Some understanding of infant mental health is essential for all psychiatrists: in adult psychiatry, forensic psychiatry, addictions and learning disability psychiatry, patients’ difficulties can have a profound impact on their relationship with their young children and a significant impact on the child's future development. Problems presenting in early childhood can signal infant mental illness, infant-carer relationship difficulties, or be an early warning for recognised syndromes in middle childhood.Reference Gillberg1 This is becoming more relevant to psychiatric services worldwide, as intervention in the early years may be financially sensibleReference Heckman2 (Fig. 1) and alter the prognosis of affected children.Reference Wallace and Rogers3 Figure 1 represents educational interventions for children, but its message is equally relevant for health: it has been amply demonstrated that focused, evidence-based interventions delivered in the early years can have a profound and long-lasting effect on a range of outcomes including crime, substance use, sexual behaviour and earnings.Reference Olds, Henderson, Cole, Eckenrode, Kitzman and Luckey4,Reference Schweinhart, Montie, Xiang, Barnett, Belfield and Nores5
Problems in the early months and years of life are related to a range of difficulties across the lifespan, including conduct disorder/antisocial personality disorder, suicide and cardiovascular disease.Reference Deans, Bezlyak, Ford, Batty, Burns and Cavanagh6,Reference Dube, Anda, Felitti, Chapman, Williamson and Giles7 For example, children with early-onset persistent aggression have escalating problems – in adolescence, they already have nine times the risk of death from all causes.Reference Coffey, Veit, Wolfe, Cini and Patton8 Societal costs will be ten times those of their peers who do not exhibit aggressive behaviour.Reference Scott, Knapp, Henderson and Maughan9 Effective early interventions and preventive programmes which target a range of difficulties now exist.Reference Bakermans-Kranenburg, van IJzendoorn and Juffer10-Reference Havighurst, Wilson, Harley, Prior and Kehoe13 However, despite increased understanding of the importance of infant mental health, this has not translated into service development. This may, at least in part, be because clinicians lack the confidence and the tools to deliver infant mental health assessments and treatments.
Despite an explosion in research on infant mental health in recent years, it has not been easy to translate research findings into clinical practice: a review by Skovgaard et al Reference Skovgaard, Houmann, Landorph and Christiansen14 highlights the gaps in the literature regarding infant mental health, in particular that research generally uses small samples of high-risk children and families, and relationship assessments used may be expensive and time consuming. We were curious to see what the literature has identified as key issues in infant mental health – of use for clinicians – and what measures were being used clinically to classify disorders in this age range.
