The numerous short-term and long-term beneficial effects of breast-feeding (BF) are well recognized, and include nutritional, developmental, immunological, psychological and cognitive benefits for breast-fed infants( 1 – Reference James and Lessen 4 ) as well as health and psychological benefits for breast-feeding mothers( 1 , Reference James and Lessen 4 , 5 ). The WHO recommends exclusive breast-feeding (EBF) for the first 6 months and continuation for 2 years or beyond. Even though the 2025 World Health Assembly’s Global Target for Nutrition( 6 ) is to achieve an increase in the rate of exclusively breast-fed infants aged 0–6 months to at least 50 %, only 38 % of infants worldwide breast-feed exclusively( Reference Black, Victora and Walker 7 ).
While a rise of BF initiation rates has been recorded in recent years, there is still widespread concern that BF is not exclusive and is discontinued prematurely( Reference Bosi, Eriksen and Sobko 8 ). In a nationwide telephone survey in Canada of more than 8000 mothers( Reference Chalmers, Levitt and Heaman 9 ), the prevalence of BF initiation was 90·3 %; however, only 14·4 % breast-fed exclusively up to the sixth month. A series of articles published recently in the Lancet provides overwhelming evidence that the prevalence of BF and EBF remains at unsatisfactory levels and falls short of the recommendations in both high- and low-income countries( Reference Victora, Bahl and Barros 10 ).
Across Europe, there is wide variability in the prevalence of BF initiation as well as BF exclusivity and duration( Reference Bosi, Eriksen and Sobko 8 , 11 ). For several countries, information is limited to the first 48 h. According to EuroPerinatal Survey (2010), Cyprus ranks among the lowest in terms of the initiation of BF and EBF at 48 h. The reported estimates, which originate from a Perinatal Survey by the Cyprus Statistical Services( 12 ), suggest that only 16 % of infants were exclusively breast-fed in the first 48 h, while as many as 33·8 % of mothers did not breast-feed at all. Other than being outdated by nearly a decade, the survey captured only the first 48 h. Reported statistics from maternity wards in public hospitals by the Cyprus Ministry of Health covering period the 2007–2012 suggest a somewhat better picture( 13 ). Nevertheless, the prevalence of EBF was still estimated at 27·7 %( 13 ). The latest 2014 Perinatal Survey of the Ministry of Health, which also included the private sector, suggests little improvement in over a decade( 14 ). In Cyprus, as many as 74·5 % of births take place in the private sector where the rate of caesarean section (C/S), a strong determinant of BF initiation( Reference Zanardo, Svegliado and Cavallin 15 – Reference Rowe‐Murray and Fisher 17 ), approaches 60 % according to official data( 14 ). Official statistics in Cyprus go back only a decade (2008–2015), and suggest that C/S rates have been high in this period and still rising (from 53·4 % in 2008 to 56·9 % in 2015)( 18 ). Of those, 16·4 % were classified as emergency C/S, whereas elective C/S reached up to 40·5 %( 18 ). It is worth noting that, based on the same report, C/S rates in the private sector have been constantly high in this period while rates have also risen in the public sector. No home deliveries are currently conducted in Cyprus.
The purpose of the present study was to: (i) provide current estimates of the prevalence of BF and EBF in Cyprus beyond 48 h and up to the sixth month of an infant’s life; and (ii) describe the sociodemographic determinants of exclusivity and duration of BF. The study is part of a wider programme entitled ‘The BrEaST start in life: addressing social inequalities and supporting breastfeeding through inclusion activities’, which aimed to strengthen the evidence base as well as raise awareness among health professionals and the general public alike.
Methods
Study design
The present study is a nationwide cross-sectional and longitudinal descriptive study, conducted in two phases between April 2014 and June 2015. During phase I, a consecutive sample of mother–infant dyads was recruited during their stay at maternity clinics over a period of 6–8 weeks. Keeping the recruitment period constant across sites was important to approximate the correct distribution of births across settings, as there is no official clinic-level data on the number of births in the private sector, which nevertheless accounts for over 70 % of all births. Adjustments to the length of the stay were made if necessary, given the observed non-participation rate, in order for the final sample to approximate the expected proportion of birth across sectors (70–30 split) and across the five districts on the Republic of Cyprus. During phase II, all mothers who provided contact details (telephone and/or email) were followed up prospectively with a telephone interview at the first, fourth and six months postpartum.
All maternity clinics in Cyprus were formally invited in writing to participate, followed by personal meetings with the hospital administration. Maternity wards in all public hospitals (five in total) and twenty-nine of thirty-five private clinics agreed to participate. Of the six that did not participate, four are small maternity clinics in terms of the total number of births. Among the larger clinics (i.e. more than forty births during the recruitment period), two did not participate. In both cases, inconvenience and/or disruption of routine activities were cited as the reasons for opting out.
Eligibility criteria and sample size
Mothers who gave birth in any of the participating clinics during the recruitment period were eligible to participate if they were: at least 18 years of age; could read or speak Greek or English (so as not to exclude the high proportion of non-Greek-speaking service users); had no health problems precluding them from BF, as recorded in the medical file and communicated to the team by the maternity clinic staff (e.g. bilateral mastectomy, postpartum maternal complications); and were not separated for any reason from their infants after birth (e.g. infant was transferred to a neonatal intensive care unit).
Precision analysis with finite population correction (as the annual number of births is about 10 000) suggested that the minimum required sample size to estimate the prevalence of BF with 95 % CI not wider than ±5 % was 370 participants. This sample size also provided sufficient statistical power of 80 % to detect a 10–15 % difference in magnitude at the 5 % statistical significance level for the comparisons of interest (e.g. private v. public sector, vaginal v. C/S birth). This was considered satisfactory and within the expected range based on previous local estimates and published literature. To take into consideration the potential loss to follow-up during phase II, the minimum required sample for phase I was set to at least 550.
