Introduction
Approximately 2.3 million people in the United Kingdom have been diagnosed with type 2 diabetes and this figure is expected to continue to rise (Diabetes UK, 2010). Although medication plays a key role in type 2 diabetes self-management, attention to diet and physical activity is also important in order to prevent long-term complications (Kulkarni, Reference Kulkarni2006; Hayes et al., Reference Hayes, Herbert, Marrero, Martins and Muchnick2008). According to national clinical guidance in the United Kingdom (National Institute for Health and Clinical Excellence, 2008), structured education is a key priority and should be offered to every person with diabetes and/or their carer at and around the time of diagnosis, with reinforcement and review on an annual basis. Health-care professionals facilitate and support this education; however, the responsibility for lifestyle self-management ultimately rests with the patient and can be difficult to achieve and maintain.
Understanding patient barriers to lifestyle change is essential in order to help prioritise areas for intervention and formulate appropriate education materials or programmes. Most of the qualitative information in this area comes from studies in the United States and Canada (El-Kebbi et al., Reference El-Kebbi, Bacha, Ziemer, Musey, Gallina, Dunbar and Phillips1996; Maillet et al., Reference Maillet, D'Eramo Melkus and Spollett1996; Sullivan and Joseph Reference Sullivan and Joseph1998; Wang et al., Reference Wang, Abbott, Goodbody, Hui and Rausch1999; Savoca and Miller Reference Savoca and Miller2001; Dye et al., Reference Dye, Haley-Zitlin and Willoughby2003; Kieffer et al., Reference Kieffer, Willis, Odoms-Young, Guzmaz, Allen, Two Feathers and Loveluck2004; Vijan et al., Reference Vijan, Stuart, Fitzgerald, Ronis, Hayward, Slater and Hofer2005; Devlin et al., Reference Devlin, Roberts, Okaya and Xiong2006; Nagelkerk et al., Reference Nagelkerk, Reick and Meengs2006; Carbone et al., Reference Carbone, Rosal, Torres, Goins and Bermudez2007), with few studies in the United Kingdom exploring barriers to dietary change (West and McDowell, Reference West and McDowell2002; Lawton et al., Reference Lawton, Parry, Peel and Douglas2005). In addition, although some studies have explored attitudes and beliefs towards self-management among patients with established type 2 diabetes, few have explored these factors specifically among patients who have been recently diagnosed. In the last 10 years, diabetes education has become a priority area in primary and secondary care and many education programmes are now embedded within patient care packages. Against this background of increased diabetes education, there are few contemporaneous explorations of patient's views about lifestyle self-management. Such research is vital in order to identify areas that require further support, refinement or enhancement in terms of patient education.
The aim of this study was to explore the views of individuals recently diagnosed with type 2 diabetes in relation to the self-management of dietary intake and physical activity. Furthermore, there is some evidence that diabetes educators and health professionals (HPs) may view barriers and diabetes care differently from patients (Pendleton et al., Reference Pendleton, House and Parker1987; Shultz et al., Reference Shultz, Sprague, Branen and Lambeth2001; Woodcock and Kinmonth Reference Woodcock and Kinmonth2001; Carbone et al., Reference Carbone, Rosal, Torres, Goins and Bermudez2007), and health-care providers may be able to identify concerns that patients do not verbalise themselves; therefore, a secondary aim was to elicit the views of health-care providers and compare these views with those of the patients.
Methods
Overview
Given the study aims, a narrative qualitative approach was adopted that was operationalised through structured interviews with HPs and focus groups with patients. Patients are no longer regarded as passive recipients of health care. They have become active participants, and narrative methodologies play a valuable role in participatory health research and are increasingly relevant in the current climate of public and patient involvement strategies (Gregory, Reference Gregory2010). Narrative research methodologies serve as a medium for ‘getting inside’ complex health care and social care behaviours and relationships (Hsu and McCormack, Reference Hsu and McCormack2012). Narrative data may be acquired through many methods; focus groups were chosen for this study owing to their explicit use of group interaction to produce unique data (Barbour and Kitzinger, Reference Barbour and Kitzinger1999) and, thus, their potential to generate data that may not become apparent using other methods. According to Krueger and Casey (Reference Krueger and Casey2000), the purpose of a focus group is to promote a comfortable atmosphere of disclosure in which people can share their ideas, experiences and attitudes about a topic (Krueger and Casey, Reference Krueger and Casey2000). Given the study aim, the interaction between individuals was viewed as potentially being very important in order to fully allow patients to share and discuss their perceptions and experiences of managing the lifestyle aspects of type 2 diabetes. Focus groups with HPs were not possible owing to their busy working schedules; therefore, individual interviews were used. This research was conducted between December 2007 and September 2008.
