In China, prevalence studies have revealed that 6.71 per 1000 people in the cities and 4.13 per 1000 people in the countryside experience schizophrenia; there are an estimated 4.5 million people with the disorder in China, of whom 90% live with their families (Reference Cheng, Shen and ZhangCheng et al, 1998). The mental healthcare system is largely institutional, and in the community the burden of care falls mostly on the shoulders of families through family ties and expectations. Nurses and doctors are the main carers in hospitals, but there was no report in the refereed literature of studies being conducted by nurses in China to identify the effect of patient or family education on people with schizophrenia.
Since the early observations by Brown et al (Reference Brown, Monck and Carstairs1958) that people with schizophrenia discharged to live in boarding-houses or with siblings fared better than those discharged to live with parents or spouses in terms of relapse, several landmark studies have demonstrated that there is now little doubt that family interventions in schizophrenia are effective in postponing psychotic relapse over periods of up to 2 years (Reference Anderson and ReissAnderson & Reiss, 1982; Reference Falloon, Boyd and McGillFalloon et al, 1985; Reference Leff, Kuipers and BerkowitzLeff et al, 1985; Reference Hogarty, Anderson and ReissHogarty et al, 1986; Reference Tarrier, Barrowclough and VaughnTarrier et al, 1988; Reference Pekkala and MerinderPekkala & Merinder, 2003; Reference Pharoah, Mari and StreinerPharoah et al, 2003). Research on family management of schizophrenia is in its infancy in China, but several studies have focused on development of education programmes and choice of outcome measures (Reference Xiong, Phillips and HuXiong et al, 1994; Zhang et al, Reference Zhang, Wang and Li1994, Reference Zhang, He and Gittleman1998, Reference Zhang, Zhao and Shen2000). Briefly, all the studies were designed with control groups and used standard diagnostic criteria such as DSM–III–R (American Psychiatric Association, 1987), or the Chinese Classification of Mental Disorders (CCMD–II–R) (Chinese Medical Association, 1995), which divides mental disorders into ten categories. These studies included either individual or group psychoeducation, often combined with antipsychotic drug treatment. There was marked reduction in relapse rates, rehospitalisation and the level of psychotic symptoms, and an enhancement of patients’ quality of life and social functioning, with an improvement in family relationships and social environment. The studies are not recent and none was conducted by nurses.
Our aim was to conduct a longitudinal experimental study that examined the effect of patient and family education on families’ knowledge about schizophrenia, and on patients’ symptoms, psychosocial functioning, adherence to medication regimens and relapse rates.
METHOD
Study design
We adopted a pre-test–post-test experimental design with a target population of people admitted to hospital for treatment of non-acute schizophrenia, and their families. The hospital was a major psychiatric hospital in Beijing with 980 beds and an occupancy rate of 104%.
To avoid contamination between the two arms of the study, wards were selected rather than individuals. The hospital had ten wards that suited the inclusion criteria: eight general adult wards (four male wards and four female wards) were selected for the study, and by random assignment two male wards and two female wards were selected to be control wards and the other two male wards and two female wards to be experimental wards. When patients meeting the inclusion criteria were routinely admitted to the wards where the study was conducted, they and their families together were fully informed about the study and asked if they would agree to participate. One in five families (either patient or family members or both) refused to do so, and in these cases the patient was excluded from the study but remained in the ward. The purpose and the procedures of the study were described to those who agreed to take part, and their questions were answered. The rights of the participants were explained to them and their written consent was obtained.
Sample
Patients were included in the study on the basis of their CCMD–II–R diagnosis and two inclusion criteria: age 16–65 years, and living with a family member at least 3 months prior to the current hospital admission. Exclusion criteria were evidence of learning disability, presence of known organic mental disorder and significant or habitual drug or alcohol use.
