Assaults on medical staff have recently been the focus of national media attention. One survey of UK accident and emergency departments (Reference Wyatt and WattWyatt & Watt, 1995) reported that 96% of junior doctors had suffered verbal abuse, 32% had been subjected to attempted assault and 18% had actually been physically assaulted in their workplace.
Concern for the safety of mental health professionals had also intensified. One study of junior psychiatric doctors found that 25% had been physically assaulted once during their work, and that 8.3% had been attacked twice (Reference Kidd and StarkKidd & Stark, 1992). More recent work has suggested that the figure may be higher, with 37% of trainee psychiatrists having sustained a physical attack (Reference ChubbChubb, 1997).
Staff need protection from these violent incidents, and there are a number of possible factors to address. Training in breakaway techniques is important and educational packages to assist staff in reducing aggression may also be of value (Reference Shah and DeShah & De, 1998). The impact of the clinical environment and its contribution to violent incidents should not be overlooked. The Royal College of Psychiatrists (1998) has made recommendations regarding the relationship between the clinical environment and violent incidents. They emphasise that the likelihood of violence will be reduced if wards are clean, calming, comfortable areas with natural daylight and fresh air. In addressing safety design of interview rooms they suggest several features. Interview rooms should have easily accessible, functioning alarm systems and clear unobstructed exit paths. Attention should be paid to door locks. Should an attack occur, it is important that other staff can enter the room quickly, and locks that could prevent this should be avoided. Rooms should be located close to other staff members in case of emergency, and should not contain objects that could be used as weapons or missiles.
Davies (Reference Davies, Howells and Hollin1989) suggested similar specifications for clinical interview rooms, but made a number of additional recommendations. In particular, the room used should be a designated interview room, rather than having a dual function such as office or storage area. The dual function of such rooms usually compromises their safety features, often by obstructing exits or providing objects that could be used in an attack. Interview rooms should have an unblocked viewing window to allow observation by other staff. A furniture plan for interview rooms that minimises the risk of violence is reproduced in Fig. 1.
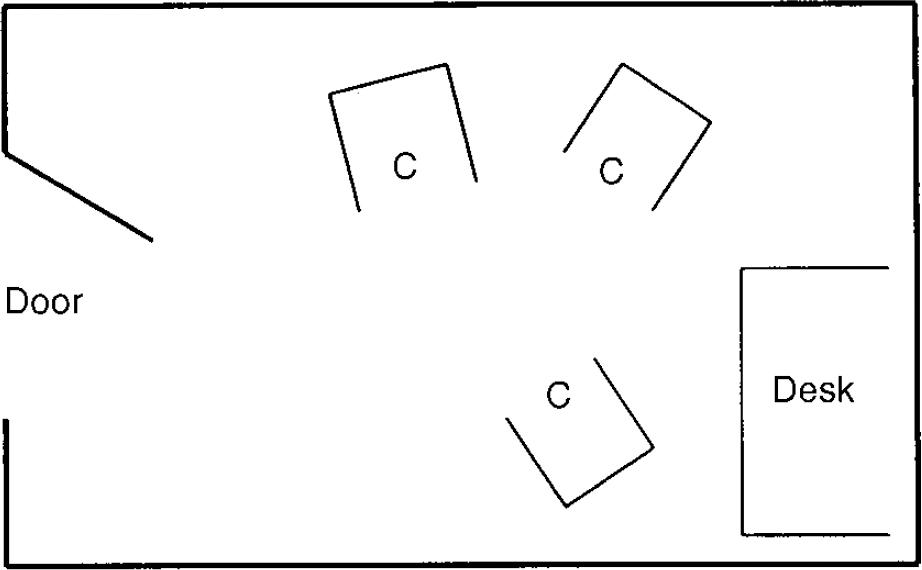
Fig. 1 Suggested furniture layout to maximise safety in interview rooms, adapted from Davies (Reference Davies, Howells and Hollin1989). C, chair
This audit project was prompted by an assault on a junior doctor, in which unsafe room features were felt to have contributed. Interview room safety is a suitable focus for clinical audit: the subject is directly relevant to clinicians, and objective data can be readily collected.
Method
An initial assessment was undertaken to determine safety features of the interview rooms in hospital and community settings, including the presence and accessibility of panic alarms and a clear exit path from the room. Results were presented at a multi- disciplinary audit meeting and future standards were discussed and agreed. Twelve standards were derived from the literature (Royal College of Psychiatrists, 1998; Reference Davies, Howells and HollinDavies, 1989) and are shown in Table 1. These standards were disseminated throughout the department and subsequently used for a more comprehensive assessment of all interview rooms in the psychiatric department, including out-patient, in-patient and day patient facilities. Results were presented to the general audit meeting and separately to the managers responsible for each area. Individual recommendations for each room were made available. At 12 months from the pilot survey changes in room safety features were reassessed against the same standards, closing the audit loop for a second time. Differences in safety features at 6 months (T1) and 12 months (T2) were compared using the Chi-square statistic. Results were further scrutinised by limiting the data to those rooms that were being used for interviews at both T1 and T2. These paired data were analysed using the McNemar test.