What might infant mental health services look like?
There is a paucity of research on infant mental health based in clinical settings. One clinical study noticed that the majority of referrals from a high-risk, socioeconomically deprived population fell within the third year of life, and speculated that clinicians tend not to refer before the age of 1 year.Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15 They noticed a higher rate of classified infant mental health disorders such as post-traumatic stress disorder (PTSD), regulatory disorder and multisystem developmental disorder16 from 25 to 36 months compared with earlier – perhaps related to the fact that symptoms of these disorders may only be unmasked when the infant moves through the developmental changes during this time.Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15 The Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0–3) axis I diagnoses are more frequently made from the age of 3 years, with an increase in diagnoses of neurodevelopmental disorders and a decrease in feeding and sleeping disorders compared with the first year of life:Reference Cordeiro and Da Silva17 this seems sensible given the developmental changes which occur in this time. However, the increase in referrals from the second year of life could hint at a critical developmental/vulnerable period at this time where developmental capacities may deviate from the norm and parents seek advice.Reference Cordeiro and Da Silva17
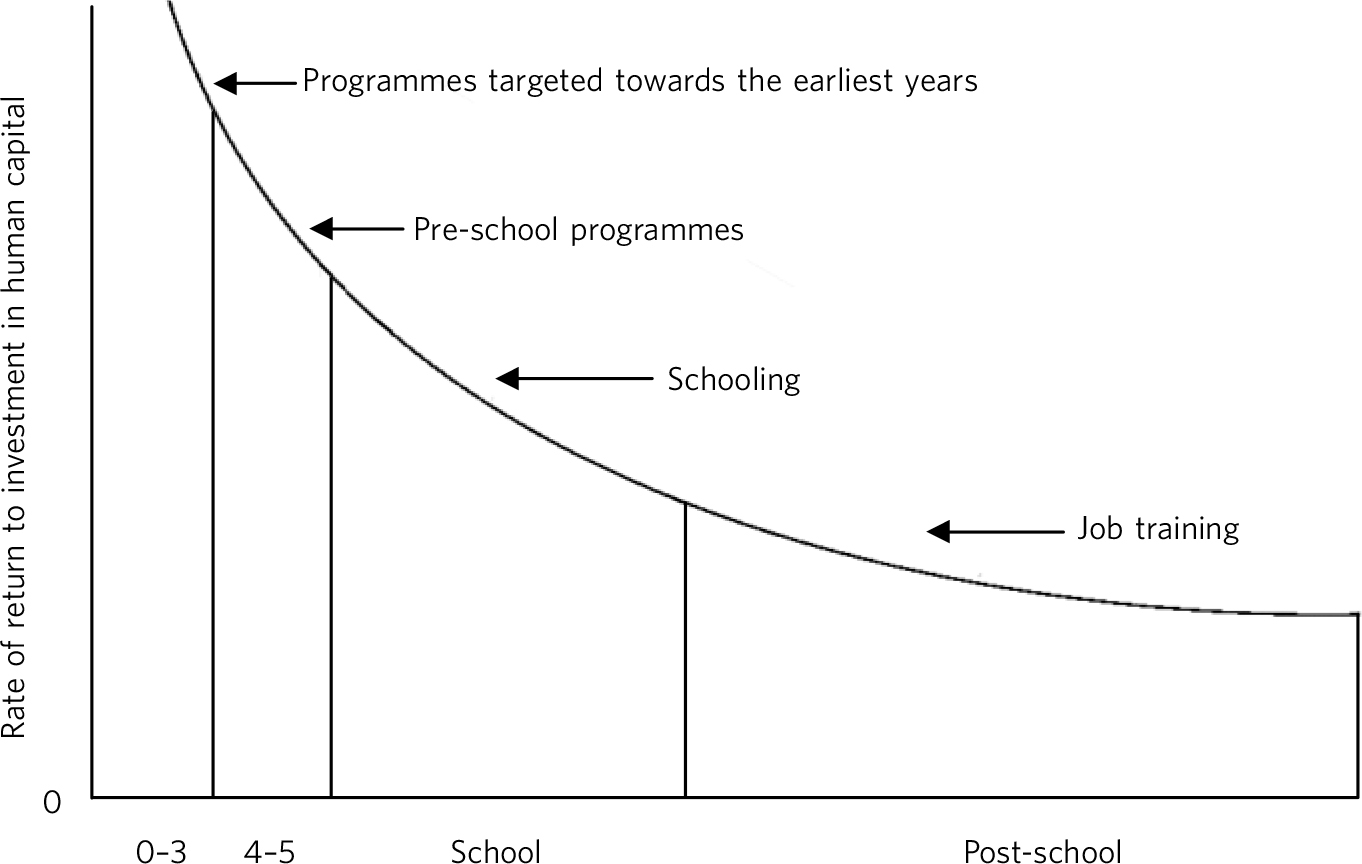
FIG. 1 Returns to a unit dollar invested. Reproduced with permission from Heckmann.Reference Heckman2
The most common symptoms found in referred infants, in clinical studies, were sleep problemsReference Frankel, Boyum and Harmon18 and eating problems.Reference Keren, Feldman and Tyano19 The vast majority of referrals were due to a concern noted about the child, with only a minority of families referred due to a primary relationship problem identified by the referrer.Reference Keren, Feldman and Tyano19,Reference Knapp, Ammen, Arstein-Kerslake, Poulsen and Mastergeorge20
Regarding interventions, a meta-analysis by Bakermans-Kranenburg et al Reference Bakermans-Kranenburg, van IJzendoorn and Juffer10 described that ‘less is more’ when it comes to interventions for improving the parent-infant relationship and attachment security: they found that the most successful interventions did not depend on large numbers of sessions. Their findings demonstrated that the idea of ‘any intervention being good intervention’ is also not necessarily the case: an intervention with a modest number of sessions (<16) and clear behaviour focus for parents seems most useful.