According to the sample size estimate for differences in proportion with power of 0.80, and treatment group relapse rate around 12% and control group around 40% in previous studies (Reference Birchwood, Spencer, Maj and SartoriusBirchwood & Spencer, 2000), the approximate sample size in each group should be 40. Finally, 101 patients with schizophrenia (and their families) were selected. There was no difference in the education level, working experience and professional position of physicians and nurses among the eight wards.
Outcome measures
Five outcome measures were used.
-
(a) Knowledge about schizophrenia of relative: this was assessed using the Chinese version of the Knowledge about Schizophrenia Interview (KASI; Reference Barrowclough and TarrierBarrowclough & Tarrier, 1992), which contains six sections, each measured on a scale of 1 to 4.
-
(b) Psychotic symptoms of patient: assessed with the Chinese version of the Brief Psychiatric Rating Scale (BPRS; Reference Overall and GorhamOverall & Gorham, 1962; Reference Zhang, He and GittlemanZhang et al, 1998), an 18-item, five-factor scale rated from 1 to 7.
-
(c) Overall function of patient: assessed with the Chinese version of the Global Assessment Scale (GAS; Reference Endicott, Spitzer and FleissEndicott et al, 1976; Reference Zhang, He and GittlemanZhang et al, 1998), a scale of 10-point intervals from 1 to 100.
-
(d) Psychosocial behaviour of patient: assessed with the Chinese version of the Nurses’ Observation Scale for Inpatient Evaluation (NOSIE; Reference Honigfeld and KlettHonigfeld & Klett, 1965; Reference Zhang, He and GittlemanZhang et al, 1998), a 30-item, five-factor scale.
-
(e) Relapse rate (rehospitalisation or BPRS score greater than 5) and medication compliance (interruptions of 1 week or change against advice on a scale of 1–4).
All the instruments have established reliability and validity and were selected carefully following review of their previous use. The Chinese versions of the BPRS, GAS and NOSIE measure psychotic symptoms, overall and psychosocial function of patients; they are reliable and valid, and have been widely used in China. The Chinese version of the KASI had rarely been used in mainland China, but its acceptable reliability and ease of administration and scoring led to its use in this study.
Following ethical approval from the university and hospital, a pilot study was conducted primarily to validate the intervention for use in the local culture and to assess the learning needs of patients and their families. The perceptions of patients’ families and nurses were assessed in the context of the international literature and related research to give validity to the intervention, the Comprehensive Patient/Family Education Guide (CP/FEG) (Reference LiLi, 2003).
Procedure
The education programme commenced in hospital for both patients and their families, but family members were able to choose whether to receive the intervention in hospital or at home subsequent to the patient's discharge. Both the experimental group and the control group were rated on the first four outcome measures on admission and at discharge, and then assessed again on all five measures 3 months and 9 months after discharge. Most studies have indicated that a programme that covers a 9-month to 12-month period following hospital discharge is acceptable to both patients and their relatives. In view of the evidence of relapse rate changes during the first 9 months after discharge, it was decided to adopt two assessment points, one short-term (3 months after discharge) and one 9 months after discharge (Reference Leff, Kuipers and BerkowitzLeff et al, 1985; Reference Tarrier, Barrowclough and VaughnTarrier et al, 1988).
Intervention
The programme duration was 8 h with the patient and 36 h with the family in hospital, and then 2 h per month for 3 months after discharge for patient and family together. A nurse with experience in family intervention (L.Z.) provided the intervention, with the aid of registered nurse research assistants who had either a diploma or a degree and had worked in psychiatric nursing for at least 10 years. The research assistants were given direct supervision and 12 h training in the intervention, and to ensure consistency were observed and critiqued in a pilot situation before the main study. The control group received usual standard treatment and care, in which there was no organised education programme, but patients and families could seek information from staff, and educational pamphlets and materials were available in a ward library. The intervention given to the experimental group was in addition to the standard treatment and care received by the control group. L.Z. and the research assistants were not masked to the participants’ intervention status when completing the assessments.
