Introduction
Quarantine is the restriction of movement of individuals who are not ill, but who may have been exposed to an infectious illness, in order to prevent transmission of a disease.1 This practice is controversial as it involves persons who are not sick and who may not develop illness. The length of quarantine is based on the incubation period of the illness. Isolation, on the other hand, is a well-accepted practice, as it involves the containment of ill and symptomatic patients to prevent spread of disease to those around them, and is based on the duration of communicability.
The practice of quarantine dates back as early as the 14th century, where it was used to control plague in Italy. Ships arriving from infected ports in Venice were required to anchor for forty days before landing.2 The practice of quarantine had fallen out of favor over the last 50 years because it was considered socially unacceptable and inhumane to imprison a healthy individual. The advent of vaccines and antimicrobials also provided governing bodies alternatives to containing the spread of infectious agents. Recent events have sparked renewed interest in quarantine including the increased fear of bioterrorism after 9/11, the 2003 SARS outbreak and, most recently, the fear of pandemic H1N1 influenza.
As a result of such events, a quarantine system was developed to limit the introduction into and spread of infectious diseases in the US. The quarantine system is made up of USA quarantine stations located at 20 ports of entry and land-border crossings where international travelers arrive. Medical and public health officers employed by the US Centers for Disease Control and Prevention (CDC) work together at these stations to respond to reports of illness, screen cargo, inspect animal products and collect medical information from new immigrants, refugees, and asylum and parole seekers wishing to enter USA.3 During an infectious disease emergency, these quarantine stations will have to team with local public health departments and provide strategic leadership.4
Quarantine is used to contain and restrict well individuals who may have been exposed to an infectious illness in order to monitor them for signs and symptoms of the infection for a period of one incubation period. Certain exposures such as illness on an airplane with foreign travelers, a bioterrorist attack at a small venue, or exposure to an unknown agent where close observation of exposed individuals is needed to learn about the infection may require quarantine in a designated hospital unit. Quarantine is not a routine hospital procedure and therefore even those health care centers specifically designated for this task may find themselves poorly prepared to handle such a situation. There are few studies in the literature that examine the preparedness of these designated hospital units.
In the event of an outbreak of a communicable respiratory illness, quarantine may become necessary. The New York Institute for All Hazard Preparedness (NYIAHP) of the State University of New York (SUNY) Downstate Medical Center, in cooperation with the New York City Department of Health and Mental Hygiene's Healthcare Emergency Preparedness Program (NYC DOHMH-HEPP) quarantine working group, developed an Adaptable Quarantine Manual containing a series of clinical protocols and worksheets designed to aid health care facilities responding to such an event.
Two full-scale exercises (FSEs) were designed based on the protocols in the Adaptable Quarantine Manual; this manual can be found on the Hospital intranet and is available for all staff; it was not published on the New York City Department of Health and Mental Hygiene's internet for public access. The FSEs were conducted to test a designated quarantine unit's ability to follow protocols within the manual and effectively receive and house patients. The exercises also aimed at increasing the readiness of Kings County Hospital Center (KCHC), a Brooklyn hospital with designated quarantine space, to respond to a severe infectious respiratory disease exposure in the community. The purpose of this study is to describe the lessons learned from each FSE, and to compare the level of preparedness during the initial exercise with that of the second exercise conducted a year later.
Methods
Study Setting
Both FSEs were conducted in the Quarantine Unit at Kings County Hospital Center (KCHC) in Brooklyn, New York. Kings County Hospital Center is a tertiary care hospital with a level 1 trauma center and 627 hospital beds. The hospital serves approximately 2.6 million residents from Brooklyn and Staten Island. The unit was renovated in 2006 specifically as an isolation unit, and then identified as a quarantine space. It has not been in operation since completion in June 2006. The unit can house 26 patients; all of the rooms have negative pressure capability and an anteroom.