Recruitment procedure
Mother–infant dyads were recruited during their stay at the maternity departments. In consultation with the department staff, trained researchers approached mothers at 24 h and no later than 48 h after birth to invite them to participate. Visits were held every other day, since commonly the duration of stay at the maternity clinic in Cyprus is rarely less than 2 d. Eligible mothers were informed by the fieldworkers about the aims of the study and if they agreed to participate, they were asked to complete a questionnaire while fieldworkers waited outside their room to ensure privacy. The questionnaire was then returned in a sealed envelope. The mothers were also given the option to complete the questionnaire in their own time, in which case the fieldworkers arranged a later time to pick it up.
Definition of breast-feeding and exclusive breast-feeding
BF and EBF were based on the WHO definitions( 19 ). Breast-feeding was considered exclusive if an infant did not receive anything other than breast milk, except for medications, vitamin or mineral drops, oral rehydration solution, etc. An infant was considered to be breast-feeding if he/she received breast milk in addition to any other liquid or food, including formula. Specifically, estimates for the prevalence of BF and EBF at each time point of interest were based on the following questions:
-
1. A question on breast-feeding status during the first 48 h, ‘Have you breast-fed your newborn baby in the first 48 h?’, was used to estimate BF initiation.
-
2. Regarding exclusivity, the set of questions referring to Step 7 (‘Implementation of Exclusive Breastfeeding’), as phrased in Section 4 of the Baby-Friendly Hospital Initiative questionnaire for mothers’ self-assessment of maternity unit practices( 20 ), was used. This included a negative response to the question ‘Did your baby receive any supplement?’, together with a negative response to ‘Did your baby receive any of the following?’ referring to formula, water or sugar water, other fluids.
Missing information was considered a negative response regarding BF and EBF, respectively.
At the first month of follow-up, the estimation of BF and EBF followed the same rationale and was based on the mother’s response to the following questions, as used previously( Reference Gaki, Papamichail and Sarafidou 21 , Reference Scott 22 ):
-
1. ‘Does your baby receive: (i) only breast milk; (ii) mainly breast milk, but also formula; (iii) mainly formula, but also breast milk; or (iv) only formula?’
-
2. ‘Until today, has your baby received: (i) water or sugar water; (ii) chamomile tea or other tea; or (iii) fruit or vegetable juice or any other liquid?’
Thus, in addition to the response of ‘only breast milk’, EBF status was defined as a negative response to having received any liquid up the point of conducting the interview.
At the fourth and sixth month of follow-up, any mother who responded positively to the question ‘Do you still breast-feed?’ was considered to still to be breast-feeding. A response of ‘only breast milk’ to the same question as above was considered EBF, together with a negative response to the question ‘Until today, has your baby received: (i) water or sugar water; (ii) chamomile tea or other tea; or (iii) fruit or vegetable juice or any other liquid?’, as well as a negative response to the question ‘Until today, has your baby received: (i) fruit purée; (ii) any ready-made baby cereal or food; or (iii) mashed or solid food?’
In addition, a 24 h recall of feeding practices was reported by mothers at every follow-up based on the Centers for Disease Control and Prevention IFP questionnaire used in the Infant Feeding Practices Study II (IFPS II)( 23 ) modified accordingly based on the literature( Reference Gaki, Papamichail and Sarafidou 21 ) as well as recommendations of an expert panel of paediatricians and lactation consultants from the Cyprus Breastfeeding Association in order to take into consideration predominant local practices (e.g. aniseed tea). Similarly, the IFP questionnaire was further modified accordingly for the fourth- and sixth-month follow-up to include other liquids and solids that might be introduced at any time up to the sixth month.
Generally, effort was made so that the follow-up interviews were conducted within a week of the fourth and sixth month of the infant’s life. Nevertheless, in some cases there was a longer delay in interviewing participants. To correct for the fact that BF or EBF cessation can occur in these critical time points, the self-reported month of BF cessation and of liquid/solid introduction was also taken into account to determine EBF or BF status at the fourth and sixth month.
Research tools
The baseline questionnaire also included a number of other research tools. For the assessment of mothers’ reported experience of the ‘Ten Steps for Successful Breastfeeding’, the self-administered WHO/UNICEF questionnaire – Section 4 (part of the WHO/UNICEF Baby-Friendly Hospital Initiative questionnaire) was used( 20 ), with permission from the Greek National Commission of UNICEF. The assessment of perceived breast-feeding self-efficacy was based on the Breastfeeding Maternal Self-Efficacy scale–short form (BSES-SF)( Reference Dennis and Faux 24 , Reference Hadjiona, Middleton and Kouta 25 ), with permission by the developer who provided an existing Greek translation of the scale. Nevertheless, a number of grammatical and syntax changes were deemed necessary, after a forward–backward translation process, to improve its readability. In a pilot study, the internal consistency of the scale (Cronbach’s α=0·95) and its test–retest reliability were deemed satisfactory (intraclass correlation coefficient=0·73). The BSES-SF contains fourteen 5-point Likert-scale items, with positive statements beginning with ‘I can always …’. The response scale provided for each statement ranges from 1=‘not at all confident’ to 5=‘very confident’. At the sixth month, mothers were also asked to rate, on 5-point Likert scales with 1=‘strongly disagree’ and 5=‘strongly agree’, the importance they personally attributed to a list of fifteen reasons for discontinuing BF, including insufficient milk, inadequate weight gain, breast problems, household and childcare responsibilities, fatigue, etc. (adapted from a similar study( Reference Gaki, Papamichail and Sarafidou 21 )), or provide additional reasons if they wished. Finally, participating mothers provided information on sociodemographic factors, parity, BF history and intention to breast-feed.
Ethical considerations
Before the initiation of the study, all necessary approvals were obtained from the Cyprus National Bioethics Committee, the Research Promotion Committee of the Ministry of Health, which also grants permission of access to public hospitals, as well as from the administration of all participating clinics. Furthermore, notification was sent to the Commissioner of Personal Data Protection. Written consent was obtained from mothers for their participation. Separate consent was obtained for each phase, since participation in the second phase required the provision of personal contact details (telephone number and/or email). Mothers were informed that their participation was on a voluntary basis and that they could withdraw their participation at any time point of the study.