In the pilot study a random sample of 15 head nurses were asked their opinions on what should be included in the programme, and 51 family members were interviewed to identify their understanding and learning needs. The responses were subjected to content analysis (Reference LiLi, 2003). On the basis of the pilot study results and a synthesis of the major findings from international research in the area, our education programme was designed primarily to educate families and patients about schizophrenia and its treatment, and to teach skills to help patients and families cope more effectively, particularly with the disruptive consequences of the illness (Reference Birchwood, Spencer, Maj and SartoriusBirchwood & Spencer, 2000). The intervention comprised five phases.
-
(a) Phase I: establish a trust relationship with the patient and family, and assess both patient and family; analyse the data gained and identify the family's individual needs (within 1 week of admission).
-
(b) Phase II: deliver the educational programme to patient and family member in hospital (patient 8 h, family member 36 h).
-
(c) Phase III: administer outcome measurement before discharge (within 1 week of discharge).
-
(d) Phase IV: deliver the educational programme to patient and family member after discharge (patient and family member 2 h per month for 3 months).
-
(e) Phase V: administer outcome measurement at 3 months and 9 months after discharge.
RESULTS
A total of 101 people with schizophrenia and their families were recruited to participate in the study (Fig. 1). When the data of the 12 people who withdrew from the programme were removed, there was no significant difference between the experimental and control groups in age, gender, education level, marriage status, hospitalisation times, length of illness and the family members’ relationship with the person with schizophrenia. The composition of the control and experimental groups was considered equivalent in terms of the above demographic data and therefore the foundation for future comparisons of the identified experimental variables was held to be satisfactory (Table 1).
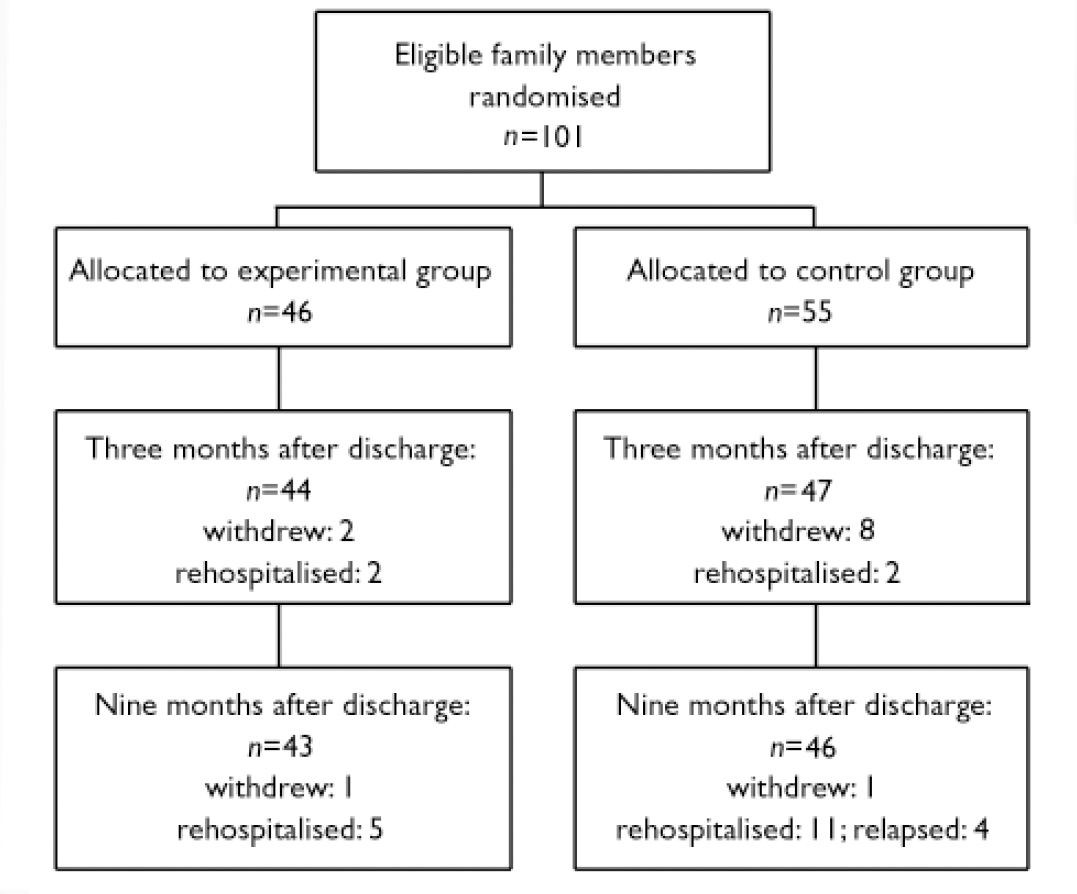
Fig. 1 Flow of participants through the study.