Drill Description
The first FSE was on April 23, 2009 and the second on April 22, 2010. The background scenario of the exercise involves the detection of an individual suspected to have Severe Acute Respiratory Syndrome associated coronavirus infection (SARS-coV) on a private jet in eastern US airspace, returning from Hong Kong. All other passengers on this flight are asymptomatic. The CDC Division of Global Migration and Quarantine employees at John F. Kennedy International Airport, New York, and the New York City Department of Health and Mental Hygiene deem it necessary to quarantine the asymptomatic passengers due to the exposure. Prior to this event, KCHC received numerous mock health alerts detailing the identification of a novel and highly pathogenic strain of corona virus in Southern China with pandemic potential.
There were a total of 15 passengers on the flight. The exercise involved ten different quarantine scenarios as follows:
1. An Orthodox Jewish family with specific religious requests;
2. A single mother and her child with behavioral problems;
3. An unaccompanied minor;
4. A smoker requesting to smoke cigarettes on the unit;
5. A non-English speaking man with dietary constraints;
6. A woman who develops respiratory distress while in quarantine;
7. A woman with severe anxiety;
8. A geriatric couple with many underlying medical problems;
9. A businessman requesting internet and cell phone services to conduct business; and
10. A cooperative individual.
Each scenario was used to evaluate five protocols developed by the quarantine working group: Activation of the Unit, Staffing, Charting/Admission, Symptom Monitoring and Infection Control, and Client Management. Evaluation of these protocols was based on the completion of critical tasks by staff working in the quarantine unit and in the emergency operations center (Table 1). There were two evaluators assigned to each patient scenario. Task completion was assessed by both FSE evaluators and FSE actors. The FSE actors were hired actors simulating patients.
Table 1 Activity by Critical Task in the Activation of the Quarantine Unit. The spreadsheets were developed in cooperation with the NYC DOHMH which addressed readiness of the Quarantine unit. A yes response on the evaluation forms was considered a positive response and therefore compliance with protocols and procedure were adhered to.
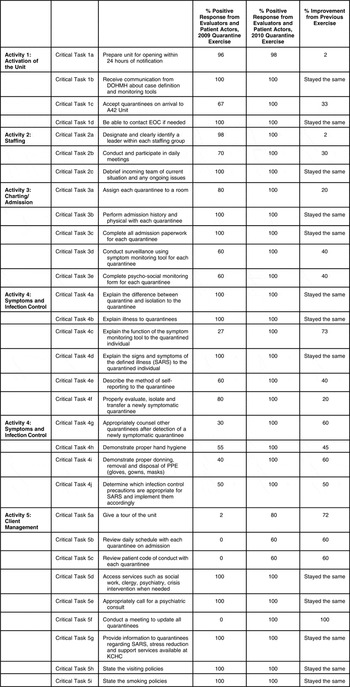
Abbreviations: DOHMH, Department of Health and Mental Hygiene; EOC, Emergency Operations Center; KCHC, Kings County Hospital Center; PPE, Personal Protective Equipment; SARS, Severe Acute Respiratory Syndrome
Evaluation and Data Collection
Drill evaluators were selected from various institutions based on their infection control and/or emergency preparedness experience. They received the evaluation materials and forms one month prior to the FSE and underwent a one-day training session on the nature of the exercise, protocols, public health recommendations and the use of the forms. Evaluation forms were created to capture critical tasks of quarantine protocols (Table 1) for each individual victim encounter in addition to observations of general preparedness of the facility. Evaluators were distributed to all critical areas and forms were designed as “easy-to-use” checklists, with the option for additional comments. The spreadsheets were developed in cooperation with the NYC DOHMH which addressed readiness of the Quarantine unit. Additional forms for Emergency Operations Center (EOC) readiness were modifications of the assessment forms produced by HHS Agency for Healthcare Research and Quality's Public Health Emergency Preparedness program. A yes response on the evaluation forms was considered a positive response, and therefore compliance with protocols and procedure were adhered to.
Actors simulating patients were selected based on experience and participation in past emergency preparedness drills or exercises. All actors but three actor/patients were medical personnel from neighboring medical facilities and were unknown to hospital staff. They were trained prior to the drill in their specific patient scenarios, as well as procedures and protocols of the unit.