Statistical analysis
Summary statistics (frequencies and mean/sd as appropriate) were used for the description of the sociodemographic characteristics of the participants at baseline. Differences in sociodemographic and other characteristics between mothers who did and did not participate at follow-up were assessed using χ 2 tests for categorical variables and independent t tests for continuous variables. The prevalence of BF/EBF was estimated based on the total number of mothers in the sample at each time point according to the operational definitions above. Mothers who reported BF or EBF cessation at the first or fourth month were included in the sample and retained their BF/EBF status irrespective of non-participation at subsequent time points. Estimation of the 95 % CI for prevalence estimates was conducted using EpiInfo based on the normal distribution approximation except for the sixth-month EBF estimate, for which, due to the very low numbers, exact binomial distribution was used instead. Differences in the prevalence of BF and EBF according to sociodemographic and other characteristics of the mothers were explored in χ 2 tests. The P value for trend was also calculated in the case of ordinal variables. The association between BF/EBF and sociodemographic or other characteristics was also explored in binary logistic regression models. OR of BF and EBF were calculated for mode of delivery, parity, educational attainment and family income at each time point of interest. The associations of BF and EBF with the abovementioned variables were explored before and after mutually adjusting for each other, as well as upon further adjusting for mother’s age, employment and marital status. The statistical software package IBM SPSS Statistics for Windows version 21 was used for the analyses.
Results
Participant characteristics
A total of 1006 mothers were approached during the period of study, of whom 797 fulfilled the inclusion criteria. The baseline sample consisted of 586 mother–infant dyads (response rate 73·5 %). Of those, 372 (response rate 63·5 %), 383 and 340 mothers were contacted by telephone at the first, fourth and sixth month, respectively. Table 1 presents the sociodemographic characteristics of the participants. The majority were aged 25–29 years, were married or cohabiting (92·7 %) and most were Cypriot (71·5 %). In terms of education, 40·6 % of mothers had at most secondary education, while 31·2 and 21·2 % had undergraduate and postgraduate tertiary education. With regard to employment, 60·6 % reported a full-time status, whereas 22·9 % were not employed. Only 12·1 % reported a net family income above 3000€/month. More than half (54·6 %) delivered their infants with C/S (30·9 and 69·1 % in the public and private sector, respectively; P=0·001). The observed rate of C/S is consistent with officially published data. For 47·4 % of mothers, this was their first child. Among the rest, 82·9 % reported previous BF experience. Even though the prevalence of EBF was only 18·8 % at 48 h, 73·2 % of mothers reported their intention to breast-feed exclusively.
Table 1 Sociodemographic characteristics, breast-feeding (BF) initiation, intention for exclusive breast-feeding (EBF) and perceived maternal self-efficacy, at baseline and among responders and non-responders at the first month, among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015
* The χ 2 test was used for categorical variables.
† Only multiparous participants were included in the analysis.
‡ The independent t test was used for continuous variables.
Table 1 also presents the sociodemographic composition of the first-month follow-up sample and a comparison between those who did and did not participate in the telephone follow-up. There were no significant differences between responders and non-responders in terms of age, marital status, education, employment, parity, BF initiation or mode of birth. Non-Cypriot mothers and mothers in lower income categories appeared more likely to participate in the follow-up. Even though no differences were observed in terms of either initiation of BF or intention for EBF, there was a statistically significant difference between responders and non-responders in terms of reported intention to breast-feed exclusively for 6 months (71·0 v. 64·0 %, respectively; P=0·026), most likely suggesting that mothers who participated in the follow-up phase might have more positive attitudes towards BF. No other significant differences were observed regarding sociodemographic characteristics or in terms of perceived BF self-efficacy.
Breast-feeding and exclusive breast-feeding rates up to the sixth month
As shown in Table 2, initiation of BF while at the maternity department was estimated at 84·3 %. Nevertheless, only 18·8 % (95 % CI 15·6 %, 21·9 %) of mothers among the full sample exclusively breast-fed while at the clinic. At the first month postpartum, there was not much change since the prevalence of BF and EBF was 73·9 % (95 % CI 69·4, 78·3 %) and 17·3 % (95 % CI 13·4, 21·1 %), respectively, among mothers who participated in the follow-up. This might be an overestimate of the true prevalence, given that mothers with a more positive attitude towards BF might have been more likely to participate at the follow-up.
Table 2 Prevalence of breast-feeding (BF) and exclusive breast-feeding (EBF) at 48 h after birth and up to the sixth month, according to estimation method, among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015
* Sample size based on number of participants at that time point.
† Sample size at the fourth and sixth months is based on the information given on EBF/BF status at that time point, as well as the assumption that mothers who reported discontinuing EBF/BF at the first or fourth month and lost to follow-up would not initiate BF or EBF again. The observed differences in the denominators for EBF and BF at the fourth and sixth months arise due to the fact that information given by mothers on the introduction of liquids and/or solids is used to indicate their EBF status. Once mothers were lost to follow-up, detailed information on their BF status was not available. Thus, while it might not be known whether some continue to breast-feed, it could be safely assumed that they are not exclusively breast-feeding at that point in time based on information about their EBF status at the previous contact.
‡ For the purposes of comparison between the two methods of estimation, the last two rows present BF and EBF estimates for the fourth and sixth months based on 24 h recall.