Table 1 Demographic characteristics of the study groups
| Item | Experimental group (n=46) n (%) | Control group (n=55) n (%) | P |
|---|---|---|---|
| Age, years | |||
| ≤20 | 6 (13) | 5 (9) | |
| 21-30 | 11 (24) | 19 (34) | |
| 31-40 | 21 (46) | 22 (40) | |
| 41-50 | 5 (11) | 9 (16) | |
| ≥51 | 3 (6) | 0 (0) | 0.6961 |
| Gender | |||
| Male | 18 (39) | 25 (45) | |
| Female | 28 (61) | 30 (55) | 0.5222 |
| Education | |||
| Junior high | 6 (13) | 17 (31) | |
| Secondary school | 11 (24) | 7 (13) | |
| Senior high | 16 (35) | 17 (31) | |
| College | 13 (28) | 14 (25) | 0.1412 |
| Marital status | |||
| Married or divorced | 23 (50) | 31 (56) | |
| Not married | 23 (50) | 24 (44) | 0.5232 |
| Hospitalisation times | |||
| First time | 26 (57) | 32 (58) | |
| Second time | 12 (26) | 17 (31) | |
| Third or more | 8 (17) | 6 (11) | 0.6142 |
| Duration of illness, years | |||
| ≤1 | 17 (37) | 18 (33) | |
| >1, ≤5 | 11 (24) | 20 (36) | |
| >5, ≤10 | 8 (17) | 8 (14) | |
| >10, ≤20 | 9 (20) | 8 (14) | |
| >20 | 1 (2) | 1 (2) | 0.3201 |
Knowledge about schizophrenia
Data from the KASI were examined at admission and there was no significant difference between the mean scores for the experimental and control groups (Table 2). Analysis of covariance (ANCOVA) was used to compare the differences in the mean scores for total KASI and its six sections for both groups, between admission (baseline) and the three subsequent assessments: at discharge, 3 months and 9 months. There was a significant difference for the experimental group on total score between admission and discharge, between admission and 3 months after discharge, and between admission and 9 months after discharge (Table 2). There was no significant difference for the control group noted between admission and any of the three time points.