Recruitment and participants
A purposive sample of HPs with varied areas of expertise was invited to participate in face-to-face interviews. All were involved in the care of people diagnosed with type 2 diabetes. A hospital dietitian, a diabetes specialist nurse and two diabetologists were invited from the Regional Centre for Endocrinology and Diabetes, Royal Victoria Hospital, Belfast, United Kingdom. An academic specialist, a community dietitian and a general practitioner from the local area were also invited. All those invited agreed to participate.
Patients were also purposively sampled; letters of invitation were sent to patients from the Regional Centre for Endocrinology and Diabetes, Royal Victoria Hospital, Belfast, United Kingdom, who had been recently (within the previous 24 months) medically diagnosed with type 2 diabetes. All had completed or partially completed the preliminary diabetes education programme at the hospital, which consists of two half-day group education sessions covering a range of topics related to type 2 diabetes including foot care, eye care, nutrition and exercise. All newly diagnosed type 2 diabetes participants are invited to take part, but not all attend. Sessions are held monthly, following which patients are offered at least one one-to-one visit with the Centre's dietitian (amount varies according to their needs, but they are usually asked to return every six months). This study was approved by the Office for Research Ethics Committees Northern Ireland. A written informed consent was obtained from all participants.
Data collection
The schedules for the interviews with HPs and focus groups with patients are shown in Table 1. The schedules were devised based on the existing literature together with input from the research team who reviewed the questions for content validity before data collection. Interview questions for HPs focussed on how patients react to their initial diagnosis, what HPs think patients find easy or difficult about making lifestyle changes, how well patients self-manage their condition and any misconceptions held by patients (Table 1). Each interview was held by the same trained interviewer and lasted for ~30–40 min.
Table 1 Interview schedule for HPs and patients

HPs = health professionals.
Focus groups were conducted with people who had been recently diagnosed with type 2 diabetes. As detailed in Table 1, questions for discussion were similar to those used in the interviews with HPs. Each focus group lasted for ~1 h and was conducted in a quiet room within the Regional Centre for Endocrinology and Diabetes facility. One trained facilitator was responsible for conducting all groups.
Data analysis
All interviews and focus groups were tape recorded, transcribed verbatim and analysed by emergent themes analysis; A.B. and a second researcher independently developed a coding structure after reading and rereading the transcripts. This was followed by a discussion and comparison of the codes (themes and sub-themes) to verify the validity and reliability of their application; any discrepancies were resolved satisfactorily and the coding framework was then applied to the transcripts using NVivo to manage the coded data (QSR NVivo version 8, QSR International). Given the qualitative nature of the data, findings are reported in broad terms (ie, most, many, several, some and few).
Results
Sample
Six focus groups were held with people who had been diagnosed with type 2 diabetes within the previous 24 months (n = 16; two to four per group, 38% female, 60.2 ± 7.5 (mean ± SD) years of age). Sixty-nine percent were married, 38% completed college or technical college and 38% stated secondary school was their highest level of schooling. Seven HPs were interviewed.
Barriers to lifestyle change
A number of barriers to lifestyle change were identified and divided into six main categories as shown in Table 2. Most of the barriers discussed related to making dietary changes but a few were specific to physical activity. Many of the dietary barriers were identified by both the HPs and patients.
