Neurodevelopment and neurodevelopmental disorders (NDDs) are increasingly recognised as being important within mainstream psychiatry. ICD-11,1 for example, places neurodevelopment centrally within psychiatric taxonomy. Although NDDs incorporate many conditions, attention-deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are currently prominent. National strategies and adult clinical guidelines for both have significant implications for adult mental health services (AMHs).
ADHD and ASD are important for non-intellectual disability AMHs because they are risk factors for common mental disorders and are over-represented in the patient population of AMHs. On average, adults with ADHD experience three co-occurring disorders, with around 70% of individuals eventually diagnosed with ASD or ADHD having first presented with co-occurring psychiatric disorders.Reference Gillberg2
Identifying ASD/ADHD in daily practice is important. Irrespective of whether aetiologically related or co-occurring, recognising that a person with depression is also autistic for example, can change how the person and their psychopathology are understood, and help the clinician provide more appropriate help. Not recognising ASD/ADHD increases the risks of misunderstanding, misdiagnosis, suboptimal help and potentially poorer outcomes. Unfortunately, individuals who are autistic or have ADHD are frequently negative about AMHs, saying they are not understood or taken seriously, suggesting many clinicians have patchy knowledge and experience about how best to help.
Although this may be because NDDs are relatively new for mainstream AMHs, it is more likely because NDDs fit uncomfortably with the usual paradigms used in AMH for diagnosis, management and service design. Additionally, the specific terms used within this field appear to represent contradictory ideas. Consequently, professionals and public may vary in what ‘neurodevelopmental’ and related terms mean and may not agree about the appropriate role and remit of mental health services, leading to unhelpful divisions.
We aim to provide definitions incorporating established evidence and harmonising apparently discordant perspectives emerging from ADHD/ASD. This may help clinicians better understand NDDs, help improve communication with individuals with recognised or unrecognised ASD/ADHD and help incorporate neurodevelopment into daily clinical practice. Agreed definitions such as these are also fundamental in developing effective co-constructed clinical pathways for individuals with ASD/ADHD and potentially NDDs in general.
The medical perspective – NDDs
Like most medical services, AMHs are comfortable with and designed around those who have episodic disorders i.e. a disadvantageous change in a person's normal state. Diagnosis describes a characteristic pattern of change, with interventions primarily aimed at restoring the person's to their normal state.
AMHs are less comfortable with trait conditions such as personality disorders, where there is no change in an individual's normality. Here, diagnosis is defined as being extreme normal traits causing significant functional impairment. Importantly, this implies that extreme traits are not invariably impairing, unlike episodic disorders. Further, although diagnostic labelling does serve to help understanding, the primary therapeutic aim is not usually to change the person's normality, but rather to advise on environmental adaptations.
The points relating to trait disorders also apply to ASD/ADHD (and potentially NDDs in general). Both DSM-5 and ICD-11 concur that these describe lifelong traits, which variably present in the population with no separation between normality and diagnosis. Diagnosis is defined when traits ‘outside the limits of normal variation’1 cause significant functional impairment. Although normal variation is not determined, research suggests that whereas there are a small number of individuals whose symptoms are so extreme as to be clearly outside normal variation (usually related to specific pathologies such as fragile-X syndrome), the majority have traits that lie at one end of, but probably within, the population's normal variation and do not have a specific aetiology. Both taxonomies therefore confer diagnosis to two groups within ASD and ADHD – the larger group who are at the extreme end of normal variation in neurocognitive function and are significantly impaired, and a smaller group who fall outside normal variation who have a specific aetiology causing severe impairment. Those who have extreme traits but are not functionally impaired do not have a diagnosis.
Neurodiversity and related terms
‘Neurodiversity’ was first coined in 1998 by Judy Singer, sociologist, and an autistic person who wrote that autistic people were a category similar to class/gender/race.Reference Singer3 This has led to the development of a number of specific terms, namely neurodiversity, neurodiverse, neurodivergent and neurotypical, which describe subsets of the normal population demarcated by the limits of current societal norms. Singer situates her arguments in the social model of disability with an explicitly political dimension, which has sprouted a civil rights ‘neurodiversity movement’. The implication is that autistic people, and by extension, all those who are neurodivergent or different on other neurocognitive dimensions are not disordered, but rather part of normal variation. Here, societal norms may disadvantage the individual, the ‘interventions’ being for society to better understand and provide an appropriate environment for the neurodivergent. This viewpoint rejects the notion of ‘normal’ or ‘healthy’ brains, or a ‘right’ style of cognition,Reference Walker4 questioning if NDDs should be seen as mental disorders, particularly as these traits can be advantageous in some situations – a view supported by data. It also implies two groups of neurodivergent individuals – those who have resultant disadvantage, and those who do not.