All actors received a briefing one hour prior to the exercise. The briefing session included an explanation of the background scenario highlighting the definition of SARS and its symptoms, expectations for each individual patient scenario and demonstration of how to complete actor evaluation forms. Actor evaluation forms were also designed as checklists with space for additional comments. A yes response on the evaluation forms was considered a positive response and therefore compliance with protocols and procedure were adhered to. All evaluation forms were collected at the end of the FSE and results were tabulated in Microsoft Excel 2003 spreadsheets for comparison.
After Action Report
An After Action Report (AAR) with an improvement plan was prepared and reviewed with the staff at KCHC after the first exercise. The Emergency Preparedness Committee at KCHC then created a plan to implement the suggested changes. The same exercise was then repeated a year later to evaluate whether improvements had been made since the last exercise to increase preparedness for a quarantine event. A second AAR was prepared after the second FSE.
Results
Activation of the Unit
The quarantine unit was evaluated for readiness for activation one hour prior to the arrival of patients. The evaluation consisted of an inspection done by the exercise evaluators to ensure adequate supplies, equipment and staffing. The unit was also inspected for cleanliness. The nursing station, clean supply room and patient rooms were all clean and well stocked with supplies, including masks, gloves, and gowns, for both exercises. Inspection of negative pressure alarms for all rooms in both exercises revealed functioning negative pressure capacity. During the initial exercise, three rooms lacked telephone and computer capabilities. All rooms were telephone and computer ready in the subsequent exercise. In both exercises, infection control teams arrived late on the unit to post recommended CDC signage, and signs were mounted as patients were entering their rooms. The overall appearance, with exception of infection control signage of the unit, was appropriate for both FSEs.
The EOC at KCHC received notification 24 hours prior to patient arrival. In the time before the opening of the unit, the EOC accomplished the following tasks in both exercises: 1) preparation of a staffing plan and recruitment of appropriate staff for the unit; 2) placement of all pre-determined and prepared monitoring tools at the nursing station in the quarantine unit prior to the exercise; 3) clarification from NYC DOHMH of case definition and disposition of the “case on the plane;” and 4) request for aircraft manifest with client demographics and special needs.
Acceptance of quarantined patients on arrival to KCHC also improved in the second exercise. In the initial exercise, hospital police sectioned off an area of the hospital for entrance of the patients; this was done to avoid intermingling with hospital visitors or staff. Hospital staff, consisting of doctors and nurses, waited at the entrance to triage and to escort patients to the unit. A patient manifest was not kept at the entrance, and there was no monitoring as to whether all quarantined individuals had been received. The non-English speaking patient was left at the entrance during the first exercise and waited at the entrance for five minutes before the staff noted he was missing. This was remedied in the second exercise. A patient manifest was requested and made available to the hospital EOC the day prior to quarantinee arrival. The EOC, together with nursing staff, provided room assignments in advance (keeping in mind family may want to stay together, etc).
The KCHC staff provided a secure surge space near the point of entry where they conducted a preliminary triage prior to intake of clients in their respective rooms in the unit. There were several administrative staff members from the admitting office assigned to keeping track of each person as they arrived and as they were being transferred. An arrival log with the name of each client was checked off, and this list was used to confirm all individuals that were on the manifest issued from the CDC were indeed still present throughout the transfer process at the KCHC.
Staffing
All hospital employees assigned to the unit were briefed with a preparatory slide presentation that discussed quarantine events and also summarized operating procedure on the quarantine unit before being permitted to begin work. At the beginning of both FSEs the Medical Director for the unit conducted a group meeting with all unit medical staff to discuss the work plan and review the basics of the quarantine event. Neither exercise required a change of shift, therefore no debriefing of incoming unit staff was evaluated.
Unit staff in the first FSE included one clerk, two attending physicians, four resident physicians and six registered nurses (four supervisors from other hospital units and two patient care assistants). Consultant services such as Pediatrics and Psychiatry were also present as needed. Assignment of only one clerk to the unit caused delays in communication on and off the unit, patient registration and delivery of meals. The physicians assigned to the unit were available by pager but not physically present at all times which caused confusion in decision making as there was no authoritative final decision maker present at all times. In the second exercise, an additional clerk was assigned to the unit, and at least one attending physician was present on the unit at all times. These additions rectified the problems described above. Staffing group leaders did not wear clearly visible identification in the first exercise. In the second exercise staffing group leaders were more clearly identified by vests and large tags describing their titles. There was an excessive number of security staff on the unit for both exercises, which created a threatening environment for patients as was mentioned in several actor evaluation forms.