By the sixth month, the prevalence of BF was estimated at 32·4 % (95 % CI 27·7, 37·2 %), with the sharpest decline observed between the first and fourth months. With respect to EBF, a more gradual reduction was observed up to the sixth month when only 5·0 % (95 % CI 3·1, 7·6 %) of mothers were breast-feeding exclusively (Table 2; also see Fig. 1). The prevalence of BF based on the 24 h recall of feeding practices was similar, if not slightly lower, than the respective estimates based on self-reported status. For example, the prevalence of BF at the fourth month was estimated at 44·0 % based on reported BF status and at 39·6 % based on whether mothers breast-fed their baby in the 24 h period prior to the interview. With respect to EBF, a slightly larger difference was observed depending on the method of assessment. For example, at the fourth month, the proportion of the mothers who exclusively breast-fed was estimated at 12·3 % based on self-reported status and slightly higher at 19·8 % based on the prior 24 h. In contrast, at the sixth month, only 0·3 % exclusively breast-fed in the 24 h prior to the interview v. 5·0 % based on reported status.
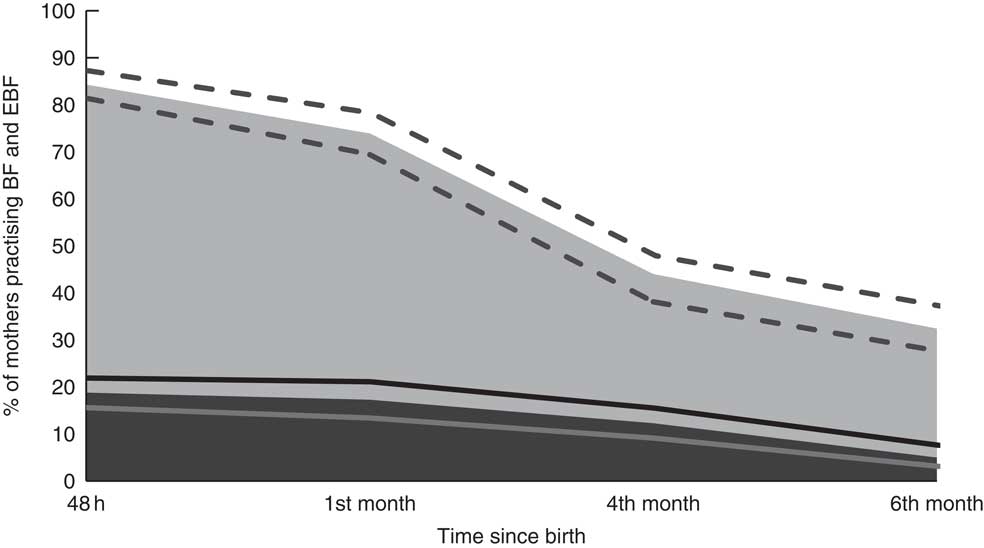
Fig. 1 Prevalence of breast-feeding (BF; ![]() ) and exclusive breast-feeding (EBF;
) and exclusive breast-feeding (EBF; ![]() ) at 48 h after birth and up to the sixth month among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015. The dotted and solid lines represent the 95 % CI for the BF and EBF prevalence estimates, respectively
) at 48 h after birth and up to the sixth month among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015. The dotted and solid lines represent the 95 % CI for the BF and EBF prevalence estimates, respectively
In terms of self-reported reasons for discontinuation, the highest ranking items in terms of importance were: (i) insufficiency of breast milk, by far (since as many as 62·5 % reported that they agree/strongly agree with this statement); followed by (ii) concern with regard to the quantity of breast milk the baby consumes (reported by 32·7 %); (iii) return to work (reported as important by 23·9 %); and (iv) fatigue, depression and stress (reported by 16·6 %). Of the mothers, 8·8 % rated inadequate weight gain as an important reason for discontinuing. In contrast, only 3·5 % of mothers reported that smoking was an important reason for discontinuation and only 6·3 % reported discontinuing due to personal reasons or choice or due to a previous unpleasant experience.
Breast-feeding and exclusive breast-feeding by sociodemographic characteristics
Table 3 presents the prevalence of BF and EBF according to sociodemographic and other characteristics of the participants. There was no significant difference in the prevalence of BF initiation or EBF at 48 h by age, marital status or nationality. In fact, no difference was generally observed according to these variables during the whole period of follow-up. In contrast, there was evidence of a social gradient in favour of mothers of higher socio-economic position. Mothers with higher educational attainment or with higher family income were more likely to BF at 48 h, even though they were not necessarily more likely to breast-feed exclusively. Moreover, they were more likely to still breast-feed at the first and fourth months. For instance, the prevalence of BF at the fourth month displayed a stepwise increase across increasing categories of income (i.e. 39·0, 46·2 and 71·4 %; P for trend <0·001). While not statistically significant, a similar stepwise pattern was observed in terms of EBF whereby twice as many mothers in high-income families were breast-feeding exclusively at the fourth month compared with mothers in the lower income category (19·2 v. 10·9 %; P for trend=0·137). A similar pattern was observed in terms of educational attainment and in fact a statistically significant difference by educational attainment was also observed in terms of EBF at the fourth and sixth months. Estimates for the sixth month are not presented in Table 3 because, apart from education, the observed gap in BF and EBF prevalence rates seemed to narrow by the sixth month.
Table 3 Baseline characteristics, according to breast-feeding (BF) and exclusive breast-feeding (EBF) status at 48 h after birth, the first and fourth month, among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015
C/S, caesarean section.
* Total number of mothers who practise EBF at 48 h, first and fourth months: Ν 110, 64 and 51, respectively; total number of mothers who practise BF at 48 h, first and fourth months: Ν 494, 274 and 169, respectively.
† The χ 2 test was used for categorical variables.
The variables for which the most striking and statistically significant differences were observed are also presented in Fig. 2. In terms of mode of delivery, while no difference was observed in terms of BF initiation, EBF was almost three times higher among mothers who gave birth vaginally (32·0 v. 10·8 and 7·4 % among mothers who gave birth by C/S without and with general anaesthesia, respectively). The difference in EBF by mode of birth was observed across all time points, and was still apparent at the sixth month even though no longer statistically significant. Similarly, while the likelihood to breast-feed did not appear to differ according to whether this was the mother’s first child, EBF was at least twice higher in multiparous compared with primiparous mothers. In fact, the prevalence of EBF at 48 h among primiparas (11·6 %) appeared lower even compared with that among mothers who had other children but reported no previous experience of BF (15·9 %). The difference between primiparous and multiparous mothers remained apparent, and statistically significant, at the first (23·1 v. 10·1 %, P=0·001) and fourth (16·6 v. 7·4 %; P=0·005) months, but not the sixth month.