The National Autism Implementation Team model and definitions
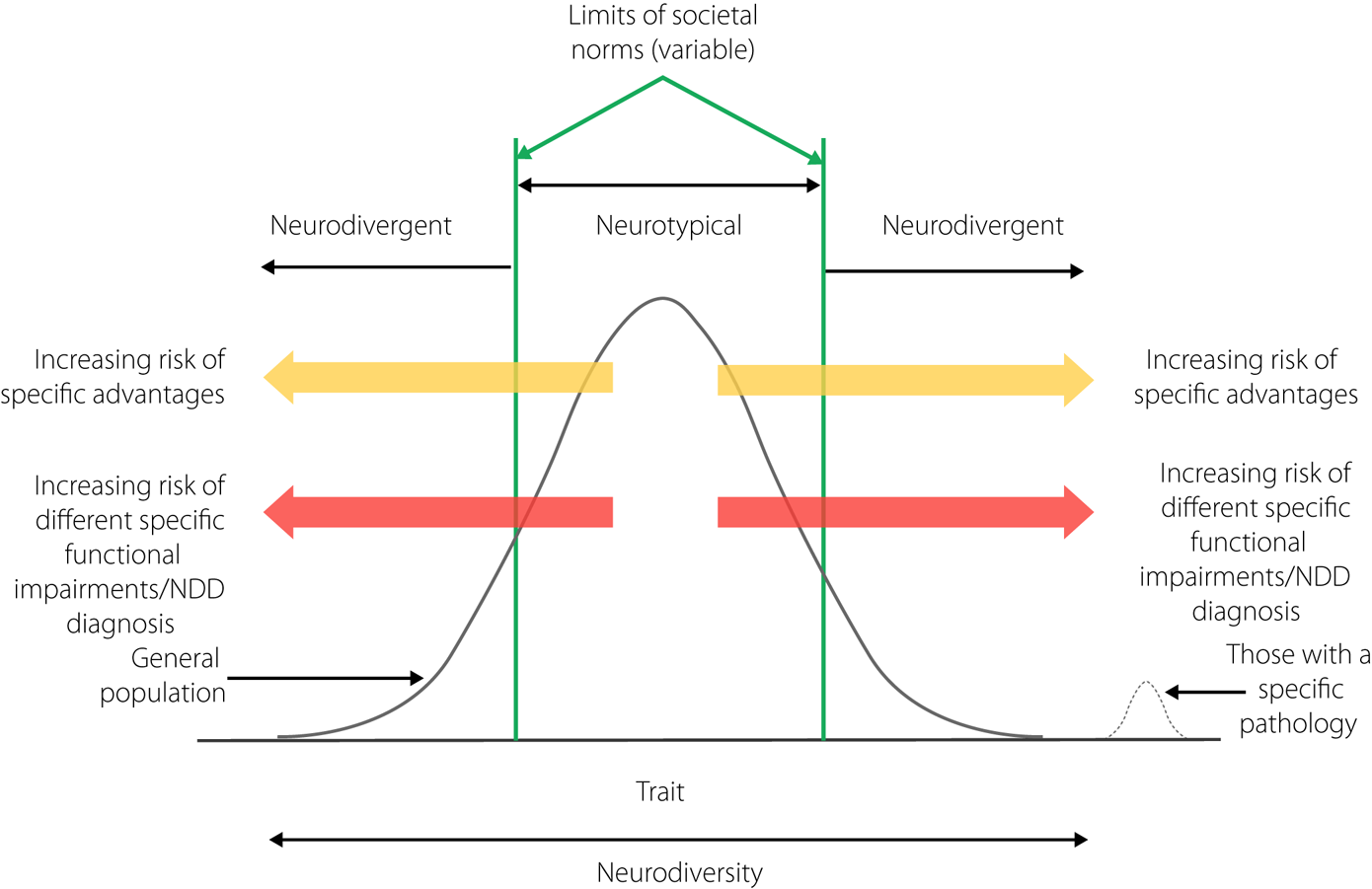
Our aim is to provide a descriptive model incorporating the different viewpoints without regarding one as more valid than any other (schematically illustrated in Figure 1). The following definitions are a development of a previous model,Reference Shah and Morton5 integrating scientific evidence and views from people with lived experience, from experts, practitioners and prominent thinkers on neurodiversity.Reference Singer3,Reference Walker4
(a) Neurocognitive functions are selective aspects of brain functions – for example regulating, learning, attention, emotions, impulses, sensory processing and social behaviours. These are traits present from birth, may be significantly genetically influenced, the normal range dependant on age.
