Lesbian, gay, bisexual, transgender, and queer (LGBTQ+) adults face unique individual stressors because of their sexual orientation and gender identity (SOGI) including self-stigma, expectations of rejection, and/or concealment of SOGI. Reference Meyer1 Moreover, persons who identify as LGBTQ+ experience a greater number of interpersonal stressors (e.g. discrimination, family rejection, and violence) Reference Havranek, Mujahid and Barr2 associated with higher rates of substance use, Reference McCabe, Hughes and Matthews3 poor mental health, Reference Klein and Golub4 and cardiometabolic risk Reference Caceres, Veldhuis, Hicket and Hughes5 throughout their lifetime. Similar to other underrepresented and stigmatized minorities, these structural stressors lead to cardiovascular morbidity and mortality in LGBTQ+ adults. Understanding the relationships between gender minority stress and cardiovascular disease in LGBTQ+ people is critical to the development of therapeutic interventions and strategies to reduce cardiovascular disease specific to this patient population.
To date, there are few published data on the cardiovascular health of sexual and gender minority adults. This is largely due to an absence of the collection of data beyond the binary (male, female) sex in current cardiovascular studies. The collection of SOGI data from patients and the entry of this data into the electronic medical record (EMR) have been recommended by the Institute of Medicine, 6 the Joint Commission, 7 and policy experts as key steps to reduce disparities among the LGBTQ+ population. However, these policies do not require physicians to collect this information. 8 Consequently, failure to discuss SOGI with patients will continue to perpetuate the invisibility of the LGBTQ+ community in clinical settings and create larger disparities in cardiovascular health for these patients.
Despite the advantages of SOGI data collection, barriers to SOGI data collection include physician misperception that patients do not want to answer these questions, Reference Cahill and Makadon9 the inability of most EMRs to accommodate SOGI data, Reference Cahill, Baker, Deutsch, Keatley and Makadon10 and the lack of educational guidance on collecting SOGI data. Despite these roadblocks, notably the lack of cardiovascular healthcare providers asking SOGI questions, no prior studies have assessed whether patients with cardiovascular disease would be upset or offended by SOGI questions. Therefore, the aim of this study was to assess patient comfort with being asked SOGI questions in five outpatient adult congenital heart disease (ACHD) clinics in the United States.
Materials and methods
Participants were recruited from five quaternary ACHD centres across the United States (MA, IN, TX, CA). Participant eligibility included patients 18 years of age or older with CHD, connective tissue disease, or congenital cardiomyopathy, who were able to read and comprehend written English. Surveys (Appendix) were voluntarily administered in private patient rooms to ensure survey confidentially. The IRB approved the study at each institution, and all participants provided written informed consent. This one-time survey administered to participants included a two-step gender identity and birth sex question endorsed by transgender researchers in the United States 11 as well as a question about sexual orientation adopted by Fenway Health. Reference Bradford, Cahill, Grasso and Makadon12 This item was followed by a question regarding pronouns usage: “he/him/his,” “she/her/hers,” “they/them/theirs,” and “other.” Respondents were then asked questions to determine patient comfort surrounding SOGI questions and whether SOGI data might influence healthcare needs. Finally, sociodemographic data including race/ethnicity, level of education, and CHD complexity were obtained.
Respondents with simple, moderate, or great complexity conditions and non-missing education data were used for analysis. Pearson’s chi-square tests were used to compare differences in survey question responses between categories of age, education, and CHD complexity and region (Indiana and Texas versus Massachusetts and California). These groupings were selected to determine if regional LGBTQ+ public policy changes might impact how patients respond to SOGI questions. Agreement with survey questions of “patient’s discussion of SOGI might impact upon specific health care needs” and “patient’s disclosure of sexual orientation might improve communication between patient and physician” were of primary interest and were each modelled using logistic regression. Age, education, complexity, and region were independent variables in bivariate models of agreement with the two statements. Variables that had a p-value of 0.3 or smaller in the bivariate models were included in the multiple regression model.