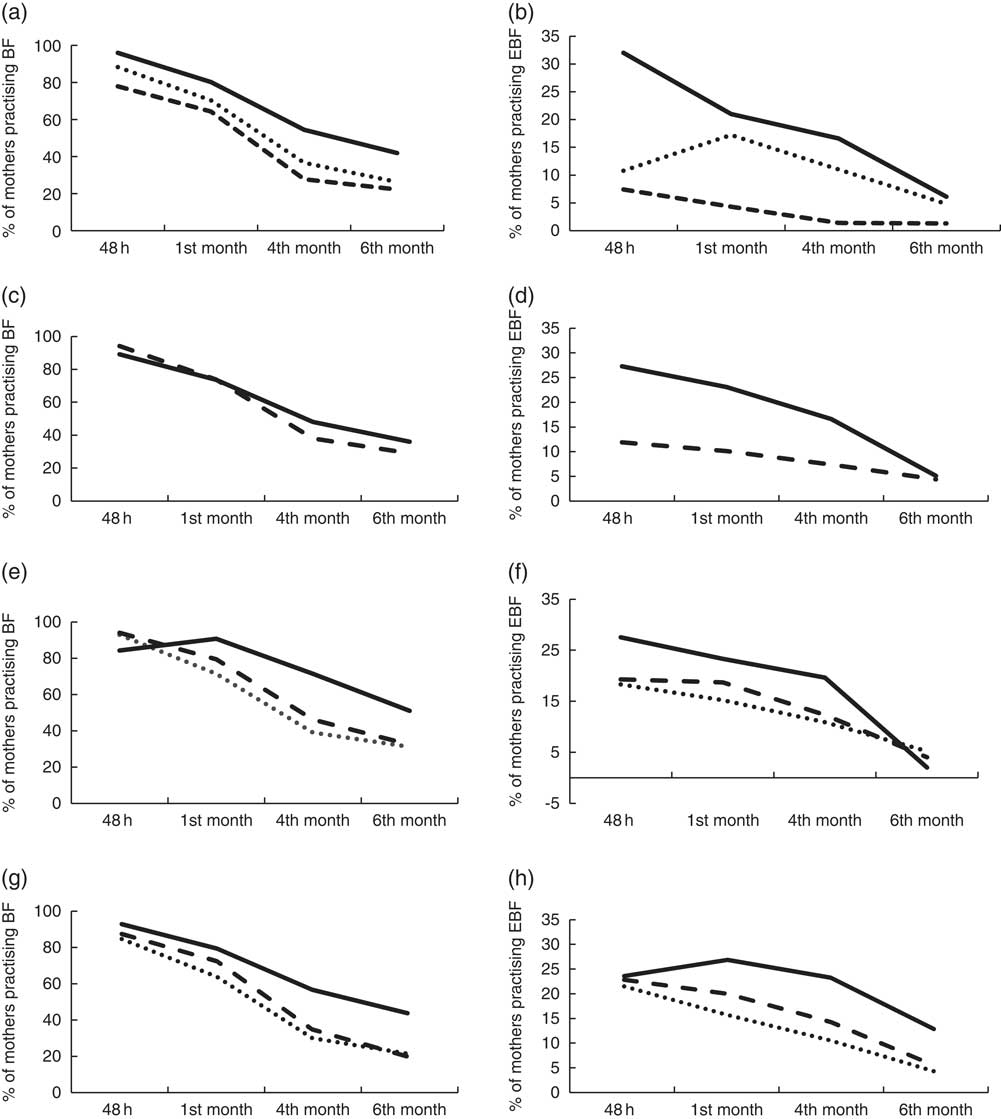
Fig. 2 Graphical representation of the prevalence of breast-feeding (BF; left column) and exclusive breast-feeding (EBF; right column) at 48 h after birth and up to the sixth month, by sociodemographic characteristics, among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015. (a, b) Type of birth (![]() , vaginal;
, vaginal; ![]() , caesarean section without general anaesthesia;
, caesarean section without general anaesthesia; ![]() , caesarean section with general anaesthesia); (c, d) parity (
, caesarean section with general anaesthesia); (c, d) parity (![]() , primiparous;
, primiparous; ![]() , multiparous); (e, f) monthly net family income (
, multiparous); (e, f) monthly net family income (![]() , ≤1500 €;
, ≤1500 €; ![]() , 1501–3000 €;
, 1501–3000 €; ![]() , ≥3001 €); (g, h) educational attainment (
, ≥3001 €); (g, h) educational attainment (![]() , primary/secondary school;
, primary/secondary school; ![]() , college/undergraduate studies;
, college/undergraduate studies; ![]() , postgraduate studies)
, postgraduate studies)
Table 4 presents crude and adjusted OR of BF and EBF by mode of delivery, parity, educational attainment and income. Mode of delivery was the strongest determinant of BF and EBF initiation as well as continuation, at least up to the fourth month. Mothers with a vaginal birth were about three to four times more likely to initiate BF (OR=3·1; 95 % CI 1·7, 5·4; P<0·001) and to breast-feed exclusively (OR=4·3; 95 % CI 2·7, 6·8; P=0·001) After adjustments, this association appeared even stronger for both BF (adjusted OR=4·5; 95 % CI 2·1, 10·0) and EBF (adjusted OR=5·6; 95 % CI 3·3, 9·7), attributed to the fact that mothers of higher socio-economic position (educational attainment and/or income) were more likely to give birth by C/S, yet more likely to breast-feed/exclusively breast-feed. In terms of parity, multiparous women appeared two to three times more likely to breast-feed exclusively throughout the period, and the observed association remained strong even after adjusting for other sociodemographic variables. Even though the estimates attenuated somewhat in the fully adjusted models and were not always statistically significant, evidence of a social gradient in BF and EBF was apparent in terms of both income and educational attainment. Interestingly, the association in terms of education appeared stronger than that of income for both BF and EBF, but seemed largely restricted to mothers with postgraduate education who appeared statistically significantly more likely to breast-feed both at the fourth (adjusted OR=2·1; 95 % CI 1·1, 3·9) month and the sixth month (adjusted OR=2·4; 95 % CI 1·2, 4·6) compared with mothers with secondary education. The association appeared even stronger in terms of EBF. In contrast, it seemed that the association with income appeared stronger in the case of BF (but not EBF), especially after the fourth month.