(b) Neurodevelopment is the process of change of these selective brain functions with age.
(c) Neurodiversity is the statistical normal range of function in a population at a particular age. Neurodiversity is a characteristic of the whole population, not a specific individual.
(d) The societal norms for selective neurocognitive functions is the range that society regards as being normal for a given age – these may be narrow, variable, arbitrary and influenced by context and culture.
(e) Neurotypical describes individuals whose selective neurocognitive functions fall within prevalent societal norms.
(f) Neurodivergent describes individuals whose selective neurocognitive functions/ neurodevelopmental differences fall outside prevalent societal norms. They do not necessarily have a neurodevelopmental disorder.
(g) A neurodevelopmental disorder or condition is a term reserved for those whose neurocognitive function lies at an extreme for a given age with associated significant functional impairment.
(h) The risk of functional impairment increases as the neurocognitive function becomes more extreme, and if the environment becomes increasingly unsupportive.
(i) Neurodevelopmental differences describe various neurotypes without labelling these as disordered, divergent or functionally impaired.
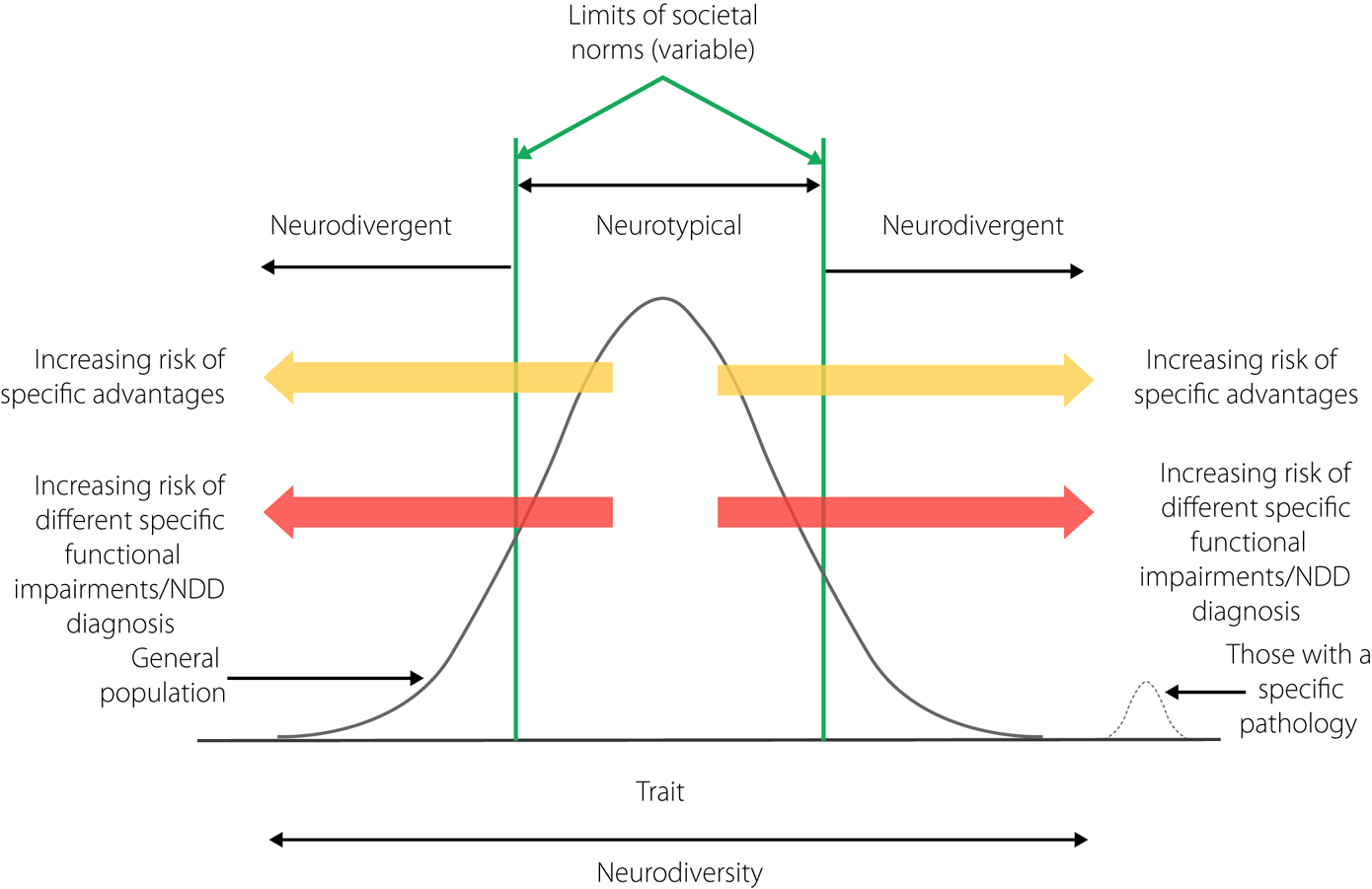
Fig. 1 The National Autism Implementation Team model illustrates the relationship between a neurocognitive function, the terms neurodiversity, neurotypical and neurodivergent. We assume the neurocognitive function is normally distributed in the population and societal norms are centred around the population norm. The green bounds represent societal norms. We describe the situation for the right side of the distribution, but it is equally applicable to the left side. The more the person is divergent, the greater the risk of impairment. However, not all who are divergent experience impairment/have a diagnosis. NDD, neurodevelopmental disorder.
The different viewpoints agree at many important points. All perspectives recognise that there is normal variation in development that forms the basis for neurodiversity/neurodevelopmental differences, that most people described as having ASD or ADHD are individuals at one end of normal variation and all perspectives express discomfort about ASD/ADHD being regarded as a disorder. All recognise the primacy of environmental adjustments, not ‘treating to normalise’, notwithstanding ADHD medications. The medical viewpoint also accounts for a group of individuals whose symptoms are a result of a specific pathologies (for example fragile-X syndrome) clearly outside the normal range.
