Depression is a major mental health problem in the older population. Reference Lebowitz, Pearson, Schneider, Reynolds, Alexopoulos and Bruce1 A study in nine European countries found an average prevalence rate of depression of 12% in people over 64 years of age. Reference Copeland, Beekman, Dewey, Hooijer, Jordan and Lawlor2 Evidence suggests that depression in this population is associated with functional impairment, increased risk of dementia, raised mortality and more admissions to psychiatric in-patient care. Reference Beekman, Deeg, Braam, Smit and Van Tilburg3–Reference Van Citters and Bartels7 Given the demographic changes with a rising proportion of elderly people in Western societies, depression in older adults poses a major and increasing challenge to public mental health. Reference Bartels, Dums, Oxman, Schneider, Aréan and Alexopoulos8,Reference Klug, Hermann, Fuchs-Nieder, Stipacek, Götz and Wallner9
Substantial evidence shows that antidepressant medication and psychological treatments such as cognitive–behavioural therapy can be effective in treating elderly patients with depression. Reference Bartels, Dums, Oxman, Schneider, Aréan and Alexopoulos8,Reference Mitchell and Subramaniam10 Less research, however, has focused on how these interventions should be delivered and whether it is more beneficial to provide them in patients' homes than in institutions. Reference Van Citters and Bartels7,Reference Cuijpers11,Reference Unützer and Bruce12–Reference Draper and Low14 Most existing trials testing models of home treatment for elderly people with depression focused on individuals living in residential care and nursing homes rather than on those who still manage to live independently. Research on the latter group appears particularly important since maintaining independent living may be seen as a major treatment goal for many individuals. Reference Van Citters and Bartels7,Reference Klug, Hermann, Fuchs-Nieder, Stipacek, Götz and Wallner9,Reference Draper and Low14,Reference Wertheimer15
A pilot study indicated that geriatric home treatment delivered by a multidisciplinary team is feasible and might be associated with positive clinical and functional outcomes over a 1-year period. Reference Klug, Hermann, Fuchs-Nieder, Stipacek and Zapotoczky16 The aim of this subsequent trial was to test the clinical effectiveness and costs of geriatric home treatment in treating elderly people with depression who live independently in the community, assessing outcomes after 3 and 12 months.
Method
The randomised controlled trial investigated whether geriatric home treatment would be associated with lower levels of depression, better functioning, more positive subjective quality of life, fewer admissions to nursing homes, shorter duration of psychiatric in-patient care and lower care costs compared with conventional psychiatric out-patient care (as it is routinely provided in Austria) over a 1-year period.
Setting
The study was conducted in Graz, a town in Austria with a population of 250 000. All potential participants received full routine care within the Austrian healthcare system. The additional experimental service was provided by a publicly funded voluntary organisation specialising in mental health services in the community (Psychosocial Services Graz). All psychiatric in-patient, out-patient and community services in the area could refer individuals to the new home treatment model.
Participants
Participants were consecutive referrals to the service meeting the following inclusion criteria: over 64 years of age; a primary diagnosis of major depression according to ICD–10; 17 moderately impaired global functioning, i.e. a score on the Global Assessment of Functioning Scale (GAF) Reference Saß, Wittchen, Zaudig and Houben18 of between 21 and 60; living independently in Graz; and capacity to provide informed consent. Exclusion criteria were: symptoms of dementia, i.e. a score on the Mini-Mental Status Examination Reference Folstein, Folstein and McHugh19 of less than 27; and an intention by the individual to give up independent living and move to a nursing home.
Design, recruitment and randomisation
Following referral to the service, all individuals were assessed. Those who were eligible for the study were asked to participate. Written informed consent was obtained from all participants. Consenting participants were then randomly allocated to geriatric home treatment or conventional out-patient care. Randomisation was done by a researcher who was otherwise not involved in the study using random tables.
Intervention
All participants in both conditions had free access to all aspects of care as routinely provided in the Austrian healthcare system, including input from general practitioners, psychiatrists, social workers, day centres with social and occupational activities, and, if required, nursing care in the individual's home.
