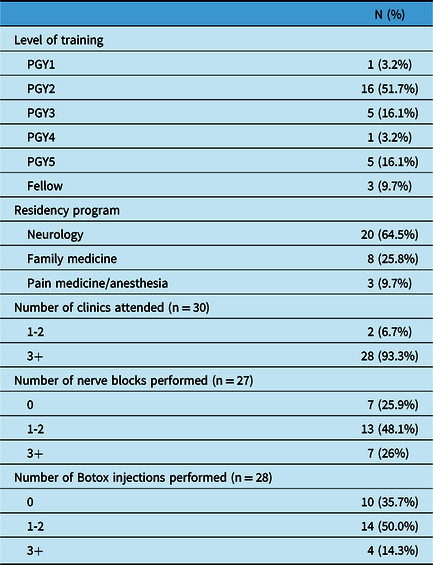
A total of 59 residents consented to participate, and 31 (52.5%) completed all surveys. From these 31 participants, 64.5% (n = 20) were neurology residents, 25.8% (n = 8) were family medicine residents, and 9.7% (n = 3) were pain medicine/anesthesia residents. The residents displayed various levels of training with 3.2% (n = 1) PGY1, 51.7% (n = 16) PGY2, 16.1% (n = 5) PGY3, 3.2% (n = 1) PGY4, 16.1% (n = 5) PGY5, and 9.7% (n = 3) fellows (Table 1). Out of 31 residents who completed the survey, 6.7% (n = 2) attended 1–2 clinics, 33.3% (n = 10) attended 3–5 clinics, and 60% (n = 18) had attended greater than 5 clinics during their rotation. Out of 27 residents who provided responses, 25.9% (n = 7) performed 0 nerve blocks, 48.1% (n = 13) performed 1–2 nerve blocks, 22.2% (n = 6) performed 3–5 nerve blocks, and 3.8% (n = 1) performed more than 5 nerve blocks. Out of 28 residents who provided responses, 35.7% (n = 10) performed 0 Onabotulinum toxin injections, 50.0% (n = 14) performed 1–2 Onabotulinum toxin injections, 10.7% (n = 3) performed 3–5 Onabotulinum toxin injections, and 3.6% (n = 1) performed more than 5 Onabotulinum toxin injections.
Table 1: Participant characteristics (n = 31)
There was significant improvement in self-reported measures of headache knowledge, and statistically significant improvement in overall knowledge, measured using case-based quizzes [mean score (SD) pre- vs. post-rotation score; 7.1 (1.4) vs. 7.9 (1.5), p = 0.003] (Figure 1). After the rotation, the mean scores showed statistically significant improvement of 3.19 (0.543) from 2.35 (0.661), for knowledge of headache disorders (KHD), p < 0.001, 3.19 (0.477) from 2.13 (0.619) for knowledge of headache medications/therapy (KHM), p < 0.001, 3.13 (0.670) from 2.13(0.619) for comfort in treating patients with headache (CPH), p < 0.001, 2.16 (0.860) from 1.13 (0.341) for comfort in doing nerve blocks (CNB), p < 0.001 and 1.90 (0.759) from 1.06 (0.250), for comfort in doing Onabotulinum toxin injections (CBI), p < 0.001 (Figure 2). These metrics measure confidence in knowledge, not the actual knowledge per se.
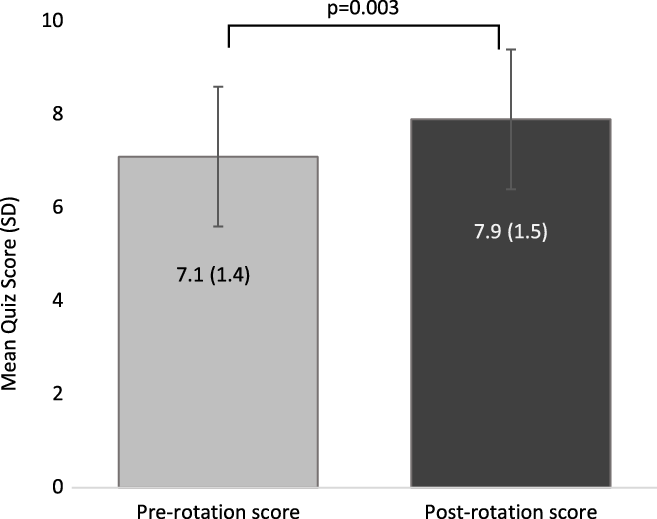
Figure 1: Overall knowledge of headache medicine measured by a case-based quiz represented by pre- and post-rotation quiz scores. Mean plus standard deviations are shown.