Results
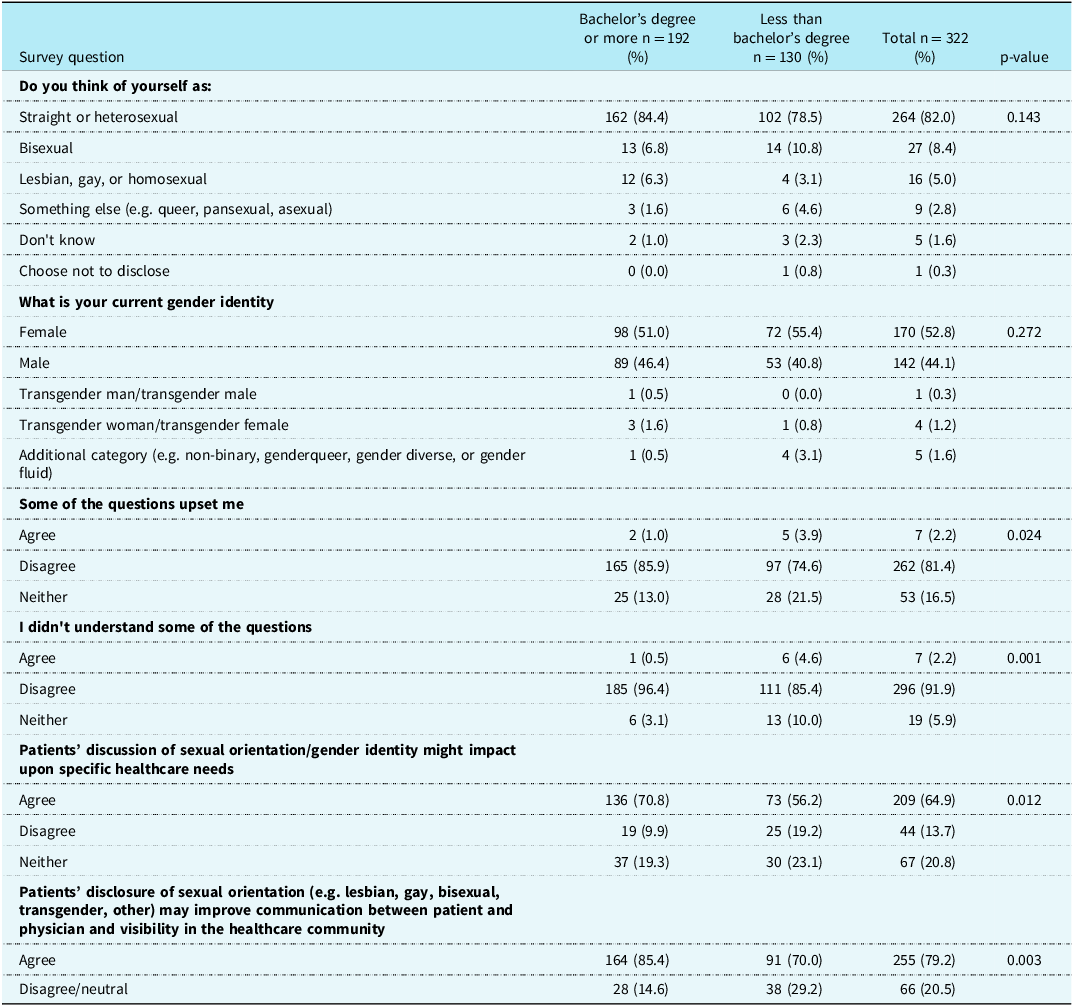
Of the 322 patients enrolled, nearly half were between the ages of 30 and 49 years (47.7%) with CHD of moderate complexity (49.7%). Although the majority of the study participants identified as straight or heterosexual (82.1%), a higher percentage (16.2%) identified as LGBTQ+ compared to the general population (7.2%). 13 Table 1 provides SOGI data on all participants by age group. Table 1 provides complete demographic information on all participants. Table 2 shows comparisons of survey questions by education.
