EDITOR:
Failure to restore an adequate airway in patients with acute upper airway obstruction can rapidly lead to hypoxic injury or even death. Helium–oxygen mixtures (heliox) are less dense than air–oxygen mixtures and can improve the flow of gas through partially obstructed airways. Since Barach described this principle 70 years ago, heliox has at times been applied in spontaneously breathing patients with acute upper airways obstruction [Reference McGee, Wald and Hinchliffe1]. Heliox has also been combined with (non-) invasive mechanical ventilation, often with specifically adapted apparatus [Reference Jaber, Fodil and Carlucci2]. However, the correct function of ventilators relies on the precise measurement of flow, pressure, temperature and oxygen fraction for which the necessary sensors are calibrated for use with air–oxygen. The unique physical properties of heliox have an important impact on all these measurements. Thus the correct application of heliox in ventilators is far from trivial [Reference Tassaux, Jolliet, Thouret, Roeseler, Dorne and Chevrolet3]. This technical problem becomes especially relevant under emergency circumstances.
Continuous positive airway pressure (CPAP) by face mask can reduce upper airway collapse [Reference Visvanathan, Kluger, Webb and Westhorpe4] and the combination of mask CPAP and heliox might be useful. The Boussignac continuous positive airway pressure (BCPAP) system (Vygon, 95440 Ecouen, France) for mask CPAP is a simple and lightweight (10 g) disposable plastic device without moving parts [Reference Maitre, Jaber and Maggiore5]. This device may thus avoid the problems with ventilators and heliox.
In a bench test, we evaluated whether heliox works with the BCPAP system and how much more heliox flow was needed compared to oxygen to achieve similar pressures. We then evaluated the effect of this combination in selected patients with acute upper airways obstruction. We chose a helium–oxygen mixture of 60/40 to ensure a sufficient oxygen delivery under all circumstances.
For the bench test we used 10 randomly selected, commercially available BCPAP systems and an analyser specifically designed to measure pressure or flow for helium–oxygen mixtures (VT Plus, Fluke Biomedical, Carson City, NV, USA). Since the variable orifice flow meters mounted on the heliox cylinders were oxygen-calibrated, we first recalibrated these meters by comparing the indicated flow of oxygen or heliox with the true flow as measured with the VT-plus analyser. This was done 10 times for each of the following levels of indicated flow: 5, 10, 15, 20, 25 and 30 L min−1. The observed relation between indicated and actual flow was also compared to the theoretically predicted flow [Reference Papamoschou6]. After this flow-calibration, we then measured the pressures generated by the BCPAP system for the various indicated flows (Fig. 1). The measured flow rates (true flow) of the variable orifice flow meters showed a 25 ± 6% (SD) higher flow for heliox compared to oxygen. When we calculated the predicted actual flow for the variable orifice flow meters for heliox 60/40 based on the gas laws and assuming fully turbulent conditions with densities (ρ = rho) of 1.33 and 0.17 kg m−3 for oxygen and heliox, respectively [Reference Papamoschou6]: (ρO2/ρHeliox 60/40)0.5 ≈ (1.33/0.63)0.5, the theoretically predicted actual flow was 145% of the indicated flow. Thus the behaviour of the variable orifice flow meter with heliox was not in accordance with the assumptions of the simplified gas law.
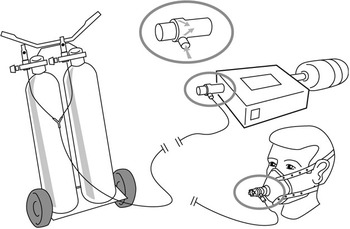
Figure 1 In a bench test (upper right), the static pressures generated by the Boussignac continuous positive airway pressure (BCPAP) system for various flows of heliox 60/40 were measured in a closed system. For this purpose, the patient side of the BCPAP system was connected to a pressure analyser. In patients, the BCPAP system was connected to a face mask.
Flow–pressure measurements were performed at six levels of flow indicated by the orifice flow meters. At every flow level, pressure was measured 10 times. With regard to the generated pressure by the BCPAP system, both for oxygen and for heliox, an approximately linear flow–pressure relation was observed. Compared to oxygen, a true heliox flow of 178% (95% CI: 168–188%) was needed to achieve similar levels of CPAP.
For rapid transport to any patient in our hospital with acute upper airway obstruction, we put the heliox cylinders and the BCPAP system, as well as conventional non-rebreathing masks, on a small trolley (Fig. 1). Over a 2-yr period, seven adult patients (aged 53–83 yr) and one infant aged 3 months with life-threatening obstruction and various degrees of inspiratory stridor were treated. Causes of the stridor included laryngeal cancer, vocal cord palsy, post extubation stridor or hygroma. Heliox and BCPAP were administered for a mean (SD) duration of 83 ± 42 (range 60–180) min. We used indicated flows from 20 to 30 L min−1, corresponding to true flow of 25–36 L min−1 and pressures of 6–8 cm of H2O. In all cases stridor typically decreased or disappeared within a few minutes. In four patients a definitive airway was established after intubation with an endotracheal tube and in four cases with a tracheostomy. In one patient we successfully performed flexible intubation through the BCPAP system.
We showed that heliox could effectively generate pressure in the BCPAP system. The simplicity of this system with no moving parts allowed us to put it on a trolley that could be brought to patients. The application of heliox and BCPAP was effective in creating clinical stabilization allowing time to create a final secure airway. Acute upper airway obstruction is often a life-threatening situation. Under such circumstances, establishing a safe definitive airway is crucial, but the procedure itself is one of the most dangerous actions in medicine. It should be stressed that neither CPAP nor heliox nor CPAP and heliox combined are intended to solve the airway obstruction, but to immediately relieve the work of breathing and buy some time. In the meantime, the precise cause of respiratory failure may be identified and an experienced team can prepare to establish a definitive airway. The considerable cost of heliox [Reference McGee, Wald and Hinchliffe1] is another reason to limit the duration of treatment with heliox. There are several reports of clinical application of heliox and non-invasive ventilation [Reference Jaber, Fodil and Carlucci2]. It is known that non-invasive ventilation and also CPAP decrease the work of breathing in patients with upper airway obstruction [Reference Visvanathan, Kluger, Webb and Westhorpe4]. Heliox also decreased the work of breathing in these patients. Obviously, CPAP alone or heliox without CPAP given by venturi mask or non-rebreathing mask may be the easiest and best solution for many patients. We assumed that combining heliox and BCPAP might have additive effects. Recently, a study showed the effectiveness of the combination nasal CPAP and heliox in infants [Reference Martinon-Torres, Rodriguez-Núñez and Martinon-Sánchez7]. To our knowledge there are no reports in adults of combining heliox specifically with CPAP devices, including the BCPAP system. The unique open design of the BCPAP system makes bronchoscopy [Reference Maitre, Jaber and Maggiore5] or even endotracheal intubation, through the system, possible with no loss of CPAP. As the true heliox flow differs both from the actual and from the theoretically predicted flow, recalibration of flow meters is mandatory, especially since the gas cylinders empty much faster than might otherwise be expected.
The simple BCPAP system circumvents many of the disadvantages associated with the use of heliox with mechanical valves or ventilators. We think the BCPAP heliox combination may be of use as a bridging therapy in selected patients with acute upper airway obstruction. Prospective studies are needed before a final recommendation can be made about the benefit of this therapy.