Participants in the intervention group additionally received geriatric home treatment over a 1-year period. Geriatric home treatment was delivered by a multidisciplinary team consisting of one psychiatrist with a psychotherapeutic qualification, two psychologists and one social worker who was also qualified as a psychiatric nurse. The team had already participated in the pilot study Reference Klug, Hermann, Fuchs-Nieder, Stipacek and Zapotoczky16 and was trained in geriatric home treatment. The team worked Monday to Friday from 08.00 h to 17.00 h and routinely visited each participant once or twice a week. In crisis situations, up to four visits per week were arranged. Additionally, there was telephone contact with the individual and, if applicable, the carer. The components of geriatric home treatment are talks about self-esteem, coping resources and medication adherence; encouragement and practical support for the individual to establish and maintain social networks, increase social and leisure activities and cope with tasks of daily living; support of carers; and crisis interventions when required. For each participant in the geriatric home treatment group an individual care plan was designed.
Participants in the control group received conventional psychiatric out-patient care as it is routinely provided through office-based practices in Austria and other countries such as Germany. In such a system, individuals have free and direct access to out-patient consultations with consultant psychiatrists, which are commonly arranged without any significant waiting time. Individuals can be referred to other services in the community by their psychiatrist or access them directly. These services are also free at the point of entry. Psychiatrists and other services can undertake domiciliary visits, but this happens only very rarely. In addition to routine out-patient care, all participants in the control group had an initial meeting with a psychologist, in which they were provided with detailed information about all available health and social services in the area and ways to access them.
Data collection
Participants were assessed at baseline, after 3 months and after 12 months. The pre-randomisation assessment was conducted by a psychiatrist. This included establishing the clinical diagnosis according to ICD–10 and applying the Mini-Mental State Examination. Reference Folstein, Folstein and McHugh19,Reference Feldman, Jacova, Robillard, Garcia, Chow and Borrie20 All other assessments were conducted by two trained interviewers who were not involved in the care of any of the participants.
Outcomes
Symptom levels of depression as a primary outcome were self-rated on the 15-item Geriatric Depression Scale (GDS–15). Reference Marc, Raue and Bruce21,Reference Sheikh, Yesavage and Brink22 Scores between 5 and 8 suggest a mild depression, scores between 9 and 11 a moderate depression, and scores between 12 and 15 a severe depression.
The level of functioning was observer rated on the GAF, which ranges from 0 (worst functioning) to 100 (best functioning). Reference Saß, Wittchen, Zaudig and Houben18 Subjective quality of life (SQOL) was assessed on the short form of the Berlin Quality of Life Profile (BELP–KF), Reference Kaiser, Isermann, Hoffmann, Huxley and Priebe23 which is a modified German version of the Manchester Short Assessment of Quality of Life. Reference Priebe, Huxley, Knight and Evans24 Similar to the Quality of Life Interview Reference Lehman25 and the Lancashire Quality of Life Profile, Reference Oliver26 participants rate their satisfaction with life in general and different life domains on scales ranging from 1 (extremely dissatisfied) to 7 (extremely satisfied). The mean score of 14 satisfaction items was taken as the score for SQOL.
Admissions to nursing homes and days spent in psychiatric in-patient care were reported by the participants and cross checked with the given institution by the interviewer.
Costs of care in both groups included costs for psychiatric in-patient care (daily fees of €520.50 as defined for the Austrian province of Styria) 27 and nursing homes (average daily costs of €112.11 as provided by Social Care Authority in Graz). 28 In the intervention group we also considered the additional costs for the input of psychologists, social workers, nurses (fees defined by regional legislation) 29 and psychiatrists (reflecting the agreed salaries and overhead costs in the region) in geriatric home treatment. The costs were calculated as a proportion of the budget for the given professional group in the service. They reflect the actual time that the professional groups spent in the care of each participant.
Statistical analysis
We used SPSS for Windows 16 to compare the intervention and control groups in an intention-to-treat analysis. Descriptive statistics are presented, with frequency and percentage distributions for categorical data and means, and for continuous data with standard deviations or 95% confidence intervals respectively.