Classifying infant mental health problems
‘Epidemiology has demonstrated that early childhood disorders are as impairing, persistent, and associated with known psychopathology risk factors as disorders at other points in childhood’.Reference Egger and Emde21 Despite the importance of identifying mental health problems in very young children, applying DSM criteria is challenging because of the rapid developmental changes, limited language abilities and interdependence with caregivers.Reference Egger and Emde21,22 Some DSM-IV diagnoses can be applied to, and are relevant for, very young children, and clinicians are encouraged to use DSM-IV diagnoses where appropriate.Reference Egger and Emde21 GillbergReference Gillberg1 has coined an acronym, ESSENCE (Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations), which addresses some of the challenges faced by clinicians when categorically diagnosing disorders in pre-school children. He suggests that certain symptoms can act as markers for a neurodevelopmental disorder later in childhood. He highlights the potential pitfalls of making a definitive diagnosis in the pre-school age group where such overlap among disorders exists, and counsels that separation of disorders may be premature and clinically unhelpful.
In contrast, others have found it useful to classify disorder in very young children; Egger & EmdeReference Egger and Emde21 have provided a detailed review of the development of criteria for classifying mental health disorders in early childhood. The DC:0-3 tool was developed in 1994 to complement existing classification systems and to provide a clear clinical framework for diagnosis up to age 4. In contrast, the Research Diagnostic Criteria – Preschool Age (RDC-PA) offered another diagnostic classification, heavily weighted towards DSM-IV and promoting systematic research into infant mental health by offering clearly specified criteria.23 The DC:0-3 tool was subsequently revised in 2005 (DC:0-3R)16 in an attempt to combine learning from the more ‘top-down’ RDC-PA approach that begins with classifications used in older children and adults and the DC:0-3 approach that uses scientific knowledge specific to infants and young children.Reference Egger and Emde21 Although similar to the RDC-PA via common DSM-IV traits, DC:0-3R is more clinically oriented and has been used widely in clinical practice with children up to the age of 5 years.Reference Frankel, Boyum and Harmon18
The DC:0-3R tool is a multi-axial categorical classification system with five axes: axis I, primary diagnosis; axis II, relationship disorder classification; axis III, medical and developmental disorders and conditions; axis IV, psychosocial stressors; and axis V, emotional and social functioning.16 Axes I, III and IV are similar to those in the DSM-IV. Axis II is a new way of including the parent-infant relationship, which may be disordered. Emde & WiseReference Emde and Wise24 also suggested a sixth axis to include consideration of family history of mental disorder, availability of family resources and cultural factors.
The DC:0-3 manual includes advice on the use of its system, and explains various assessment tools used to help the clinician classify a disorder. Wright & NorthcuttReference Wright and Northcutt25 also developed some ‘decision trees’ to help guide the clinician with questions to ask in clinical assessments, observation of the parent-infant interactions, and assessment of the functional emotional developmental level, with reference to DC:0-3.
When looking at the relationship between DC:0-3 and DSM classifications, similarities exist between axis I disorders such as PTSD, adjustment disorder,Reference Dunitz, Scheer, Kvas and Macari26 affective disorders, disorders of sleep and eatingReference Emde and Wise24 and reactive attachment disorder (RAD)Reference Frankel, Boyum and Harmon18,Reference Dunitz, Scheer, Kvas and Macari26 (reactive attachment disorder has been revised to deprivation/maltreatment disorder in DC:0-3R, due to confusion between attachment problems which could be included in axis II16).
What are regulatory disorders?