Table 2 Outcome measures score by groups
| Outcomes | Experimental group (n=36) | Control group (n=33) | ANCOVA1 | |
|---|---|---|---|---|
| Mean (s.d.) | Mean (s.d.) | F | P | |
| KASI | ||||
| Baseline | 11.9 (2.1) | 12.1 (2.5) | 0.372 | 0.714 |
| Discharge | 14.8 (2.7) | 13.0 (2.1) | 13.18 | 0.001 |
| 3 months | 15.3 (2.9) | 13.0 (2.0) | 18.41 | <0.001 |
| 9 months | 15.9 (3.1) | 13.0 (2.3) | 19.25 | <0.001 |
| ANCOVA3 | F=2.08, P=0.133 | F=0.31, P=0.675 | ||
| Post hoc test4 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | A, P=0.206; B, P=0.304; C, P=0.473 | ||
| BPRS5 | ||||
| Baseline | 46.1 (12.5) | 47.1 (10.3) | 0.452 | 0.743 |
| Discharge | 22.8 (4.3) | 23.0 (5.1) | 0.01 | 0.919 |
| 3 months | 22.8 (3.3) | 23.8 (5.6) | 0.74 | 0.393 |
| 9 months | 22.7 (3.7) | 26.5 (7.4) | 7.60 | 0.008 |
| ANCOVA3 | F=0.53, P=0.589 | F=1.37, P=0.262 | ||
| Post hoc test4 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | ||
| GAS | ||||
| Baseline | 33.3 (9.9) | 28.3 (11.1) | 1.942 | 0.056 |
| Discharge | 74.9 (8.7) | 76.9 (10.8) | 0.07 | 0.792 |
| 3 months | 77.1 (10.2) | 76.4 (13.6) | 0.18 | 0.671 |
| 9 months | 78.0 (10.3) | 70.2 (15.9) | 5.32 | 0.024 |
| ANCOVA3 | F=0.64, P=0.532 | F=3.76, P=0.029 | ||
| Post hoc test4 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | ||
| NOSIE6 | ||||
| Baseline | 168.2 (36.0) | 159.5 (29.6) | 0.962 | 0.34 |
| Discharge | 213.4 (11.1) | 205.7 (12.1) | 4.77 | 0.034 |
| 3 months | 206.8 (12.5) | 202.6 (13.2) | 1.23 | 0.273 |
| 9 months | 206.5 (12.5) | 195.8 (18.7) | 5.77 | 0.020 |
| ANCOVA3 | F=0.41, P=0.663 | F=0.82, P=0.445 | ||
| Post hoc test4 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | A, P <0.00 1; B, P <0.00 1; C, P <0.00 1 | ||
Brief Psychiatric Rating Scale
A t-test revealed no significant difference between the two groups on the total BPRS score at admission, and both groups were therefore considered compatible for the purposes of further inferential analysis. At discharge and at 3 months after discharge ANCOVA revealed no significant difference between the two groups on the total BPRS score. At 9 months after discharge, however, there was a significantly lower score for the experimental group on the BPRS. Interestingly, the mean scores for the somatic concern and motor retardation items were also significantly higher in the experimental group.
Repeated measures ANCOVA adjusted for baseline outcomes was calculated to compare the differences between the groups at the different time points. There were significant differences for both groups on the BPRS score between admission and before discharge, between admission and 3 months after discharge, and between admission and 9 months after discharge. Internal consistency was estimated by Cronbach's a at 0.7.
Global functioning and psychosocial behaviour
There was no significant difference for the GAS scores between the two groups at admission and ANCOVA revealed no significant difference between the two groups before discharge and at 3 months after after discharge, but there was a significantly higher mean in the experimental group at 9 months after discharge (Table 2). We used ANCOVA to compare the mean scores between admission (baseline) and the three assessment points. There were significant differences in the GAS mean scores between admission and before discharge, between admission and 3 months after discharge and between admission and 9 months after discharge for both the experimental and control groups (Table 2). The scores of the experimental group continued to increase from admission to discharge, whereas the highest score for the control group was before discharge.
There was no significant difference for the NOSIE scores between the two groups at admission, and ANCOVA revealed no significant difference between the two groups at 3 months after discharge, but there was a significantly higher mean in the experimental group at discharge and at 9 months after discharge (Table 2). Scores for both groups were significantly different between admission (baseline) and the three time points. Internal consistency of the NOSIE was estimated by Cronbach's a at 0.65.
Relapse and medication adherence
Of the 89 people who completed the study, 4 were readmitted to hospital within 3 months of their discharge, a further 16 were readmitted within 9 months and 4 relapsed according to the BPRS criteria within 9 months of their discharge. There was no significant difference between the experimental and control group in the number of people who relapsed (16% v. 37%), using Fisher's exact test. At 3 months after discharge, 91 participants (excluding the 10 people who had withdrawn at that time) were asked whether they were adhering to their medication regimen. Fisher's exact test revealed no significant difference in medication adherence between the experimental group (30 adherent and 14 not adherent) and the control group (27 adherent and 20 not adherent).