Table 1. Demographic characteristics of participants surveyed, adult congenital patient self-identification by sexual orientation, and gender identity by age group

Table 2. Survey questions by education
Patient comfort regarding SOGI data collection
Most patients (90.4%) felt comfortable answering SOGI questions (Figure 1). The percentage of feeling comfortable did not significantly differ by age, CHD complexity, level of education, or region. Only 2.2% of respondents reported that answering SOGI questions “upset” them (Figure 2). No statistically significant differences in the percent upset by SOGI questions were seen with regard to age, CHD complexity, or regional comparisons. A significantly greater percentage of patients with at least a bachelor’s degree disagreed with the statement that some of the questions upset them than did those with less education (85.9% versus 74.6%, p = 0.024, see Table 2).

Figure 1. Participant response to, “I felt comfortable answering SOGI questions.”
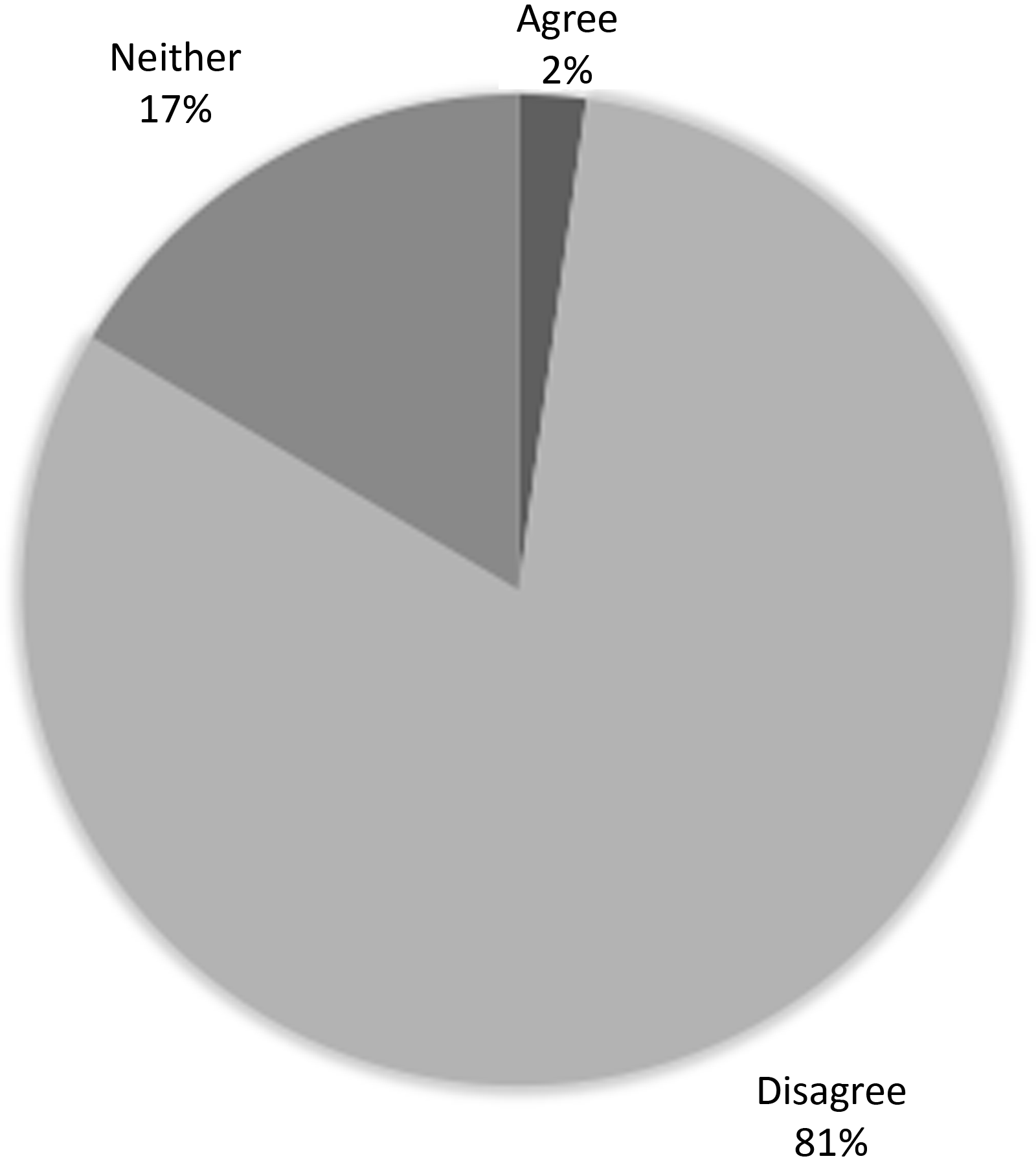
Figure 2. Participants response to, “Responding to SOGI questions ‘upset’ me.”