The exercise evaluators and actors noted that the unit was overstaffed in both FSEs. This was probably due to the artificiality of the exercise. In the first exercise, patient actors felt overwhelmed with the number of staff visiting them and felt there was too much activity in the corridors from increased staff numbers. In the second exercise, a more organized approach to patient interactions was developed, in which medical staff would enter the room together. History and physical examinations were done in a coordinated manner. Evaluators in both exercises commented that senior staff such as nursing supervisors would not be likely to staff the unit. This was also due to the artificiality of the exercise.
Charting/Admission
Client demographics and special needs were more comprehensively analyzed, and more efforts were made to appropriately address this information in the second exercise. In the first exercise, unit staff did not pre-assign rooms in a way that would accommodate family requests to stay together and facilitate special needs of some patients. This caused confusion and hallway crowding during readjustment of room assignments. Further problems occurred when these adjustments did not happen in a timely manner. Room assignment was more organized in the second FSE, because rooms were specifically assigned and prepared based on the patient demographics and special needs. Once patients were placed in their assigned rooms, there was no need to change rooms. For example, cribs were already placed in rooms with infants, and translation devices set up in all rooms.
It was noted in the initial exercise that all required admission paperwork, including history and physical forms, symptom monitoring tools and psychosocial monitoring tools, was not completed. Only 9/15 (60%) of charts were complete with all required forms filled out. This problem was remedied in the second exercise by creating a checklist that was placed on the front of each patient chart to ensure collection and completion of all required documents. Fifteen of 15 (100%, Table 1) charts were complete in the second exercise.
Symptom Monitoring and Infection Control
Case definition and monitoring tools were received by the Incident Command Center (ICC) a full 24 hours prior to the exercise yet, in both exercises, many of the staff on the unit were both unfamiliar with and unable to explain many specific details of the illness accurately. In both exercises staff was able to clearly describe the symptoms of SARS and the differences between isolation and quarantine but most were unable to give specific details regarding the length of quarantine and the consequences of symptom detection. The Medical Director assigned to the unit in both exercises is an Infectious Disease specialist and therefore all disease related questions from the patients were deferred to him. An Infection Control Specialist was also present on the unit to counsel patients and give advice to staff on infection control practices. In the second exercise, an attempt was made to further educate unit staff about SARS with a briefing prior to duty. This briefing did not improve staff knowledge when results were compared to the past exercise (Table 1).
The evaluation, isolation and transfer of the newly symptomatic patient actor were performed more efficiently in the second exercise. The term performance in this drill is defined as the proper response as per protocols to a specific activity in which the emergency preparedness players/officials responded during this drill/exercise. This response needed to be in a coordinated manner to a timed, simulated incident. This also included the mobilization of hospital staff personnel and resources and the actual movement of emergency workers, equipment, and resources required to demonstrate coordination and response capability.
In the first exercise, the patient was evaluated within a few minutes of symptom onset but there was a delay of approximately 10 minutes before infection control precautions were applied for all staff caring for the patient. The patient was transferred off the unit within 45 minutes of symptom onset down a corridor that was not cleared by security. There were breeches in infection control precautions during the transfer of the symptomatic patient including the patient incorrectly wearing the mask, staff with open gowns and staff touching other surfaces with contaminated gloved hands. In the second exercise, at the onset of the patient's complaints of a cough, proper personal protective equipment and infection control procedure was strictly enforced. The patient was immediately transferred off the unit to an isolation room in the Medical Intensive Care Unit through an evacuated corridor. More attention was given to infection control and no breeches occurred. Decontamination and disinfection of the symptomatic patient's room was performed correctly by housekeeping in both exercises. When questioned, housekeeping staff were able to correctly answer questions regarding the suspected infectious agent and proper procedure for cleaning of the room.