Outcomes on depressive symptoms, global functioning and SQOL were compared in separate covariance analyses (ANCOVAs) for the follow-ups at 3 months and 12 months. Baseline scores of the chosen outcome criterion were included as a covariate. Admissions to psychiatric nursing homes were analysed using a chi-squared test.
To compare days in psychiatric in-patient care and costs of care, a non-parametric bootstrap procedure was applied. The sampling distribution of mean differences collected the values of such differences from 10 000 samples by repeatedly sampling with replacement from the observed random sample. Statistical inferences whether means differed significantly were drawn by constructing a 95% CI for the observed mean difference. Reference Efron and Tibshirani30 The bootstrapped confidence intervals were constructed using the ‘boot’ package version 1.2-43, as implemented in R for Windows. 31
Sample size and ethical approval
For the sample size calculation, we hypothesised a difference of two-scale points on the GDS–15 that corresponds to an effect size of f = 0.35, Reference Canuto, Meiler-Mititelu, Herrmann, Delaloye, Giannakopoulos and Weber32,Reference Hayman, Kerse, La Grow, Wouldes, Robertson and Campbell33 which is regarded as a medium to large effect size. To detect such a difference at a 5% significance level with 80% power, a sample size of 54 was required. Assuming a drop-out rate of 10% between baseline and follow-ups, the sample size was determined as 60, with 30 participants in each arm. Ethics approval for the study was obtained from the ethics committee of the Medical University Graz (trial registration number EK 13-209 ex 02/03).
Results
Participant flow
The participant flow is shown in Fig. 1. Out of 60 randomised participants, 41 had been referred by psychiatric hospital departments following an episode of in-patient treatment, 8 each from psychiatrists working in private office practice, and 3 from other community services. At 3 months, 58 participants were re-interviewed and at 12 months 51 participants. Between baseline and 12-month follow-up, seven participants dropped out in the control group and two in the geriatric home treatment group.
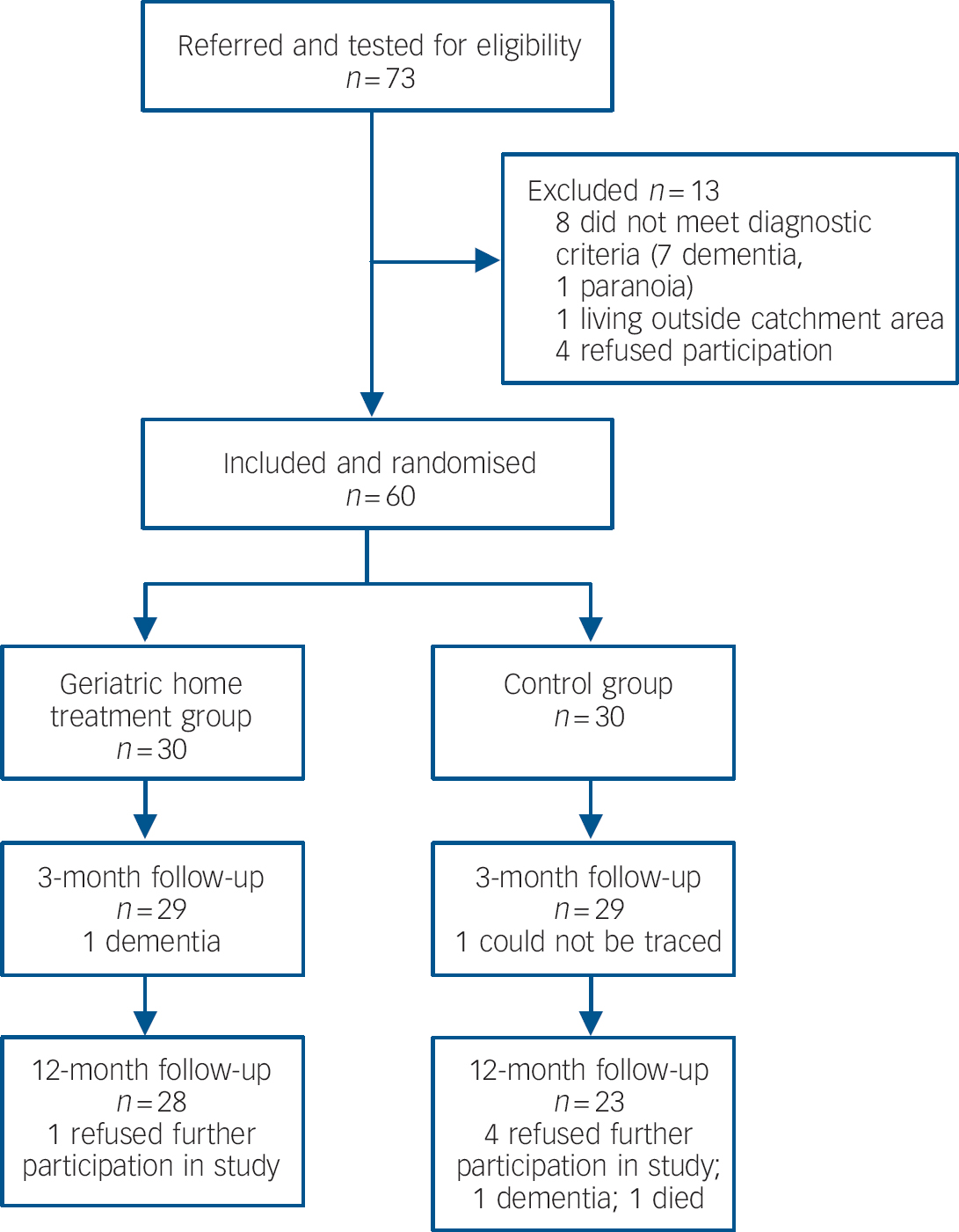
Fig. 1 Participants' flow through the trial.
Baseline characteristics of participants and treatment received