Patient perceived benefits of SOGI collection
Over half of respondents (62.4%) agreed that SOGI data is important for ACHD physicians to know about ACHD patients, and the percentage who agreed did not differ significantly by any of the four demographic and clinical characteristics we analysed. Sixty-five percent of patients agreed with the statement “Patient discussion of SOGI might impact upon specific health care needs.” The percentage who agreed to this statement did not differ by age, CHD complexity, or region. A significantly greater percentage of patients with at least a bachelor’s degree agreed with the statement than did those with less education (70.8% versus 56.2%, p = 0.012, see Table 2). Bivariate models of agreement with the question “Patient discussion of SOGI might impact upon specific health care needs” estimated that patients with a bachelor’s degree or higher were 83% more likely to agree (OR = 1.83; 95% CI 1.15, 2.92; p = 0.0115) with this statement than those with less education. The multiple regression model of agreement with the statement included education, region, and complexity. Adjusted for CHD complexity, respondents with bachelor’s degrees were significantly more likely to agree with the statement (OR = 1.97; 95% CI 1.20, 3.23; p = 0.0074) as were those from Indiana and Texas (OR = 1.74; 95% CI 1.06, 2.85; p = 0.0292) (see Table 3).
Table 3. Models of SOGI discussion and impact on health
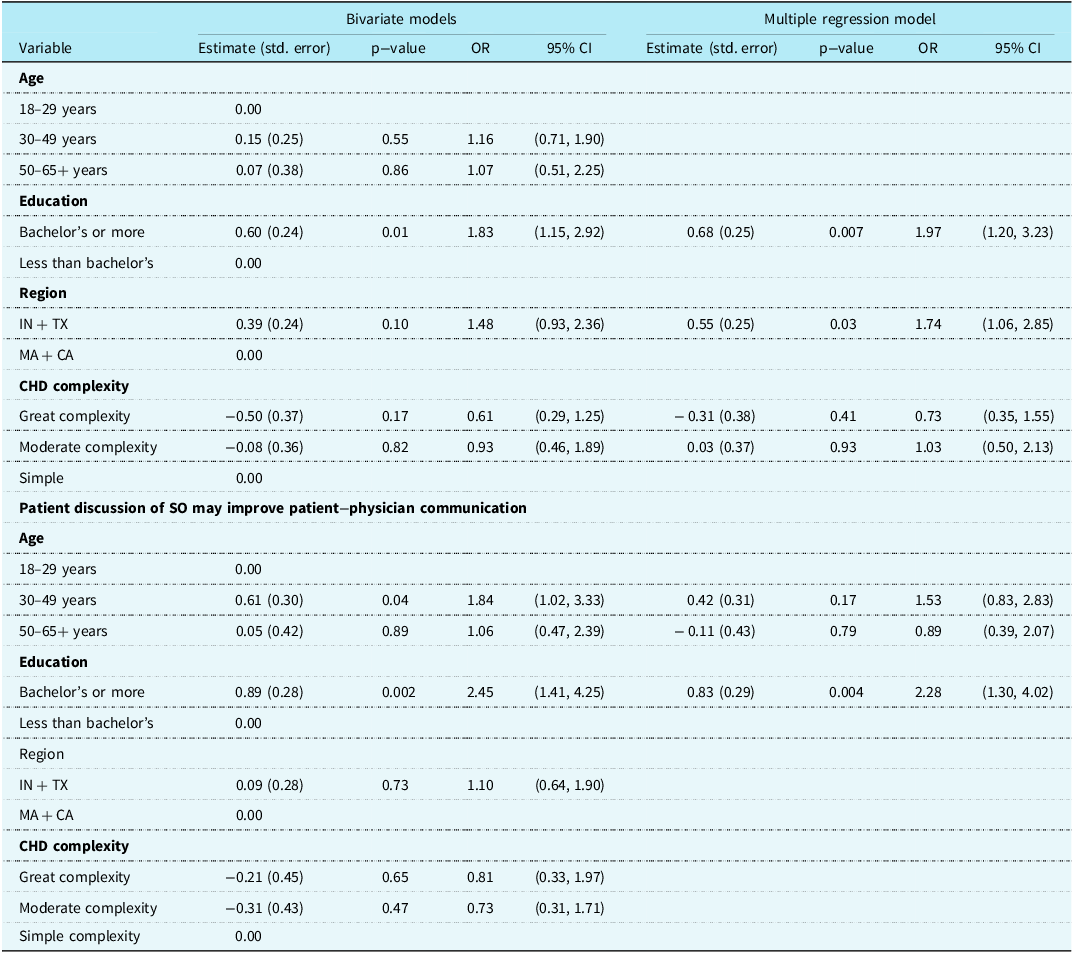
CA = California; CHD = Congenital heart disease; IN = Indiana; MA = Massachusetts; OR = odds ratio; SOGI = sexual orientation, gender identity; TX = Texas.
