To the Editor—An immunocompromised hospital inpatient with Norwegian (crusted) scabies went undiagnosed for 6 weeks without isolation or treatment. A literature review revealed little guidance on the logistics of providing mass prophylaxis to exposed individuals. We used a hospital-based incident command system to establish a mass prophylaxis clinic.
A patient with a history of gynecological malignancy undergoing chemotherapy was admitted to a 33-bed hematology-oncology, bone marrow transplant unit at our academic medical center in northern New England. The patient had skin plaques and rash of unknown etiology, which went undiagnosed for 43 days due to the absence of pain or itching. Dermatology was consulted, and an exam revealed diffuse crusted hyperkeratotic scaly macules and papules including plaques in the webbing of the fingers. Skin scraping with mineral oil preparation revealed at least 5 scabies mites. The patient was diagnosed with crusted scabies, placed on contact precautions, and treated with oral ivermectin and topical permethrin.
Upon notification, the infection prevention (IP) program reviewed guidance from the Centers for Disease Control and Prevention and additional literature to assess recommendations for providing prophylaxis in the setting of a prolonged period of undiagnosed crusted scabies in a healthcare facility. Modified institution-wide prophylaxis for patients, staff, visitors, and household contacts was deemed necessary to prevent an outbreak of scabies within the facility. The literature lacked guidance on operationalization of a large-scale intervention. The hospital incident command system was activated to assist in establishing methods for notifying staff, patients, and visitors of their exposure and to manage the logistics of providing prophylaxis to a large number of people over a short period of time.
The hospital incident command system is activated in situations in which a large number of people may be affected. Past activations included network outages and contamination of the city water supply. Notifications are sent via a paging system and by telephone to members of the incident command team alerting them of the activation. A dedicated conference room is used as a meeting space and a dedicated phone line is established for conference calling. Those responding to the activation include hospital administrators, subject-matter experts, public information officers, and emergency management (EM) staff. Because this incident involved patients, staff, and visitors in inpatient and ancillary areas, more team members were utilized than in a typical activation.
The incident command team met 3 times daily, and smaller subcommittees met throughout the day to discuss physical setup, location, staffing and dates of the clinic, acquisition of medication, and communication with those exposed. A walk-in clinic was deemed the most efficient way to provide prophylaxis to those exposed. Based on availability and ease of dosing, topical permethrin was selected as prophylaxis.
Staff who had the closest contact with the index patient, as determined by a review of the medical record, were notified by email of their exposure and the need to acquire prophylaxis for themselves and their household members. Dates, times, and locations of the clinics were included in this communication. A review of the affected unit’s census was performed to identify patients who were admitted to the affected unit during the specified period, and a letter was sent to those discharged notifying them of their possible exposure and providing information for attending the clinics. For those who had passed away since their admission, families were notified by a phone call from the nursing director and prophylaxis was offered to the household members. Patients currently on the affected unit at the time of the outbreak were notified by their attending physician and were prescribed permethrin or ivermectin as prophylaxis. A public announcement was made in the local newspaper, television, and radio stations to alert members of the public who may have visited the affected unit during the exposure period. An information hotline was set up through the department of health for anyone with questions about scabies or the clinics. The department of health, in collaboration with the IP program, released a Health Alert Network (HAN) communication regarding the exposure, and a website was created with contact information and frequently asked questions.
Two adjoining conference rooms were used as clinic space. Figure 1 illustrates the set up and flow of the clinics. Everyone who presented to the clinic was screened using a paper screening tool. All who indicated being on the affected unit during the exposure period or who were a household member of someone who was, were offered prophylaxis. A cohort order was written by the medical director of EM, and a nurse protocol was used to place the order for those needing prophylaxis. The order allowed for heads of households to obtain medication for those living with them. All patients were assessed for allergies or contraindications to permethrin cream before it was given, and heads of household were responsible for reporting allergies and contraindications of those who were not present.
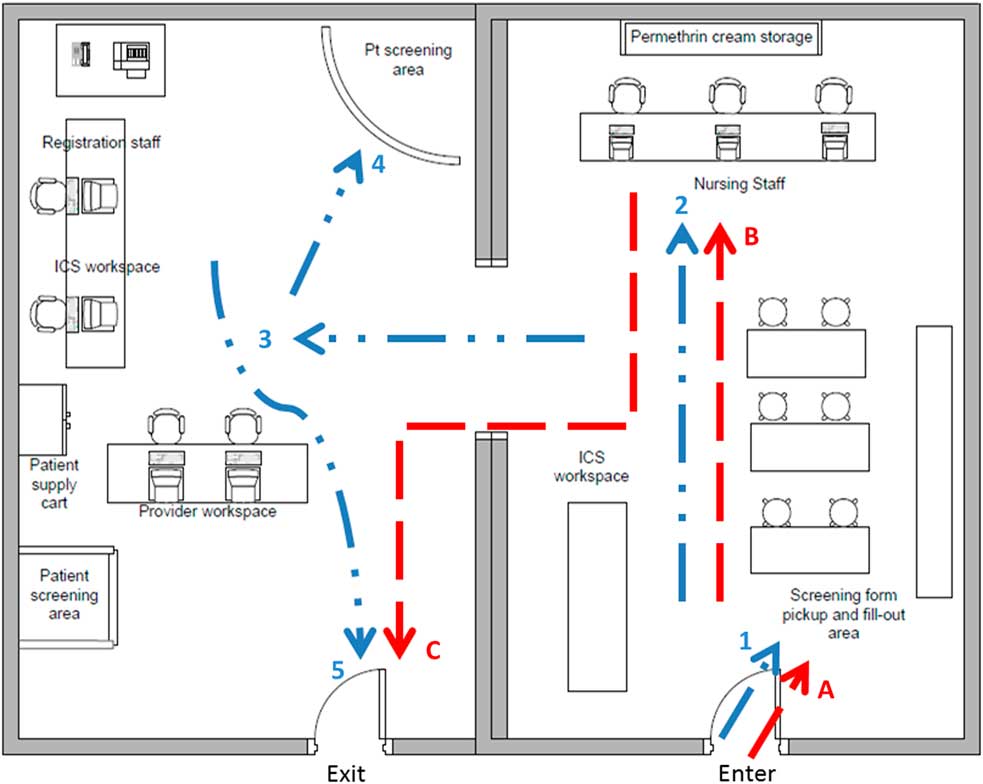
Fig. 1 Mass prophylaxis clinic set up. The dashed line (A–C) presents patient flow of a patient not needing provider examination. The dotted line (1–5) represents patient flow of a patient needing a provider examination.
Adjacent to the screening, a prescribing and dispensing area was established for patient examination. Privacy screens were used to create examination areas, and personal protective equipment, patient gowns, and linens were provided. Physicians staffed the clinic to assess patients who were concerned that they might have scabies. Supplies for skin scrapings and slide preparation were available, and a lab technician was on-call to collect specimens for processing.
More than 1,000 doses of permethrin were distributed during the clinics. There was 1 confirmed case of scabies and 3 probable cases of secondary transmission as a result of this outbreak.
Establishing a centrally located clinic using the incident command system structure provided rapid and effective screening and prophylactic treatment of scabies to prevent a larger outbreak of scabies within the institution.
Acknowledgments
None.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.