The baseline characteristics of participants in the two groups are shown in Table 1. On average, participants were about 75 years of age. Most were female and living alone. There were no significant differences in the sociodemographic and clinical characteristics of participants in the intervention and control groups. Within the observation period, all of the followed-up participants in both groups were seen by a general practitioner and were prescribed antidepressant medication. All participants in the geriatric home treatment group and 20 out of 23 participants in the control group were seen at least once by a psychiatrist in office practice.
Table 1 Baseline characteristics of participants in the intervention group (geriatric home treatment) and the control group (conventional out-patient care)

| Characteristics | Geriatric home treatment group (n = 30) | Control group (n = 30) | Total sample (n = 60) |
|---|---|---|---|
| Gender, female/male: n (%) | 28/2 (93/7) | 26/4 (87/13) | 54/6 (90/10) |
| Age, years: mean (s.d.) | 74.3 (7.3) | 75.5 (5.7) | 74.9 (6.5) |
| Living alone, n (%) | 21 (70.0) | 26 (86.7) | 47 (78.3) |
| Receiving antidepressant medication, n (%) | 29 (97) | 28 (93) | 57 (95) |
| Mini-Mental State Examination, mean (s.d) | 29.3 (0.9) | 29.3 (0.9) | 29.3 (0.9) |
For participants in the intervention group, geriatric home treatment provided a mean of 78.2 activities (s.d. = 98.6), which included direct or telephone contacts with the individual and contacts with carers and other agencies. Participants received on average 50.8 home visits (s.d. = 45.1), i.e. about one visit per week, through the geriatric home treatment team. Of these, on average 3.67 visits (s.d. = 9.91) were crisis interventions, and on average 2.0 times (s.d. = 2.6) a psychiatrist participated in the home visit. Out of all participant-related activities in geriatric home treatment, 63.6% were conducted by psychologists, 29.0% by a social worker or nurse, and 7.4% by a psychiatrist.
Outcomes
The findings on symptom levels of depression, global functioning and SQOL are shown in Table 2. On average, symptoms of depression showed a slight deterioration in the control group and a marked improvement in the intervention group. The difference between the two groups was statistically highly significant at both 3 and 12 months. When the analyses were repeated adjusting for living status, gender and age, the differences between the two groups remained significant.