Seventy-nine percent of patients agreed with the statement “Patient disclosure of sexual orientation may improve communication between patient and physician and visibility in the healthcare community.” Comparisons of agreement did not differ significantly between age, CHD complexity, or region. A significantly greater percentage of patients with at least a bachelor’s degree agreed with the statement than did those with less education (85.4% versus 70.0%, p = 0.003). The bivariate models for agreement with the statement showed that respondents having a bachelor’s degree of higher were 2.5 times more likely to agree (OR = 2.45; 95% CI 1.41, 4.25; p = 0.0015). Adjusting for age, respondents who had a bachelor’s degree or higher were still 2.3 times more likely to agree with this statement (OR = 2.28; 95% CI 1.30, 4.02; p = 0.0043).
Discussion
This is the first study to assess patient comfort regarding SOGI data collection in a cardiology clinic (e.g. ACHD clinic). A key finding in this study is that a largely heterosexual cohort of ACHD patients across several outpatient clinics felt comfortable answering SOGI questions. Additionally, given the awareness of the importance of intersectionality in sexual and gender minority patients, it is notable that our patient population was racially diverse. These findings are similar to those from patients surveyed in urology and oncology clinics with standardized SOGI questions in addition to EMR-expanded gender identity questions; Reference Rosser, Polter and Chandiramani14 however, this was one of the first studies to determine that patient-centred sexual orientation data in the EMR was acceptable, understandable, and feasible for almost all patients. The Emergency Department Query for Patient-Centered Approaches to Sexual Orientation and Gender Equality (EQUALITY) study tested two different approaches to SOGI collection among four emergency departments and assessed whether either method was associated with higher patient satisfaction with their ED experience. Reference Haider, Adler and Schneider15 Phase I of the EQUALITY study demonstrated that 80% of clinicians believed that patients would refuse to provide SOGI data, yet only 10% of patients reported that they would refuse to do so. Reference Haider, Schneider and Kodadek16 Another key finding of this study was that sexual and gender minority patients reported greater comfort when SOGI data was collected via non-verbal self-report. This suggests that sexual and gender minority patients prefer a standardized collection process where all patients can report SOGI information in addition to other demographic data compared to being asked by a nurse during their clinical encounter thus providing culturally relevant care.