Table 2 Barriers to lifestyle change that emerged from discussions with people recently diagnosed with type 2 diabetes and HPs involved in their care
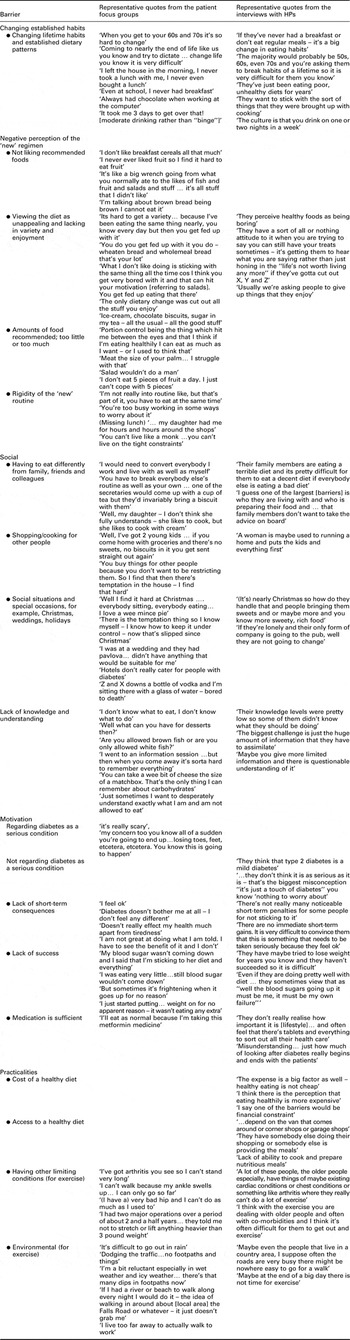
HPs = health professionals.
Difficulties changing well-established habits
The mean age of participants taking part in the focus groups was ~60 years; therefore, it is not surprising that a predominant discussion point was the concern about changing long-established habits.
When you get to your 60s and 70s it's so hard to change.
(Female, focus group 2)
Coming to nearly the end of life like us you know and try to dictate … change life you know it is very difficult.
(Male, focus group 5)
The need to make significant dietary changes appeared to be a key concern for patients and was also mentioned by HPs.
The majority would probably be 50s 60s even 70s and you're asking them to break habits of a lifetime so it is very difficult for them you know, diets very difficult for them they have maybe tried to lose weight for years you know and they haven't succeeded so it is difficult.
(Female, Specialist Nurse)
Some routines were seen as cultural habits, for example, binge drinking rather than moderate drinking as recommended, and for some the recommended changes meant a complete change to their dietary pattern, for example, starting to have breakfast when they had never done so before. Others found it difficult to change specific habits.
Like myself, even at school I never had breakfast. I went straight out. I never – and some ways since I came here because the dietitian making the point about eating in the morning – it's only in the past three, four months that I have really forced myself to eat a breakfast in the morning even though some ways I am really not that hungry but I am trying to change my eating routine which was no breakfast.
(Male, focus group 3)
Barriers relating to patients’ perception of their ‘new’ regimen
Discussions with patients also revealed several negative perceptions towards the ‘new’ or recommended regimen. Patients highlighted that they felt they were being asked to cut out foods that they found enjoyable in favour of foods they did not like. They perceived the new dietary regimen to be boring and lacking in variety and felt that the required portion control was stark (too small in some cases and too large in others), which was something they would struggle with. They also felt that the recommended diet regimen was too rigid and constrained. When considered together, these factors indicate that recently diagnosed patients view the recommended diet as unappealing and not enjoyable.
The food, going from what you normally eat to fruit all the time you know and fish – it's all stuff that I didn't like. I never had much of it. It's like a big wrench going from what you normally ate on the likes of fish and fruit and salads and stuff.
(Male, focus group 2)
What I don't like doing is sticking with the same thing all the time … I think you get very bored with it and that can hit your motivation.
(Female, focus group 6)
The fact that patients perceive the recommended dietary regimen as boring and restrictive was also verbalised in discussions with HPs.
‘They perceive healthy foods as being boring’, ‘they have a sort of all or nothing attitude to it when you are trying to say you can still have your treats sometimes – it's getting them to hear what you are saying rather than just honing in the “life's not worth living any more” if they've gotta cut out X, Y and Z’.
(Female, Dietitian)
Barriers relating to the social environment in which people live their lives
Many socially related barriers were discussed by both patients and HPs. The social network in which people live and work presented a challenge as often family or friends or work colleagues were not necessarily mindful of, or sympathetic towards, the needs of the person who had diabetes. For women, there was also an additional problem in that they were generally responsible for shopping and cooking for other people, and often their needs came secondary to the preferences of the other members of the family; inevitably, it seemed that they purchased food preferred by other family members, thus making their food choices at home more difficult. Social occasions in general were highlighted as difficult, again because there was too much temptation on offer and often a lack of healthier or more appropriate choices. The focus groups were conducted around Christmastime and many patients acknowledged that they had difficulty getting back on track afterwards (Table 2).