Table 1. Number(%) of rooms meeting agreed safety standard at pilot assessment (T0), and reaudit at 6 (T1) and 12 months (T2) after agreement of standards
| Number (%) of rooms meeting standard at | ||||
|---|---|---|---|---|
| Room feature | T0 (n=27) | T1 (n=46) | T2 (n=50) | Significance level |
| Alarm present | 26 (96) | 41 (89) | 46 (92) | NS |
| If present, alarm accessible | 14 (54) | 27 (66) | 38 (83) | NS |
| Clear exit path to door | 11 (41) | 32 (70) | 23 (46) | χ2=5.44, P=0.02 |
| Room not isolated | — | 21 (46) | 33 (66) | NS |
| Viewing window in door | — | 23 (50) | 24 (48) | NS |
| Safe lock (see text) | — | 6 (13) | 16 (32) | χ2=4.87, P=0.03 |
| No objects to use as weapons in an attack | — | 17 (37) | 9 (18) | χ2=4.36, P=0.04 |
| Room layout resembles Fig. 1 | — | 8 (17) | 8 (16) | NS |
| Furniture suitable for conducting interviews | — | 17 (37) | 9 (18) | χ2=4.36, P=0.04 |
| Room has natural light | — | 25 (54) | 31 (62) | NS |
| Room is clean | — | 41 (89) | 39 (78) | NS |
| Décor satisfactory standard | — | 31 (67) | 24 (48) | NS |
Results
Twenty-seven rooms were assessed in the pilot survey (T0). The number of rooms with unsafe features generated concern, and the more comprehensive audit was commissioned. Six months later, at the time of this first comprehensive assessment (T1), 46 rooms were being used for interviewing within the department. Twelve months later (T2), when accepted standards were reaudited, 50 rooms were being used for this purpose. Safety features of the rooms at all three assessments are also shown in Table 1.
Only one room contained all of the 12 safety features at each assessment point and could therefore be considered a safe environment in which to interview patients. At 12 months significantly fewer rooms had clear exit paths (P=0.02) and significantly more rooms contained potential weapons (P=0.04). In contrast, more door locks were now of a safe design (P=0.03). Other measures had not changed significantly. There were still rooms without panic alarms and just over half the rooms had doors without viewing panels. Only 16% had furniture arranged to resemble the suggested safer room plan. When the analysis was restricted to those rooms in use for interviews at both T1 and T2, 44 rooms were eligible for inclusion. This analysis showed no significant changes, apart from an increase in the number of objects available for use as weapons (P=0.03).
Comments
The pilot survey revealed that safety was markedly compromised in the rooms in which people interviewed patients. Our audit resulted in a lack of positive substantial change from the first comprehensive assessment (T1) to the reaudit (T2). This was disappointing and concerning. Subjectively we felt that the staff working in the units and their managers were greatly concerned about safety after both the pilot assessment and the first comprehensive audit. Unfortunately, this concern did not translate into positive change.
There are a number of possible explanations for these results. Issues relating to finance, staff apathy, management and the process of clinical audit itself may all have contributed, and we recognise that our method had some limitations.
One limitation of the study methodology is the subjective nature of some of the measures, such as décor and cleanliness. Although the same two assessors were used at each stage, this could be a source of bias. In addition, the audit was clinically driven, so all the rooms currently in use for clinical interviews were included at each assessment. This meant that different rooms were included at T1 and T2. However, the analysis of paired data for the rooms that were assessed at both T1 and T2 did not support this explanation.
Some changes may have been limited by financial constraints. The installation of alarm systems, improvement of décor and door lock replacement can all be costly. However, finance cannot explain all the results, since there was little improvement in recommendations without major financial implications, such as furniture layout. Financial concern is also no excuse for compromising staff safety.
In an established unit, some physical changes are also difficult to address. This is particularly true of the requirement for rooms to benefit from natural light. Although room function can be manipulated, so that rooms with natural light are used for clinical purposes, this is not always possible.
An alternative explanation for the lack of change might be a variation in the level of interest in safety issues over time. After the original assault in our unit and presentation of the audit results, concern seemed genuine. Between T0 and T1 there was a significant improvement in the number of interview rooms containing clear escape paths (P=0.02). However, between T1 and T2 there was a subsequent significant deterioration in this safety feature (P=0.02). As time passed without further incident, concern for safety seemed to wane, so that other changes to rooms did not occur. Over time, staff allowed interview rooms to become significantly more cluttered with unnecessary objects and furniture. Although significantly more interview rooms possessed door locks with adequate safety features, a majority (68%) still had unacceptable locks. The change in locks was actually owing to reallocation of rooms used for interviews, rather than the replacement of unsuitable locks, since analysis of the paired data did not suggest any change in lock safety in the rooms assessed at both time points.
Perhaps it is difficult for staff to remain vigilant regarding safety without frequent reminders. It may also be psychologically more comfortable to forget safety issues, rather than to constantly worry about being attacked during the working day.
Some blame for our disappointing results may lie with the process of audit itself. A current national project is examining the reasons why audit may fail, and preliminary discussion has suggested that one factor could be a mismatch between the priorities of management and clinicians (Berger, Reference Berger1998a ,Reference Berger b ). Managers may allocate less priority than clinicians to issues of staff safety. This is clearly unacceptable, and we believe that clinicians should ensure that staff safety is pushed to the top of the management agenda. Another criticism is that the process of audit sometimes functions only as an assessment exercise. As a consequence, projects with worthwhile aims can simply result in “reports that end up in a drawer” (Reference BergerBerger, 1998c ). Unless clear action plans are formulated during the audit process and individuals are identified to oversee this action, changes are unlikely to be forthcoming.
We believe that the safety features of interview rooms are an important subject for audit. Future audit design should incorporate an active limb, with a clear line of individual responsibility for implementing recommendations. Staff safety should be a major priority for managers, and clinical staff should be encouraged to remain permanently vigilant regarding their own clinical environment when interviewing patients or relatives.
Acknowledgements
We are grateful to Lorna Squires and Keith Russell, The Royal Free Hospital, for help with data collection.





eLetters
No eLetters have been published for this article.