In this study, 16.2% of ACHD patients identified as LGBTQ+. Although this only represents a small sample of ACHD clinics in the United States, that is more than two times the prevalence of the LGBTQ+ population in the United States. This is not surprising as an increasing number of younger adults continue to come to terms with their own sexuality and gender identity compared to older generations. The data in our study reflects similar information collected by Gallup public-opinion polls in the United States, as follows: (1) LGBTQ+ identification is highest among younger generations; (2) the proportion of bisexual adults relative to other LGBTQ+ identities is higher in younger than older age groups; and (3) in older age generations, LGBTQ+ individuals are more likely to identify as gay. 13
While this study identifies a sizeable demographic of LGBTQ+ adult patients with CHD, the number of LGBTQ+ cardiologists (ACHD)—including within the field of ACHD—is unknown. The current studies evaluating the demographic status of cardiologists in the United States have yet to collect gender data beyond binary (male, female) sex. Reference Mehta, Fisher and Rzeszut17 Although there has been a push for diversity and inclusion in cardiology, this study demonstrates the need for LGBTQ+ physicians and supportive allies in cardiology. Available data from LGBTQ+ trainees report the importance of having LGBTQ-identified mentors for personal and professional development. Reference Sanchez, Rankin and Callahan18 From the patient’s perspective, disparities in LGBTQ+ health care are driven by a lifetime of mistreatment within the healthcare system. Data from the PRIDE study, a national longitudinal study on the health of sexual and gender minority people, showed that participants reporting any lifetime healthcare mistreatment had greater odds of past-year healthcare avoidance due to anticipated mistreatment among gender expansive, transfeminine, and transmasculine people. Reference Clark, Luong and Lunn19 For the sexual and gender minority patients with cardiovascular disease, delayed presentation leads to delayed beneficial therapies leading to poorer outcomes. It is possible that concordance between sexual and gender minority patients and physicians may improve the quality of care through improved levels of trust and patient satisfaction, enhanced cultural competency, and expanding minority patients’ access to health services. Today, the term “diverse” workforce should now be expanded to include sexual and gender minorities. Thus, institutions need to make efforts to recruit and retain LGBTQ+ cardiologists to reduce disparities in cardiology for sexual and gender minority patients with both acquired and congenital heart disease. This may ultimately provide an opportunity for increased LGBTQ+ visibility in cardiology and an increased ability to effectively mentor LGBTQ+ trainees in the future.
Interestingly, the multiple regression model of the importance of SOGI discussion and impact upon specific healthcare needs revealed that adjusted for education and complexity, participants in Indiana and Texas were more likely to agree than those in Massachusetts and California. Currently, there are a record-breaking number of anti-LGBTQ+ bills and policies passed in the United States this year including both Indiana (House Bill 1608: censors LGBTQ+ kids in schools and outs transgender students) and Texas (Senate Bill 14: bans gender-affirming care for transgender youth). One reason as to why ACHD participants in Indiana and Texas were more likely to agree may be increased tolerance and inclusion of the LGBTQ+ community, given that the ACHD community is often also considered by patients to be a marginalized community within the field of cardiology (e.g. lack of access to specialized care and lack of representation in large clinical trials). Therefore, this community of patients can also recognize the importance of safety and protection (e.g. primary care providers and general cardiologists often lack knowledge of their condition) especially in regions of the country where the LGBTQ+ community is targeted based on sexuality and gender.
Next, higher education also contributed to the agreement between SOGI discussion and healthcare needs for LGBTQ+ patients. This suggests that a higher patient education level (bachelor’s degree or more) is expressive of increased participant awareness or exposure to disparities in sexual and reproductive health care by LGBTQ+ patients. Similar findings have been described in previous studies where 55% of respondents agreed that sexual orientation in the EMR was important for their provider to know, but the lack of response was attributed to patient education. Reference Rosser, Polter and Chandiramani14 Today, trainees of all levels are poorly prepared to address sexual and gender minority health when it applies to terminology, health disparities, and preventive care issues affecting LGBTQ+ patients. Reference Streed, Hedian, Bertram and Sisson20 Consequently, this highlights the importance of educating the medical community, especially the cardiology community, about the unique needs of sexual and gender minorities. This includes not only a basic understanding of sexual and gender minority diversity but also providing a safe and welcoming environment for patients to receive cardiovascular care. Improvements in physician training on the clinical cardiovascular care of LGBTQ+ patients with acquired or congenital heart disease may lead to better awareness of healthcare disparities in the LGBTQ+ community and therefore to improved outcomes for these patients.