Table 4 OR (95 % CI) of breast-feeding (BF) and exclusive breast-feeding (EBF) at 48 h after birth and at first, fourth and sixth months, according to each sociodemographic variable before and after mutually adjusting for each other in multivariable logistic models, among a consecutive sample of 586 mothers recruited from maternity wards in all public hospitals and twenty-nine (of thirty-five) private maternity clinics in Cyprus, April 2014–June 2015
AOR, adjusted OR; C/S, caesarean section; Ref., reference category.
The above variables were mutually adjusted but also adjusted for the following variables: age, marital status, employment status.
Discussion
Main findings
The present study estimated the prevalence of BF and EBF for the first time among a representative sample of mothers giving birth in Cypriot private and public maternity departments. While BF initiation appeared high, premature discontinuation was observed with the highest reduction after the first and before the fourth month. By the sixth month, only one in three mothers was still practising BF. The prevalence of EBF was low even at 48 h (18·8 %), while by the sixth month only 5·0 % of the mothers were still breast-feeding exclusively. For primiparas and those who gave birth by C/S, lower rates of initiation, exclusivity and duration of BF were observed. In addition, there was evidence of a social gradient, with mothers of higher socio-economic position being more likely to breast-feed, breast-feed exclusively (particularly those with higher educational attainment) and breast-feed longer.
Prevalence of breast-feeding and exclusive breast-feeding
BF initiation was comparable to estimates seen in some countries such as Greece (87·9 %)( Reference Gaki, Papamichail and Sarafidou 21 ); slightly lower than in some e.g. Canada (90·3 %)( Reference Chalmers, Levitt and Heaman 9 ), Italy (91·6 %)( Reference Lauria, Spinelli and Grandolfo 26 ) and Australia (93·3 %)( Reference Magarey, Kavian and Scott 27 ); but higher than in others e.g. the UK (81 %)( Reference McAndrew, Thompson and Fellows 28 ). The prevalence of BF at the sixth month was lower than respective figures reported elsewhere, such as Italy (57·7 %)( Reference Lauria, Spinelli and Grandolfo 26 ), Norway (82 %)( Reference Kristiansen, Lande and Øverby 29 ), Australia (41·7 %)( Reference Magarey, Kavian and Scott 27 , Reference Scott, Binns and Oddy 30 ), Canada (53·4 %)( Reference Chalmers, Levitt and Heaman 9 , Reference Al-Sahab, Lanes and Feldman 31 ) and the USA (51·8 %)( 32 ), but comparable to the UK (34 %)( Reference McAndrew, Thompson and Fellows 28 ). In contrast, the prevalence of EBF was particularly low even at 48 h, and much lower by comparison to other high-income countries such as Italy (57·2 %)( Reference Lauria, Spinelli and Grandolfo 26 ) and Australia (75·6 %)( Reference Scott, Binns and Oddy 30 ), being more similar to that observed in Greece (41·1 %)( Reference Gaki, Papamichail and Sarafidou 21 ). At 6 months, only one in twenty mothers breast-fed exclusively. This particularly low rate appears comparable to the respective value reported in a recent study from Italy (5·5 %)( Reference Lauria, Spinelli and Grandolfo 26 ). Even though the various studies are not directly comparable, both in terms of methodology as well as the time periods, the low rate of EBF observed in Cyprus at the sixth month appears lower than in Norway (10 %)( Reference Kristiansen, Lande and Øverby 29 ), Canada (13·8 %; 14·4 %)( Reference Chalmers, Levitt and Heaman 9 , Reference Al-Sahab, Lanes and Feldman 31 ) and Spain (10 %)( Reference Lozano de la Torre, Martin-Calama and Hernandez-Aguilar 33 ), but higher than in Australia (<1 %)( Reference Scott, Binns and Oddy 30 ), Greece (0·9 %)( Reference Gaki, Papamichail and Sarafidou 21 ) and the UK (1 %)( Reference McAndrew, Thompson and Fellows 28 ). By comparison to other studies( Reference Chalmers, Levitt and Heaman 9 , Reference Lauria, Spinelli and Grandolfo 26 , Reference Kristiansen, Lande and Øverby 29 , Reference Camutdan, Ilhan and Beyazova 34 ), it is also of note that BF discontinuation appears to occur sooner in Cyprus since BF rates drop sharply between the first and fourth months. In fact, 50 % of the mothers reported BF discontinuation within the first 2 months (data not shown). A similar pattern was observed in a study in Greece, where the greatest reduction was observed even sooner than in the present study( Reference Gaki, Papamichail and Sarafidou 21 ).