Even when you say to them I'm not allowed any biscuits they [work colleagues] still come up and they say ‘sure one's not going to be any harm with a cup of tea’ the problem is then you're having 4 or 5 cups of tea during the day – a working day, so you're getting 4 and 5 chocolate biscuits during the day … and then at home you kinda go out and you say right I'm not going to buy any biscuits and cakes this weekend for the groceries so you come home and the first thing somebody says is ‘what sweet stuff did you buy – did you get any biscuits?’ so they go out and buy them so it's sitting there.
(Male, focus group 3)
Their family members are eating a terrible diet and it's pretty difficult for them to eat a decent diet if everybody else is eating a bad diet.
(Male, Consultant Physician)
Lack of knowledge and understanding
HPs commented on the large amounts of information that patients are required to assimilate and did vocalise that knowledge was a barrier to positive change. Patients clearly vocalised a feeling of not being able to process and recall all the information that was provided to them and so they felt adrift.
I went to an information session which was very good went over for one afternoon and one morning but then when you come away it's sorta hard to remember everything, you know.
(Female, focus group 1)
Knowledge levels were pretty low so some of them didn't know what they should be doing.
(Female, Academic Specialist)
This lack of understanding and uncertainty was evident in discussions between participants as they frequently asked each other questions about what foods were suitable or unsuitable for consumption (Table 2). Some of the main areas of confusion related to the following: the concept of carbohydrates, both how much and what type was recommended; fruit consumption in terms of what fruits were or were not allowed and how many portions of fruit should be consumed per day; and sugar versus fat; in general more priority was given to consideration of the sugar content rather than the fat content.
I like yogurts…you have to watch the fat content, you have to watch the sugar content, and I get confused with it so I actually haven't been eating yogurt, which I really like…I just don't know which ones to go for.
(Female, focus group 1)
A critical issue in relation to knowledge and education in general was that some patients felt they received little or no information on what to eat during the initial weeks or months following diagnosis. Some ate small amounts of food due to fear of eating the wrong foods or they did try to make changes themselves only to find they had made unsuitable changes.
(I started having) honey…came here and they were horrified ‘my god you can't touch honey you know’.
(Male, focus group 4)
They (told) me that my blood sugar was far too high and it was dangerous but they didn't do anything for 10 weeks. They told me to try and bring this down to a manageable level…I'm basically not eating because they're sorta saying you know, control it and what not and I was eating very little – eating enough to stay alive but eating very little – still blood sugar wouldn't come down.
(Male, focus group 3)
Barriers relating to a lack of motivation
A general lack of motivation to make lifestyle changes was an important barrier highlighted by both patients and HPs and many factors contributed to this lack of motivation. HPs highlighted that some patients did not view diabetes as a serious condition and therefore did not feel any particular urgency to examine their lifestyle and make appropriate changes. This was not a view expressed by patients; most appeared to be well aware of the long-term consequences of type 2 diabetes and expressed fear about the possibility of becoming ill or developing complications. For some, this fear of the long-term consequences acted as an inducement to change (see section ‘Facilitators of lifestyle change’ on facilitators below).
My concern too you know all of a sudden you're going to end up…losing toes, feet, etcetera, etcetera. You know this is going to happen.
(Male, focus group 4)
Other demotivating factors included the lack of short-term consequences, which meant that some individuals had no symptoms and so no incentive to change. Some said they had tried to change their lifestyle but became disillusioned when they had not experienced any benefit, for example, blood glucose remaining high. One participant felt that medication was sufficient to take care of their diabetes and so they did not need to take any action themselves.
Human being is naturally lazy. You can't just you know force yourself you know to eat something you know you don't like…I'll eat as normal because I'm taking this metformin medicine.
(Male, focus group 5)
Barriers relating to the practicalities of changing behaviour
Two barriers were clearly discussed in relation to increasing physical activity levels by both the HPs and the patients having other limiting conditions and environmental influences (Table 2). Most of the patients had co-morbidities such as arthritis, and previous major operations that limited their ability to attempt to tolerate increased physical activity. In addition to these physical limitations, poor weather, traffic, safety concerns and lack of pleasant places to walk were among many reported environmental barriers to meeting the activity recommendations.