To compare relapse and adherence after discharge, 89 patients (excluding the 12 who had withdrawn) were separated into ‘medication adherent’ and ‘not adherent’ groups. Fisher's exact test revealed a significant correlation between medication adherence and relapse. Clearly, the patients who did not adhere to medication regimens were more likely to relapse (Table 3). No significant difference was found between male and female patient groups and relapse rate. The relapse rate for females was 31% (17/55) and for males 21% (7/34). Because the sample size is small, these are exploratory findings only and need to be treated with caution.
Table 3 Relationship between relapse and medication adherence
| No relapse | Relapse | P 1 | |
|---|---|---|---|
| Medication adherent | 55 | 2 | |
| Not adherent | 14 | 18 | <0.001 |
DISCUSSION
Families’ knowledge about schizophrenia
The significant difference between the experimental group and the control group in the knowledge level assessed by KASI in this study was evident before discharge and existed 3 months and 9 months after discharge. These results suggest that the shorter the duration of illness the less the families know but the more receptive they are to acquiring information, whereas longer duration of the patient's illness gives relatives more time to formulate their own lay model of the illness, making them less likely to be influenced by professional opinion. These results are similar to those of European studies (Reference Barrowclough, Tarrier and LewisBarrowclough et al, 1999; Reference Pharoah, Mari and StreinerPharoah et al, 2003).
Symptoms of patients
Our study confirmed that patient and family education in addition to routine hospital treatment was as effective as the routine hospital treatment alone for schizophrenia in the early admission period. Clearly, over the period from admission to discharge, the medication regimens and other treatments such as occupational and recreational treatment in the hospital have a good effect on the symptoms. This period is one of marked improvement as patients are medicated, relieved of stress and pressure and given ‘intensive’ treatment. Three months after discharge, BPRS scores (including hostile–suspicious symptoms) in the experimental group were significantly lower than in the control group. This interesting and reassuring finding continued at 9 months after discharge, when thinking disturbance, hostile–suspicious symptoms and the overall symptoms in the experimental group were significantly lower than in the control group. This was consistent with the findings of two other Chinese studies (Reference Xiong, Phillips and HuXiong et al, 1994; Reference Zhang, Wang and LiZhang et al, 1994) using the BPRS.
An interesting and unexpected finding was that the somatic concern of the experimental group was higher than that of the control group before discharge and at 3 and 9 months after discharge. Similar findings were not reported in other studies. The tendency of somatic presentation among Chinese patients, and the nurses’ and families’ tendency to reinforce these symptoms in people with mental disorders, has been frequently examined and discussed (Reference Lin, Tseng and YehLin et al, 1995). These behaviours might reinforce the patients’ role and encourage somatic expression of symptoms, or patients might believe that the more intervention they received, the more severe or complex their symptoms were.
Psychosocial functioning of patients
The overall psychosocial functioning of patients in both groups was significantly improved before discharge and at 3 months and 9 months after discharge, compared with their function at admission. However, importantly – and in line with symptom improvement – the overall functioning of the experimental group kept improving, and at 9 months after discharge there was a significant difference between the two groups on the GAS score. These findings support those of Rund et al (Reference Rund, Moe and Sollien1994) and Barrowclough et al (Reference Barrowclough, Tarrier and Lewis1999), but not those of Merinder et al (Reference Merinder, Viuff and Laugesen1999) in their community study, and reinforced the findings of the Chinese studies (Reference Xiong, Phillips and HuXiong et al, 1994; Zhang et al, Reference Zhang, Wang and Li1994, Reference Zhang, He and Gittleman1998; Reference Song, Lu and LiuSong et al, 1998), particularly in terms of return to work.
The outcomes of symptoms and psychosocial functioning in this study demonstrated that the effect of the patient and family education programme may be overshadowed by other factors around discharge, and that it may start to exert its influence only 3–9 months after discharge. One explanation is that it takes time for patients and families to integrate new knowledge and skills into their daily life, and as symptoms and problems with living reappear people are able to change their coping behaviour or modify their relationships and interactions to influence their coping.