Sociodemographic determinants of breast-feeding initiation, exclusivity and duration
Delivery by C/S was the strongest negative determinant of BF and EBF during the first 48 h. This finding is consistent with several previous studies( Reference Zanardo, Svegliado and Cavallin 15 – Reference Rowe‐Murray and Fisher 17 , Reference Al-Sahab, Lanes and Feldman 31 , Reference Pérez-Escamilla, Maulén-Radovan and Dewey 35 – Reference Tavoulari, Benetou and Vlastarakos 37 ). The high rate of C/S deliveries in Cyprus might partly explain the very low rate of EBF. Comparable low EBF rates are reported elsewhere with similar high rates of C/S( Reference Pechlivani, Vassilakou and Sarafidou 38 ). Furthermore, as in the present study, C/S has also been associated with BF duration( Reference Kohlhuber, Rebhan and Schwegler 39 , Reference Ahluwalia, Li and Morrow 40 ). Evidence supports that delay of initiating BF may lead to difficulty in successfully establishing BF and therefore to premature discontinuation( 14 , Reference Prior, Santhakumaran and Gale 16 ). To date, no studies from Cyprus have directly addressed the multitude of reasons behind the currently high C/S rate. One study of qualitative design( Reference Hadjigeorgiou, Kouta and Papastavrou 41 ) may shed further light into the issue. Even though that study focused on women’s choice of place of birth (rather than mode of birth), some of the themes identified provide a deeper understanding into the birth environment as well as some of the perceptions of Cypriot women around childbirth. Medicalization of childbirth, as well as fear and safety of mother and baby, were identified as some of the main factors that influence the choice of place of birth. Furthermore, a qualitative study among midwives on their role as advocates of normal birth identified five main interconnected themes: ‘lack of professional recognition’, ‘deficiencies in basic or continuing education’, ‘physician dominance’, ‘medicalization of childbirth’ and ‘lack of institutional support’( Reference Hadjigeorgiou and Coxon 42 ).
Evidence on the association of BF with parity in the literature is inconsistent. Several studies report that primiparous mothers may be more likely to initiate BF( Reference Scott, Landers and Hughes 36 , Reference Manios, Grammatikaki and Kondaki 43 ). However, they are more likely to discontinue BF( Reference Camutdan, Ilhan and Beyazova 34 ), probably due to lower self-efficacy for BF and lack of support( Reference Dennis and Faux 24 ). It is not uncommon for studies to also show that BF initiation( Reference Tavoulari, Benetou and Vlastarakos 37 ) and premature BF discontinuation( Reference Kohlhuber, Rebhan and Schwegler 39 ) are more common among multiparous mothers, or report no differences by parity( Reference Camutdan, Ilhan and Beyazova 34 , Reference Ekström, Widström and Nissen 44 ). This is probably largely dependent on the community health services and support (formal and informal) available for first-time mothers, which vary considerably across settings. For instance, in the case of Cyprus, it is not surprising given the lack of BF support in the community. With no community midwifery, care is largely provided by paediatricians in the private sector with varied practices, while a number of non-governmental organizations fill the gap in formal services by providing postnatal education and support, but the capacity and reach are limited. In fact, their services may benefit the more health literate who seek the support, introducing further social stratification.
Similar to the social gradient observed in the present study, several studies have repeatedly shown a positive association of educational attainment( Reference Victora, Bahl and Barros 10 , Reference Kristiansen, Lande and Øverby 29 , Reference Al-Sahab, Lanes and Feldman 31 , Reference Flacking, Nyqvist and Ewald 45 – Reference Yngve and Sjöström 48 ) and/or family income( 20 , Reference Amir and Donath 46 , Reference Meedya, Fahy and Kable 47 ) with BF initiation and longer duration. However, beyond indicators of social position, an important aspect that has been receiving more attention in recent years is the health literacy of parents. A recent study from the USA provides evidence to suggest that low parental health literacy is associated with ‘obesogenic’ infant care behaviours, including formula-feeding and immediate feeding when the baby cries( Reference Yin, Sanders and Rothman 49 ) and premature BF discontinuation( Reference DeWalt and Hink 50 ). Furthermore, while research evidence suggests that motivation to change towards a healthier lifestyle is higher during the transition to parenthood( Reference Edvardsson, Ivarsson and Eurenius 51 , Reference Lindqvist, Lindkvist and Eurenius 52 ), there is also evidence suggesting that, while intentions may generally improve, perceived behavioural control or actual change may be differential among fathers v. mothers as well as new parents v. established parents( Reference Bassett-Gunter, Levy-Milne and Naylor 53 ). The extent to which this is also differential according to the socio-economic position or indeed the health literacy of the parents is not well understood. Moreover, owing to the fact that initiation of BF is high (about eight out of ten women initiate BF), low rates of EBF and early discontinuation may not necessarily indicate that parents do not acknowledge the benefits of BF or show lack of motivation( Reference Synnott, Bogue and Edwards 54 ). Taking a socio-ecological framework approach, several factors beyond the intrapersonal level are at play, such as practical difficulties( Reference Odom, Li and Scanlon 55 ), misconceptions with regard to infant feeding( Reference Synnott, Bogue and Edwards 54 ) (such as perception of insufficient breast milk, also observed in the present study) and lack of BF support or supportive policies from the immediate or wider social environment, health professionals and workplace( Reference Atchan, Foureur and Davis 56 , Reference Hannula, Kaunonen and Tarkka 57 ).
One important aspect is BF education in the prenatal period (Step 3 of the ‘Ten Steps for Successful Breastfeeding’). It has been previously reported that implementation of Step 3 across Cypriot maternity clinics is suboptimal( Reference Hadjiona, Middleton and Kouta 25 ). Specifically, only 15·7 % of mothers reported receiving information in the antenatal period on all three topics concerning successful EBF (the importance of skin-to-skin contact, rooming-in and the risk of giving water, formula or other supplements in the first 6 months), while as many as 57·9 % reported receiving no such advice. Regarding adherence to the International Code of Marketing of Breast-milk Substitutes, a high proportion of mothers (83·8 %) reported not receiving any breast-milk substitute up to the point of the interview (24–48 h after birth). Nevertheless, this might be an overestimation resulting from the study design since samples may be given at discharge.