There is, however, a significant point of disagreement. Both DSM-5 and ICD-11 criteria require significant impairment for a diagnosis, whereas from other viewpoints the label is useful as an identity and differences are not seen as deficits. This is reflected in language use – some in the autism community state that identity-first terms should be used (such as ‘autistic person’), moving away from the idea that autism is a disorder. Others in the community however, prefer ‘person-first’ terminology (such as ‘a person with autism’). As this debate is currently unresolved, we use both forms interchangeably, recognising varying individual preferences.
This disagreement indicates that those with observable traits but who are not considered impaired find labels such as autism useful and meaningful, suggesting the continuing need to evaluate the concept of autism, and explore the role of impairment and neurodevelopmental differences in diagnosis. Understanding impairment and difference more fully may open up possibilities for preventative/early interventions. Individuals may ‘mask’ their differences and potentially experience resulting impairment if society does not accept, tolerate or understand neuro-differences. A lack of understanding or validation may also limit access to supports again increasing potential impairment. Helping society to accommodate differences and reduce barriers to participation could be useful early or preventative strategies for reducing impairment in neurodivergent individuals.
Author contributions
The first draft was written by P.S. The other authors confirm that they meet ICMJE criteria. All authors contributed to review and commented on the document.
Funding
This work was supported through funding from the Scottish Government.
Declaration of interest
P.S. has received payments from Takeda for providing continuing professional development sessions on neurodevelopmental disorders. All other authors declare no conflicts of interest.




eLetters
No eLetters have been published for this article.