Regulatory disorders have not been previously described in any other classification system. Several subtypes exist in DC:0-3. These disorders refer to the difficulties a child may have in regulating emotions and behaviours in response to sensory stimulation, leading to impaired development and functioning,16 thought to share some common ground with the concept of temperament, where disorder occurs at the extremes.Reference Skovgaard, Houmann, Landorph and Christiansen14 The subtypes include hypersensitive, fearful/cautious, negative/defiant, hyposensitive/underresponsive and sensory stimulation-seeking/impulsive.16 Early use of DC:0-3 showed that paediatricians found these terms useful to describe very young (<1 year old) children who do not suit DSM criteria.Reference Dunitz, Scheer, Kvas and Macari26 There has been overlap identified with DC:0-3 regulatory disorder and DSM diagnoses of oppositional defiant disorder (ODD) and attention-deficit hyperactivity disorder (ADHD); for example, in one study 13/20 infants diagnosed with regulatory disorder could also receive a DSM diagnosis of ODD or ADHD.Reference Frankel, Boyum and Harmon18
The importance of axis II
The inclusion of an entire axis in DC:0-3 to describe relationship disorders, with a proposed assessment tool, the Parent Infant Relationship – Global Assessment Scale (PIR-GAS), allows assessment of relationship problems which may not have been addressed in any other evaluation of the child.Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15,Reference Emde and Wise24,Reference Stafford, Zeanah and Scheeringa27 It widens the thinking beyond the child, concentrating somewhere between the ‘child with the problem’ and the caregiver potentially as the ‘cause’ of the problem, and guides clinicians to investigate this complex relationship in a standardised and purposeful way.Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15 There already exist many ways to consider the infant-caregiver relationship, and it can be hard to distinguish the phenomenology in terms of relationship qualities, attachment and other descriptive concepts such as temperament. With regard to the attachment relationship, maternal sensitivity has been traditionally seen as a focus of importance:Reference De Wolff and van Ijzendoorn28 maternal insensitivity can be related to mental health outcomes in children, particularly aggression.Reference Alink, Mesman, van Zeijl, Stolk, Juffer and Bakermans-Kranenburg29 Temperament in infancy has also been related to childhood mental illness.Reference Kagan, Snidman, Zentner and Peterson30
Attachment disorders are placed in axis I because they are pervasive disorders identified within the child. In contrast, relationship disorders may be specific to the individual relationship between the parent-infant dyad. Maldonado-Duran et al Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15 consider how attachment disorders relate to relationship disorders: although attachment disorders are diagnosed in axis I where there has been historical evidence of maltreatment or deprivation, it may be argued that relationship disorders in infancy are closely related to the subsequent development of attachment disorders. There is also a question as to whether attachment disorders exist discretely, or whether attachment should be considered part of other disorders as an associated relationship disturbance.Reference Stafford, Zeanah and Scheeringa27 The DC:0-3R tool further clarifies that observation and evaluation of the current relationship is rated under axis II. The issue of the effect of inexperienced parents on the relationship has also been raised, although not included in DC:0-3.Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15
Assessment tools for the 0-3 age range
Assessments based on DSM-IV and DC:0-3 can still seem imperfect: there is a general lack of research into infant mental health disorders using DSM criteria, and a lack of reliability and validity using DC:0-3.Reference Kagan, Snidman, Zentner and Peterson30 Tools to assess infant mental health rely on observation of the infant and infant-carer relationship (PIR-GAS) and reports from informants, namely parents/carers (using the Child Behaviour Checklist (CBCL)Reference Rescorla31 and the Preschool Age Psychiatric Assessment (PAPA)Reference Egger, Angold, Delcarmen-Wiggens and Carter32): infants communicate largely non-verbally and are therefore unable to report on their own symptoms. There have been attempts to standardise parent report questionnaires in this age range using the CBCL and the Strengths and Difficulties Questionnaire (SDQ; www.sdqinfo.com). The CBCL now has a version for children as young as 18 months,Reference Rescorla31 and the SDQ has been adapted for age 2-3 years (R. Goodman, personal communication, 2011).
Observation of the relationship between the parent/primary caregiver and infant is essential for classification with DC:0-3. The description and guidance on the use of the PIR-GAS is detailed in DC:0-3R, along with another tool, the Relationship Problems Checklist (RPCL), to classify the quality of the relationship on axis II.16 In practice, the interaction between infant and caregiver is commonly recorded on video, for subsequent scoring with the PIR-GAS. The PIR-GAS is scored out of 100, where 81-100 represents an adapted ‘good enough’ relationship; 41-80 suggests a relationship at risk of dysfunction, and 40 or less represents a disordered relationship (i.e. a relationship disorder which can be coded under axis II).16,Reference Thomas and Guskin33 There is consensus that the overall assessment of an infant and parent should be approached from an ‘ecological’ perspective, observing the child and parent in different settings to take into account any situational variations which may affect the child at the time of assessment.Reference Maldonado-Duran, Helmig, Moody, Fonagy, Lartigue and Sauceda-Garcia15 The PIR-GAS seems to be particularly valuable in detecting internalising symptoms.Reference Thomas and Guskin33,Reference Aoki, Zeanah, Scott Heller and Bakshi34
The parent-reported CBCL 1.5-5Reference Rescorla31 includes a language development screening tool to link whether a child with language problems may also have behavioural/emotional problems, and aims to maintain DSM-based diagnostic scales with seemingly good reliability and validity; its use is suggested as a preclinical assessment tool. The PAPA is a structured parent interview using DSM and DC:0-3 principles to diagnose children aged 2-5 years,Reference Egger, Angold, Delcarmen-Wiggens and Carter32 developed to further address the diagnostic challenges in young children. The Diagnostic Infant and Preschool Assessment (DIPA)Reference Scheeringa and Haslett35 is another caregiver-reported tool that follows DSM criteria to assess children aged 1-6 years; it has shown good agreement in concurrent criterion validity to the CBCL 1.5-5 and is more concise than the PAPA.