Table 2 Scores of Geriatric Depression Scale, Global Assessment of Functioning Scale, and Berlin Quality of Life Profile (subjective quality of life) for the intervention group (geriatric home treatment) and the control group (conventional out-patient care) at baseline, 3 months and 12 months, and results of covariance analyses with the baseline score of the outcome as covariate
| Geriatric home treatment group Mean (95% CI) | Control group Mean (95% CI) | F | P | |
|---|---|---|---|---|
| Geriatric Depression Scale | ||||
| Baseline | 9.29 (8.41–10.39) | 8.52 (7.75–10.12) | ||
| 3 months | 6.82 (5.69–7.72) | 9.70 (9.08–11.10) | 22.3 | <0.001 |
| 12 month | 6.11 (4.98–7.20) | 10.43 (9.28–11.69) | 29.7 | <0.001 |
| Global Assessment of Functioning Scale | ||||
| Baseline | 50.2 (46.2–53.3) | 54.8 (50.9–56.0) | ||
| 3 months | 58.4 (56.5–62.0) | 51.5 (46.4–51.9) | 26.2 | <0.001 |
| 12 month | 61.9 60.3–65.5) | 49.7 (45.5–51.3) | 53.1 | <0.001 |
| Subjective quality of life | ||||
| Baseline | 3.85 (3.52–4.17) | 4.29 (3.85–4.61) | ||
| 3 months | 4.51 (4.41–4.83) | 3.86 (3.45–3.88) | 40.0 | <0.001 |
| 12 months | 4.77 (4.60–5.11) | 3.45 (3.06–3.63) | 61.9 | <0.001 |
In the control group, global functioning remained largely unchanged and SQOL scores deteriorated. In the intervention group, both global functioning and SQOL showed improved scores at 3 months and 12 months. The differences between the two groups were statistically significant for each outcome and at each point of time.
In the geriatric home treatment group, one person was admitted to a nursing home. The admission was temporary and the individual was discharged after 37 days. In the control group, eight participants were admitted to a nursing home, seven of them stayed there until the end of the study. The difference in the number of admissions is statistically significant (χ2 = 6.41, P = 0.011). Participants in the intervention group spent on average 19.6 days (s.d. = 6.8) in psychiatric in-patient care, whereas participants in the control group spent 52.2 days (s.d. = 46.8) in psychiatric in-patient treatment. For the observed mean difference of 17.60 the corresponding bootstrap 95% CI was 3.68–31.52, which reflects a statistically significant difference.
Costs
Over 1 year, mean costs per participant in the geriatric home treatment group were €1821.75 (95% CI 189.92 to 3453.58) for psychiatric in-patient care and €148.15 (95% CI –155.82 to 452.11) for nursing homes. In conventional out-patient care, the mean costs were €13 125.65 (95% CI 3403.73 to 22 847.57) for psychiatric hospital treatment and €7906.19 (95% CI 1379.41 to 14 432.98) for care in nursing homes. The additional mean costs in the geriatric home treatment group were €5717.28 (95% CI 3370.88 to 8063.68) for the input of psychologists, social workers and nurses, and €1064.26 (95% CI 503.74 to 1624.79) for the input of psychiatrists. The total costs of care per participant were therefore €8751.44 (95% CI 5995.59 to 11507.29) for the geriatric home treatment group and €21 031.84 (95% CI 10 091.93–31 971.76) for the control group. For the observed mean difference of 12 280.40 the corresponding bootstrap 95% CI was 1859.00–22 701.80, indicating a statistically significant difference.
Discussion
Main findings
Geriatric home treatment was associated with lower depression scores, better global functioning and a more favourable SQOL after 3 and 12 months. The effect sizes in favour of geriatric home treatment were large and clinically significant. Participants in the geriatric home treatment group also had fewer admissions to nursing homes and spent fewer days in psychiatric in-patient care. Because of the successful prevention of admissions to psychiatric in-patient care and nursing homes, geriatric home treatment was associated with substantially lower care costs. As compared with conventional psychiatric out-patient care, geriatric home treatment can be seen as a very effective and cost-effective form of treatment. The benefits are already substantial after 3 months and are even more marked after a 12-month period.