Client Management
Patients received information regarding stress reduction and support services available at KCHC. Services were available from Social Work, Crisis Intervention and the Department of Psychiatry throughout both drills. When called, service providers arrived in a timely fashion and assisted patients appropriately. Religious services were also provided to patients upon request. Patients were given access to many amenities such as computers, telephone access, video games and DVD players for children. The children's services provided were age appropriate and helped to alleviate stress to children and families. Food delivery was late and inadequate in the first exercise but this problem was corrected in the second exercise. Neither a walking tour of the unit nor a daily schedule was given to patients in either exercise. Visiting policies and smoking policies were clearly explained to all patients. Patients felt well taken care of, and responded positively to all questions related to their management.
Discussion
The results of the initial FSE found that there were incomplete critical tasks (Table 1) within all five protocols: Activation of the unit, Staffing, Charting/Admission, Symptom Monitoring and Infection Control and Client Management. These deficiencies were detailed in an After Action Report, and an Improvement Plan was presented to the KCHC Disaster Preparedness Committee a month after the initial FSE. In the second FSE, all critical tasks for Activation of the unit, Staffing and Charting/Admission were achieved. Completion of critical tasks related to Symptom Monitoring and Infection Control and Client Management was improved in the second FSE, but some tasks were still not performed appropriately.
This exercise highlighted the need for an Infectious Disease Task Force during an infectious quarantine event. This has been demonstrated by various governmental groups when handling outbreaks. For example, the Department of Defense Science Board recommended the establishment of such a task force for the SARS outbreaks of 2003-2004.Reference Lederburg and Gibson5-7 This should be a group of Infectious Disease and Infection Control specialists. This team should communicate directly with the Department of Health or CDC to obtain up-to-date information about the infectious illness in question. These individuals will be responsible for quarantine-specific decisions regarding precautions and the posting of appropriate CDC signage. A member of this team should also be assigned the role of Health Educator to train staff and aid in patient education. Such a task force was not created for either FSE, and would have improved staff performance in the area of symptom monitoring and infection control.
All unit staff should receive more training about the infectious illness for which quarantine is in place. Training should be provided in advance for staff assigned to the unit and “Just in Time Training’ modules should be available for those assigned to the unit during the quarantine period. A refresher “Just in Time Training’ should also be offered to the staff. The EOC, in conjunction with the Infection Control and Infectious Disease Departments, should create training material (lecture/slides) to educate staff prior to stationing them on the unit for duty. This training would include a review of infection control precautions (including but not limited to hand hygiene and use of personal protective equipment) and disease-specific details (incubation period, mode of spread and infection control measures). These trainings should be given by the Health Educator.
Exercise evaluators and actors also suggested that a proper walkthrough of the unit, or at least a detailed description of the layout with a unit map, should have been conducted with all patients to alleviate the stress of being placed into quarantine.
Based on the results of these exercises, the Adaptable Quarantine Manual is a good guide for institutions to use in preparation for quarantine. One of the main difficulties noted in using the manual was its general nature. Kings County Hospital Center staff had some difficulty using the guide to create a plan that was tailored to the specific event they were facing. One way to improve the current manual is to include chapters with fill in the blank type plans for different specific quarantine events. This could include specific symptoms and infection control procedures. Institutions could therefore create a very event-specific guide each time quarantine was mandated.
Conclusion
The purpose of this exercise was to test the utility and feasibility of quarantine protocols with two FSEs timed one year apart. Lessons learned from these exercises, including logistical set-up or readiness of the unit, receipt of quarantined individuals, infection control procedure and the services and the staff needed for the quarantine unit, will improve operations.
In short, these exercises identified critical needs in disaster preparedness of the KCHC Quarantine Unit. The lessons learned from this logistical exercise enabled the planning group to have a better understanding of leadership needs, communication capabilities, and infection control procedures. Kings County Hospital Center performed well during these exercises. It was clear that performance in the second exercise was improved, and many problems noted in the first exercise were corrected. Staff comments at the debriefing stated that they also felt better prepared for the second exercise. This supports the idea that frequent exercises are vital to maintain disaster readiness. This study did not address the frequency of exercises required to maintain readiness, and this may be the topic of future study.