The lack of SOGI data collection in cardiovascular medicine, specifically among ACHD centres with a large volume of LGBTQ+ patients, will continue to create disparities among sexual and gender minority patients. Reference Deb, Porter, van Cleef, Reardon and Cook21 Similar to other stigmatized populations (e.g. racial and ethnic minorities), it is now described that stress exposure related to discrimination and stigma related to gender minority can lead to unhealthy coping behaviours and arouse psychological stress reactions that negatively affect the health of stigmatized people. Reference Panza, Puhl, Taylor, Zaleski, Livingston and Pescatello22 However, given the lack of cardiovascular research in LGBTQ+ adults with CHD, there is now a critical area for future work. Cardiology/ACHD fellowship programme directors should consider incorporating LGBTQ+ content into fellowship curricula to better understand and reduce cardiovascular disparities in marginalized populations such as sexual and gender minorities.
Impact on cardiovascular research
This study provides a detailed assessment for the evaluation of SOGI in cardiovascular research. Sex and gender are not mutually exclusive. Yet, in cardiovascular clinical research, these terms are often used interchangeably. Prior to initiating a study, the clinical researcher should ask the following questions: (1) Should the sex or gender of the study participants be reported? and (2) What is the correct term for designating male/female versus men/women? Reference Clayton and Tannebaum23 Clinical investigators should therefore use the terms male and female only when describing the sex of human subjects when sex is reflected by the gonads, external genitalia, and internal reproductive organs. Alternatively, gender comprises the social, environmental, cultural, and behavioural factors and choices that influence a person’s self-identity and health. Reference Heidari, Babor, DeCastro, Tort and Curno24 Importantly, this study demonstrated the importance of incorporating two-step gender identity questions as well as questions regarding SOGI as standard measures in cardiovascular research. These SOGI questions when tested in this tertiary care setting provided additional information on LGBTQ+ patients with CHD but may also be applicable for adults with acquired cardiovascular disease.
Research continues to demonstrate that diversity among the cardiovascular workforce including race, ethnicity, gender, nationality, religious affiliation, and socio-economic background drives innovation and performance. Reference Helwett, Marshall and Sherbin25,Reference Chapman, Thomas and Tan26 Importantly, as a result of our work demonstrating a large number of patients who identify as LGBTQ+, the definition of diversification of the workforce should now be expanded to include SOGI. A diverse research cardiovascular research workforce is essential to identify cardiovascular issues unique to not only ACHD patients but also those who are currently underserved by the healthcare system (e.g. LGBTQ+).
Study limitations
There are several limitations when interpreting the results of this study. First, the results of this study were obtained from large, academic ACHD centres. Therefore, the results may not be generalizable to other areas of the country or other populations of patients (e.g. patients with acquired heart disease). To facilitate this study, we kept the number of questions in the survey to a minimum, thereby decreasing the stress and overall burden on patients participating in a research study while attending ACHD clinics. Importantly, we were not able to collect data on patients who did not choose to participate in this study or their reasons for declining to participate as this would still require consent to participate consistent with Institutional Review Board (IRB) approval. Furthermore, many LGBTQ+ patients still have concerns about confidentiality with regard to research about their SOGI data and how this information will be used. Therefore, some patients may have chosen not to disclose their identity due to fear and/or stigma from prior experiences in the healthcare setting. Reference Rossman, Salamanca and Macapagal27 Conversely, many of the physicians conducting this study and consenting for participation publicly identify as LGBTQ+ or allies to that community and often wear symbols of inclusion such as rainbow badge holders. While anonymity in survey participation was assured, patients may have progressively answered questions given the environment and situation in which the survey was administered. Future studies may include the development of therapeutic interventions for risk reduction for LGBTQ+ adults with acquired and congenital heart disease. Additionally, this study demonstrates the need for other research opportunities to expand educational and public health efforts to understand and reduce disparities in cardiovascular health among LGBTQ+ adults.
This study supports the need for integrating SOGI questions for patients with CHD, as well as other types of cardiovascular disease. In this largely heterosexual population, ACHD patients demonstrate comfort and acceptability with responding to SOGI questions. Collecting SOGI information is the first step towards reducing cardiovascular health disparities in LGBTQ+ adults with CHD.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951124025344.
Acknowledgements
The authors would like to acknowledge Jeannette Lin, MD, at Ahmanson/UCLA Adult Congenital Heart Disease Center.
Financial support
None.
Competing interests
None.