Figure 2: Resident self-reported improvement in headache medicine knowledge (KHD), management (KHM), comfort in treating headache patients (CPH) in doing procedures (nerve blocks (CNB) and injections (CBI)) post-headache rotation. Mean and standard deviations are shown.
This study looked at whether the level of training impacted the post-rotation score, and no statistically significant differences were seen in the post-rotation scores for KHD, KHM, and CPH. We also looked at the relationship between the number of clinics attended or the specialty of the residents and its possible impact on the post-rotation score, and this was found not to be statistically significant.
All (100%, n = 31/31) residents felt that they improved their clinical approach to patients with headache, 100% (n = 23/23) indicated that they would recommend this elective to their colleagues, and 73.9% (n = 17/23) felt that their interest in headache medicine changed following the rotation compared to their previous opinion, and 52.2% (n = 12/23) of residents which were all neurology residents also indicated they would consider pursuing a headache fellowship in the future.
The results of this study found that overall, residents who rotated through the Centre for Headache experienced an improvement in their self-perceived knowledge of headache medicine and comfort in treating patients with headache.
The aim of the study sought to evaluate residents rotating through headache medicine clinics on their knowledge and comfort in treating headache patients; however, this study had its limitations. Data were obtained from a single clinic at a single institution, and study enrollment was slow at times with periods of fewer residents on rotation or residents not consenting to participate. The headache quiz consisted of 10 questions and due to time constraints it is unlikely to be detailed enough to provide a reliable evaluation of whether residents understood all the core concepts of headache medicine. There was a statistically significant improvement in overall knowledge, yet we recognize that the differences seen were small and therefore cautious interpretation is needed. The fact that residents took the quiz twice could in of itself improve resident’s score, and it can also be difficult to interpret the reliability of self-evaluation as it does not always correlate with actual clinical capabilities. Reference Lai and Teng8 Clinical skills examination of competencies would better determine whether there is a correlation with self-evaluation, which will be considered in the future.
This study highlights that resident trainees find formal headache medicine training beneficial outside of the didactics they receive during their residency. The Women’s College Centre for Headache clinical experience could be an elective that can successfully be incorporated into other neurology residency programs. This study shows the importance of dedicated headache medicine rotations in neurology programs and the opportunity for non-neurology residents to gain important exposure to headache medicine. There is a growing body of literature that consistently tells us that graduating neurologists do not feel properly equipped with the tools to treat headache disorders comfortably. It is imperative that we provide the adequate resources and education to our postgraduates for them to effectively manage their patients.
Acknowledgements
The authors thanks their Headache Centre administrator Toni Morrison for her assistance in administering and collecting all the questionnaires from the residents. The authors would also like to thank Dr Manav Vyas for his contributions.
Statement of Authorship
Conception of study: CT, CL, and AMLB. Design of study: CT, CL, and AMLB. Data collection and analysis: CT and HP. Writing of manuscript: CT, HP, CL, and AMLB. Critical review of manuscript: CT, HP, CL, and AMLB.
Conflict of Interest
Ana Marissa Lagman-Bartolome participated in advisory boards for Lundbeck, TEVA, Eli Lilly, and Novartis; however, fees were submitted to Women’s College Hospital, Department of Medicine. Christine Lay participated in advisory boards for Lundbeck, TEVA, Eli Lilly, and Novartis; however, fees were submitted to Women’s College Hospital, Department of Medicine. All other authors declare no other relationships or activities that could appear to have influenced the submitted work.
Ethics Approval
This study was approved by the Women’s College Hospital Research Ethics Board (REB # 2018-0129-E).