Strengths and limitations
Strengths of the study are that it was conducted as a pragmatic trial in a routine service and that the effect was established on different outcome criteria including observer and self-ratings. A further strength is that the control condition of conventional psychiatric out-patient care was a freely accessible and well-developed system of health and social care in Austria.
There are also several limitations. Interviewers were not masked to the allocation of the individuals, which might have influenced observer ratings more than the objective outcome criteria of admissions to nursing homes, time spent in psychiatric in-patient care and costs. The trial was conducted at only one site so that it remains unclear to what extent the findings may depend on context-specific factors and can be replicated elsewhere. Finally, the cost analysis did not consider all aspects of care. In particular, the costs of conventional out-patient consultations were not assessed. This, however, would have shown even higher costs in the control condition and not altered substantially the cost findings of the study. Also, the costs of non-mental healthcare were not considered.
Comparison with the existing literature
Some research has been conducted on home treatment for elderly people, mostly with individuals with dementia or mixed samples. Reference Bartels, Dums, Oxman, Schneider, Aréan and Alexopoulos8,Reference Stuck, Egger, Hammer, Minder and Beck34 A systematic review Reference Stuck, Egger, Hammer, Minder and Beck34 on the effect of home visits in elderly people in general showed only modest and non-significant gains in reducing the risk of admission to nursing homes. In our study, however, we specifically targeted individuals with depression. Most previous experimental or quasi-experimental studies with samples consisting only of participants with depression tested treatment delivery in residential facilities or nursing homes and these suggest largely positive results. Reference Van Citters and Bartels7
A trial in the UK Reference Banerjee, Shamash, Macdonald and Mann35 tested multidisciplinary home care in frail elderly people with depression who lived independently. After a 6-month period, the intervention group had significantly lower levels of depression. Reference Banerjee, Shamash, Macdonald and Mann35 Although our study was conducted with a different target group (participants were not frail), in a different context and over a longer period of time, the findings may be seen as consistent with and adding to those of the UK study.
All participants in both groups in this study were prescribed antidepressant medication. One can only speculate as to whether geriatric home treatment led to a better medication adherence and what difference in outcomes may have been as a result of the psychosocial components of geriatric home treatment and the crisis interventions. A meta-analysis Reference Cuijpers11 suggests that psychological interventions for elderly people with depression that are delivered in the community may indeed be effective in improving symptoms. Geriatric home treatment is a complex intervention Reference Campbell, Fitzpatrick, Haines, Kinmonth, Sandercock and Spiegelhalter36 that is not restricted to using a specific psychological model and includes various types of practical support and crisis interventions in addition to psychological work. Participants in the geriatric home treatment group received on average more than three crisis interventions within the 1-year period, which may have been particularly helpful in avoiding hospital admissions.
The findings of this study suggest that the effect of geriatric home treatment is maintained over a 1-year period. It was already substantial after the initial 3-month period and increased further during the year. To what extent the benefit may be sustained or even improved over longer periods of time needs to be addressed in further research.
Implications
In many countries, community service models for elderly people are less well developed than those for individuals of working age. Reference Beekman, Deeg, Braam, Smit and Van Tilburg3,Reference Wertheimer15 The findings of this study suggest that investment in services delivering home treatment might lead to much improved clinical and social outcomes. Geriatric home treatment appears effective not only in reducing symptoms and improving individuals' SQOL, but also in preventing admissions to nursing homes and psychiatric hospitals. This is a great benefit for the individuals concerned. Geriatric home treatment was not only associated with more positive clinical outcomes, but also with substantially lower costs of care. The intervention therefore appears highly cost-effective and the study supports the case for investing in such services as an intervention to improve outcomes and reduce costs.
The findings of the trial are very positive and encouraging, but should be replicated in other settings and with larger samples, and future studies may consider follow-up periods of more than a year. Further trials may also identify the most relevant ingredients of geriatric home treatment so that the model can be improved and be made more efficient.






eLetters
No eLetters have been published for this article.