At different times of the year, weather isn't great so I figure ‘oh aye’ if I do my exercise but get pneumonia on the way getting me exercise or slip on the ice which again wouldn't do me any favours…I'm a bit reluctant especially in wet weather and icy weather… there's that many dips in footpaths now.
(Female, focus group 6)
I can't walk because my ankle swells up… I can only go so far.
(Male, focus group 3)
Facilitators of lifestyle change
In general, factors that facilitated behaviour change were discussed to a much lesser extent compared with barriers to behaviour change; however, several factors that aided motivation or supported behaviour change were evident from discussions. Patients reported that feeling healthier in response to making changes encouraged them to continue and many were motivated by the desire to avoid long-term health consequences or to remain well. Some patients also reported that self-monitoring of blood glucose levels and meeting set targets, such as weight loss, helped keep them motivated and the support of HPs and family members were also raised as important facilitating factors, for example, having a partner that cooks for them. HPs also mentioned setting targets, follow-up visits or additional reviews and the diagnosis itself as being motivators to change.
After the first weeks of cutting out the sugars I felt a lot better – just felt better, immediately now and I started to lose a bit of weight so I've lost over a stone and would like to lose more – a few pounds maybe, but – other than that I haven't any real problems but all the symptoms have stopped. I stopped going to the loo and I'm not thirsty, just normal …and I've been to the dietitian since in the hospital here and spent a good bit of time with her – she sorta put me right as to what perhaps I should be doing as opposed to cutting out all my sugars.
(Male, focus group 4)
Family support's been great you know… wife and daughter – both for different reasons – one wants to lose the weight and one wants to stay off the chocolate so they are happy enough to go along with whatever is happening.
(Male, focus group 4)
Discussion
In general, barriers to lifestyle change received more prominence in discussions compared with facilitating factors. These patients had been diagnosed within the previous 24 months and so may not have felt fully competent in terms of self-management. Furthermore, in general terms, exercise was also discussed to a lesser extent compared with diet, perhaps reflecting the complexity of the dietary changes that patients are required to make, but maybe also indicating that physical activity receives less prominence in education activities or it may indicate a lack of interest in physical activity by the patients.
In this study, the overriding barriers that were discussed at length and across all focus groups were patients’ concerns about changing well-established habits, coupled with a broadly negative perception of many aspects of their recommended diet and confusion about particular aspects of the diet. Patients appeared to feel overwhelmed by the number of changes they had to make to their diet. Although these factors have been reported previously (El-Kebbi et al., Reference El-Kebbi, Bacha, Ziemer, Musey, Gallina, Dunbar and Phillips1996; Savoca and Miller, Reference Savoca and Miller2001; Nthangeni et al., Reference Nthangeni, Steyn, Alberts, Steyn, Levitt, Laubscher, Bourne, Dick and Temple2002; Vijan et al., Reference Vijan, Stuart, Fitzgerald, Ronis, Hayward, Slater and Hofer2005; Nagelkerk et al., Reference Nagelkerk, Reick and Meengs2006), patients in this study were recently diagnosed (<24 months) and were on a steep learning curve with respect to diabetes self-management. Previous research in people with type 2 diabetes has highlighted that patients perceive making even moderate dietary changes to be more difficult than taking oral medications, and if their dietary regimen has been designed to promote weight loss, it is viewed as having a burden similar to that of twice daily injections (Vijan et al., Reference Vijan, Stuart, Fitzgerald, Ronis, Hayward, Slater and Hofer2005). Making dietary changes is a challenge not only for patients but also for HPs who must work towards making these changes appear less daunting, more manageable, more appealing and more achievable for patients.