Methodological issues on the estimation of breast-feeding indicators
The present study used both a 24 h recall of infant feeding practices as well as self-reported status to estimate the prevalence of BF and EBF. Even though the WHO recommends the 24 h recall dietary method for comparability and consistency of estimation of the BF indicators, this method has been criticized because it may lead to misclassification of BF status( Reference Hector 58 – Reference Li, Scanlon and Serdula 61 ). In fact, the 24 h recall method appears to overestimate EBF at the fourth month compared with self-reported status. This observation could be attributed to the fact that during the weaning phase, mothers may have already introduced other liquids in the child’s diet but exclusively breast-fed the day prior to the interview. Other studies have also suggested that the 24 h method may overestimate the prevalence of EBF( Reference Agampodi, Fernando and Dhramratne 59 – Reference Li, Scanlon and Serdula 61 ). In Aarts et al.’s study, current status of EBF was estimated to be about 40 % higher at the second and fourth months and 9·2 % higher at the at six month in comparison with retrospective measurement of EBF since birth( Reference Aarts, Kylberg and Hörnell 60 ).
In the present study, the 24 h recall produced a lower estimate for EBF than self-reported status at the sixth month (0·3 %) compared with the fourth month (5·0 %). This is more likely to be a design effect, since the self-reported month of BF cessation and of liquid/solid introduction in infant feeding were also taken into account to determine EBF or BF status at the fourth and sixth months. For example, at this critical period, if a mother was interviewed a few days past the sixth month and reported liquid or solid introduction at the sixth month and no sooner, she was then considered to be breast-feeding exclusively up to the sixth month.
Strengths and limitations
The present study is the first to provide current estimates of BF and EBF past the first 48 h in Cyprus, with participation of nearly all the maternity clinics in the country from the public and private sectors. A clear strength of the study is the prospective design which facilitated the assessment of infant feeding practices over the period of the first 6 months, avoiding the recall bias of a retrospective design. Furthermore, in addition to self-reported BF and EBF status, the study also assessed the time of introduction of liquids or solids. The extent to which the self-exclusion of two larger private clinics has affected the estimates is not clear, but the national representativeness of the sample is supported by the fact that no differences were observed in terms of the anticipated proportion of C/S based on best available national data.
However, the present study has some limitations. First, the baseline response rate was 73·5 %, which none the less is within the range observed in studies elsewhere( Reference Kristiansen, Lande and Øverby 29 ). Reasons for not participating were not clear; thus, the extent to which potential selection bias has over- or underestimated the prevalence is not known. Nevertheless, the observed prevalence rates at 48 h appear very similar to the only available data( 12 – 14 ). This may suggest that there has not been much improvement in nearly a decade. Alternatively, assuming that a less favourable attitude towards BF may have contributed to the decision of mothers to opt out, then this may also suggest that the study may not only have overestimated the true prevalence of BF, but also that there has been a decline in BF and EBF prevalence over this period. Similarly, even though no significant sociodemographic or other differences were observed in terms of participation in the follow-up phase of the study, it is more likely that the study has overestimated the true prevalence, given that mothers with a more positive attitude towards BF as indicated by reported intention to BF were more likely to participate.
Conclusion
Significant improvements have been achieved in many European countries through the development of national policies and actions to promote and support BF over the last decade( Reference Cattaneo, Burmaz and Arendt 62 ). The National Breastfeeding Committee of the Cyprus Ministry of Health has recently developed a national strategy for breast-feeding (2011) and policy (2015), published on the Cyprus Ministry of Health’s website (www.moh.gov.cy; available only in Greek), which includes a call to launch the Baby-Friendly Hospital Initiative. Currently, no hospital in Cyprus is certified as baby-friendly. The particularly high rates of C/S, together with fragmented implementation of the ‘Ten Steps for Successful Breastfeeding’( Reference Hadjiona, Middleton and Kouta 25 ), may contribute to the low prevalence of EBF and its premature discontinuation.
This highlights the need for further research of both quantitative and qualitative design into understanding this multidimensional phenomenon, including the reasons for the high rate of C/S, knowledge about the benefits and practice of BF, as well as general parental health literacy. Furthermore, there is a pressing need for interdisciplinary policy action to protect, promote and support BF with clear BF policies, including structural changes such as the introduction of community care and community intervention programmes, as well as public awareness campaigns to challenge both potential misconceptions (e.g. insufficient milk) and social norms (e.g. breast-feeding in public).
Acknowledgements
Acknowledgements: The authors wish to express their appreciation and gratitude to all mothers who participated in the study and to the fieldworkers for their essential contribution in the recruitment of participants at the maternity clinics and data collection at the baseline phase of the study. Furthermore, they would like to acknowledge the National Breastfeeding Committee for its support. Financial support: The study was part of the research programme ‘The BrEaST start in life: addressing social inequalities and supporting breastfeeding through inclusion activities’, which was funded by Iceland, Liechtenstein and Norway through the EEA Financial Mechanism and the Republic of Cyprus. The funders had no role in the design, analysis or writing of this article. Conflict of interest: The authors declare of no conflict of interest. Authorship: N.M., I.P.-D., O.K., C.K., E.L. and E.H. conceived and designed the study and secured the funding. I.P.-D. was the project leader and N.M. was the scientific coordinator of the BrEaST start in life programme. M.E. was the study’s research coordinator and the study forms part of her doctoral dissertation. N.M. was the main PhD advisor of the first author (M.E.) and C.K. and E.L. were members of the PhD advisory committee, and were all involved in the overall supervision of the study. N.M., V.H., E.P. and M.E. trained the fieldworkers and monitored the data collection at phase I. V.H. and F.T. performed data collection at phase I of the study and contributed to data management and analysis and to the editing of the manuscript. M.E. conducted the telephone follow-up data collection at phase II, managed the data set, performed the statistical analysis and wrote the first draft of the manuscript. N.M. guided the statistical analysis and N.M. and O.K. assisted in drafting and editing the first draft of the manuscript. All authors assisted in interpreting the data and critically revised the manuscript. All authors have read and approved the final version of the manuscript. Ethics of human subject participation: This study was approved by the Cyprus National Bioethics Committee, the Research Promotion Committee of the Ministry of Health, and the administration of all participating clinics. Notification was sent to the Commissioner of Personal Data Protection. Written consent was obtained from mothers for each phase of their participation.