Reliability of diagnosis in infancy
Several authors have compared and contrasted DC:0-3 with DSM or ICD systems. Frankel et al Reference Frankel, Boyum and Harmon18 used both DSM-IV and DC:0-3 to diagnose the same sample of patients in their general infant patient group, and suggested good concordance between the two systems for axis I disorders. Another study looked at the reliability of use of ICD-10 and DC:0-3 in 1.5-year-old infantsReference Skovgaard, Christiansen and Andreasen36 and found greater interrater reliability and test-retest reliability using DC:0-3, but demonstrated that ICD-10 in infants also provides good reliability. With regard to the PIR-GAS, there was 100% agreement between raters, suggesting it is a reliable assessment tool for axis II.Reference Skovgaard, Christiansen and Andreasen36
Stafford et al Reference Stafford, Zeanah and Scheeringa27 reviewed two diagnostically challenging conditions in young children (RAD and PTSD) and their classification in different systems. The authors comment that infants may present with PTSD symptoms but not fulfil DSM-IV criteria due to their non-verbal communication (i.e. not being able to describe the subjective experience), therefore DC:0-3 included more ‘behaviourally anchored’ criteria. The authors also favour DSM-IV for diagnosing RAD (as ‘a within-child disorder’), due to the lack of criteria in DC:0-3, although they acknowledge the benefits of considering relationship problems in general as part of axis II of DC:0-3. When considering the symptoms of these disorders and how they present within certain developmental stages, Stafford et al Reference Stafford, Zeanah and Scheeringa27 criticise DC:0-3 for not accounting for age and developmental capabilities. As a result of these diagnostic challenges, some of the main changes from DC:0-3 to DC:0-3R include: changing RAD to deprivation/maltreatment disorder, separating it from possible axis II classifications regarding the attachment relationship; and consolidating PTSD as a disorder in DC:0-3R, where traumatic stress disorder stood before, allowing more analogy with DSM-IV and adding in extra diagnostic criteria for infants.16 Another significant revision was the restricted use of multisystem developmental disorder to infants under the age of 2 years, accounting for the increase in research on autism spectrum disorders demonstrating a diagnosis can be made from the age of 2.16,Reference Carr, Lord and Zeanah37 This could support the view that in infants younger than 2 years a broader view of neurodevelopmental disorders should be taken, in line with the ESSENCE concept.Reference Gillberg1
It may be that DC:0-3R and other infant assessment tools should marry with, and not replace, existing classification systems: the DC:0-3R, although filling in gaps with specific infant disorders not found in DSM and ICD systems, has a clinical focus and could be balanced by stricter research- and evidence-based approaches like the RDC-PA.Reference Postert, Averbeck-Holocher, Beyer, Muller and Furniss38
Implications for mental health services
At the moment, generic child psychiatric services may be struggling to assess infants, despite a general interest in early intervention on the research and political levels,Reference Scott, Knapp, Henderson and Maughan9 perhaps because services are overstretched to manage their existing child and adolescent patients. Early difficulties such as sleeping, behaviour or feeding problems often fall to health visitors to manage and child psychiatrists might feel inadequately trained in assessing and treating infant mental health problems. Interestingly, there is some evidence to suggest that infant mental health problems could be predicted during a routine general health surveillance carried out by non-mental health professionals in early infancy, potentially identifying infants at risk of mental health problems in early life.Reference Skovgaard, Houmann, Christiansen, Olsen, Landorph and Lichtenberg39 Perinatal services remain focused on maternal mental health as their main priority:Reference Austin and Priest40 although some monitoring of the mother-baby relationship occurs in an in-patient setting with mothers with the most severe illness, any out-patient work around this is generally performed by health visitors and social work agencies. Parenting capacity and child protection are paramount across psychiatry: Milburn et al Reference Milburn, Lynch and Jackson41 highlight the process of assessment of these factors with parents and children of all ages, especially infants in vulnerable families, with consideration towards involvement of statutory measures where necessary. Infant mental health is just starting to reach the curriculum for child psychiatrists in training, although hands-on experience is lacking.




eLetters
No eLetters have been published for this article.