Patients in this study, and many others (El-Kebbi et al., Reference El-Kebbi, Bacha, Ziemer, Musey, Gallina, Dunbar and Phillips1996; Savoca and Miller, Reference Savoca and Miller2001; Nagelkerk et al., Reference Nagelkerk, Reick and Meengs2006; Carbone et al., Reference Carbone, Rosal, Torres, Goins and Bermudez2007), felt they were not as knowledgeable in some areas as they would have liked and felt confused about a lot of specific details (mainly quantity, type and amount of foods ‘allowed’). Knowledge acquisition is a central aim of diabetes education programmes as it is fundamental to skills acquisition and enhancement of self-efficacy. It is noteworthy in this study that even though all of the participants had attended one or two group education session(s), knowledge and confusion about diet remained a major barrier for these patients. This has also been noted in many studies where most, or all, participants had attended a group education session (El-Kebbi et al., Reference El-Kebbi, Bacha, Ziemer, Musey, Gallina, Dunbar and Phillips1996; Savoca and Miller, Reference Savoca and Miller2001; Vijan et al., Reference Vijan, Stuart, Fitzgerald, Ronis, Hayward, Slater and Hofer2005; Nagelkerk et al., Reference Nagelkerk, Reick and Meengs2006). This may be related to both the amount of information that is conveyed to patients in a short period of time and the way in which it is conveyed. Repeated exposures to this new information in more manageable amounts may be required to build knowledge and confidence in this area. Provision of information in stages (which is the case in some, but not all, education programmes), alongside access to resources that can be used by patients in their own time and at their own pace outside of the formal education sessions, may be helpful. Such resources could be designed to assist with knowledge acquisition while also helping with self-monitoring and goal setting, thus helping to provide ongoing support to patients.
In relation to knowledge, one important issue was the fact that some patients felt they had been ‘left in the dark’ for months after being initially diagnosed as they received little or no information on what to eat during that period, so some ‘didn't eat anything’ and others made what they subsequently found were unsuitable changes. This is something that, to our knowledge, has not been highlighted previously and is worthy of exploration in other groups of patients and other health-care systems as it presents a significant gap that may need to be addressed.
Patients and HPs’ views of physical activity were also explored; patients appeared to place much less emphasis on exercise when compared with diet as reflected in the extent of discussions around this topic, something that was also noted by Nagelkerk et al. (Reference Nagelkerk, Reick and Meengs2006) in their study of patients with type 2 diabetes in a rural setting in America. In this study, the main barriers identified were in relation to having other co-morbidities and barriers related to the physical environment, both of which have been observed in previous research (Thomas et al., Reference Thomas, Alder and Leese2004; Dutton et al., Reference Dutton, Johnson, Whitehead, Bodenlos and Brantley2005; Lawton et al., Reference Lawton, Ahmad, Hanna, Douglas and Hallowell2006). Physicians and nurses should consider these activity-related barriers alongside diet-related barriers in order to provide the most appropriate advice for each individual and ensure that advice to increase physical activity receives equal prominence to dietary advice; making changes towards a healthier activity pattern may help patients see positive effects quicker and thus assist with motivation.
Only a few barriers that have been frequently mentioned in other studies were not directly discussed in the present study, the most common one being poor communication with health-care providers. In many cases, this barrier refers to a lack of understanding by the health practitioner of cultural needs and financial situations of the patients (Quatromoni et al., Reference Quatromoni, Milbauer, Posner, Carballeira, Brunt and Chipkin1994; Maillet et al., Reference Maillet, D'Eramo Melkus and Spollett1996; Savoca and Miller, Reference Savoca and Miller2001; West and McDowell, Reference West and McDowell2002; Dye et al., Reference Dye, Haley-Zitlin and Willoughby2003; Lawton et al., Reference Lawton, Parry, Peel and Douglas2005; Vijan et al., Reference Vijan, Stuart, Fitzgerald, Ronis, Hayward, Slater and Hofer2005; Devlin et al., Reference Devlin, Roberts, Okaya and Xiong2006; Nagelkerk et al., Reference Nagelkerk, Reick and Meengs2006). The participants in this study attended a clinic in an area of lower socio-economic status and perhaps the health practitioners were cognizant of this fact and tailored their communications accordingly. Supporting this, cost was mentioned as a barrier by few HPs in the present study, and is frequently cited as a barrier in other studies (Quatromoni et al., Reference Quatromoni, Milbauer, Posner, Carballeira, Brunt and Chipkin1994; El-Kebbi et al., Reference El-Kebbi, Bacha, Ziemer, Musey, Gallina, Dunbar and Phillips1996; Wdowik et al., Reference Wdowik, Kendall and Harris1997; Wang et al., Reference Wang, Abbott, Goodbody, Hui and Rausch1999; Hwang and Bugeja, Reference Hwang and Bugeja2000; Kieffer et al., Reference Kieffer, Willis, Odoms-Young, Guzmaz, Allen, Two Feathers and Loveluck2004; Vijan et al., Reference Vijan, Stuart, Fitzgerald, Ronis, Hayward, Slater and Hofer2005; Nagelkerk et al., Reference Nagelkerk, Reick and Meengs2006; Carbone et al., Reference Carbone, Rosal, Torres, Goins and Bermudez2007; Simmons et al., Reference Simmons, Lillis, Swan and Haar2007), but not was not raised as an issue by patients. Another barrier that has often been identified in other studies was the apparent time-consuming nature of the diet (El-Kebbi et al., Reference El-Kebbi, Bacha, Ziemer, Musey, Gallina, Dunbar and Phillips1996; Savoca and Miller, Reference Savoca and Miller2001; Carbone et al., Reference Carbone, Rosal, Torres, Goins and Bermudez2007). This barrier may have been less of a concern in the present study as most of the participants were retired, and, in the case of most of the men, responsibilities for food preparation rested with their partners.