This study has reinforced the findings of local Chinese studies of the positive effect of family education on global assessment of functioning. In this study those in the experimental group were healthier at the 9-month measurement point, as it seems that the effects of our education programme become apparent at a point after hospitalisation when symptoms begin to reappear. This confirms similar findings in overseas studies (Reference Barrowclough, Tarrier and LewisBarrowclough et al, 1999).
Medication adherence
The lack of significant difference between the intervention and control groups may be due to the long period of hospitalisation, family factors and/or cultural factors. This finding did help to isolate the notion that medication adherence did not necessarily affect deterioration in symptoms. Caution needs to be exercised with these results, as the sample size was small, the reliability of assessing adherence by patients’ selfreport is questionable and other extraneous variables may be operating. More research needs to be done to identify whether (and why) Chinese people seem to be more adherent than those in overseas studies.
Relapse rate
Nine months after discharge the relapse rate of the experimental group (16%) was lower than that of the control group (37%), but this was not statistically significant. Zhang et al (Reference Zhang, He and Gittleman1998) also reported that compared with the control group (from 26% reduced to 23%), the experimental group (from 32% reduced to 18%) showed a reduction in annual relapse rates at 2-year follow-up. These findings were supported by Song et al (Reference Song, Lu and Liu1998), Xiong et al (Reference Xiong, Phillips and Hu1994) and Chen et al (Reference Chen, Gong and Weng2000).
This study is important because the Chinese government is beginning to increase the numbers of nurses in China and to expand their role, and the societal and legal expectations are that the family members will care for disabled individuals indefinitely, regardless of the emotional and economic burden. Moreover, given the limited housing availability and the complete absence of ‘half-way houses’, neither patients nor families have the option of choosing to live separately. Chinese families and patients need help to adapt to this difficult situation (Reference Zhang, Wang and LiZhang et al, 1994), as the financial consequences of the government accepting responsibility for housing mentally ill persons would be daunting. People with schizophrenia and their families in China therefore should have the chance to obtain an educational intervention in hospital and also after discharge. The success of our education programme, and the needs of the patients and families revealed during the education process, should stimulate nursing managers and nursing staff to realise their own responsibility and be confident to take on the educator role. The Chinese government recognises the need for more nurses of a higher quality, and future studies and practice could be enhanced by the findings of this study. Some of the challenges facing nurses include having to develop interventions that are culturally sensitive and appropriate for environments where patients and their families are hesitant about sharing their feelings and experiences.
This study was the first of its kind to be conducted by nurses in mainland China. Its positive findings provide much impetus for the development of research and independent evidence-based practice in a branch of nursing and healthcare that is in much need of stimulation. Through the rigour of the research process, decades of valuable research was synthesised into a culturally valid intervention, adapted to a unique healthcare environment and successfully applied to a culturally unique sample of patients and their families, by their culturally unique nurses.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The education programme had a significant effect on families’ knowledge and on patient symptoms and overall functioning, particularly at 9 months after discharge.
-
▪ The pressure on families to care for their ill relatives is high in China, and these results offer encouraging clinical tools for development in rural communities as well as institutions.
-
▪ As nursing expands in quantity and with expanded roles, this intervention offers a culturally valid treatment and offers challenges for future implementation across the country.
LIMITATIONS
-
▪ The intervention was offered mainly in the institution owing to the lack of community services, and this might have biased the results.
-
▪ Patients were randomised by ward to avoid contamination of the study groups, and true individual randomisation was not possible.
-
▪ Small sample size and weak measures limit the conclusions in terms of medication adherence and relapse, and further studies are recommended.
Acknowledgements
This study was conducted while Dr Li was a PhD student at the Hong Kong Polytechnic University, funded by the University Grants Committee of Hong Kong.







eLetters
No eLetters have been published for this article.