A secondary aim of this study was to elicit the views of HPs and compare them with those of the patients as some evidence suggests that these two groups of individuals may have different views about diabetes self-care (Woodcock and Kinmonth, Reference Woodcock and Kinmonth2001; Nthangeni et al., Reference Nthangeni, Steyn, Alberts, Steyn, Levitt, Laubscher, Bourne, Dick and Temple2002; Lawton et al., Reference Lawton, Parry, Peel and Douglas2005; Carbone et al., Reference Carbone, Rosal, Torres, Goins and Bermudez2007). In general, there was a high level of agreement between the barriers identified by patients and those identified by HPs; however, HPs did highlight a few barriers that the patients did not confirm. For example, patients expressed a much more negative perception of the new dietary regimen than HPs. Although HPs did note that many patients viewed the diet as boring or unappealing, they did not pick up on the related issues surrounding their preference for habitual foods rather than the new foods, the issues with recommended portion sizes and the difficulties patients felt with regard to having to follow a more regimented routine in general with respect to food. The patient groups were more homogeneous than the HPs (ie, all attended the same Centre), which may account for some of the differences in views expressed. Despite this, these appear to be critical issues that need to be considered when communicating with patients.
The limitations of this study must be borne in mind. The patients who participated in this study were a self-selected group of patients from a large regional diabetes clinic in Northern Ireland and so their views may not be representative of all recently diagnosed patients. More males participated than females, and although men may hold different views stark differences were not apparent in this study. The participant numbers were low, which may affect generalisability of the data, and the findings should be considered with this in mind; however, each group in this study provided consistent information and the researchers felt that saturation of ideas and themes had been reached after four focus groups. Even so, the possibility remains that further barriers may be elucidated given further exploration of this topic; many other interrelated factors that affect a patient's ability to self-manage their condition such as psychological well-being (Peyrot et al., Reference Peyrot, Rubin, Lauritzen, Snoek, Matthews and Skovlund2005) and depression (Vickers et al., Reference Vickers, Nies, Patten, Dierkhising and Smith2006) were also not explored in this study. The small number of HPs interviewed may also affect generalisability of the results; however, care was taken to include a variety of HPs who are involved in the care of patients with type 2 diabetes.
Conclusion
Even against a background of diabetes education, patients recently diagnosed with type 2 diabetes discussed a wide range of barriers to self-management of diet and physical activity, with facilitating factors receiving much less attention. HPs generally echoed the views of patients but perhaps underestimated the depth and breadth of the negative feelings that patients held towards the recommended dietary regimen. Support for diabetes self-management must try to make the required lifestyle changes more appealing and achievable and, in general, should also place more emphasis on physical activity. Consideration needs to be given as to how best to support people in the period between receiving their initial diagnosis and being offered diabetes education, which can often be a few months, as some patients feel that they are ‘on their own’ during this period. Qualitative research of this nature should be conducted on a regular basis in order to continue to prioritise areas for improved education, develop appropriate education tools and explore how these barriers and facilitators change over time.
Practice implications
The major challenge for HPs and those designing resources for people with type 2 diabetes remains communicating a large volume of information in a manageable form that will make lifestyle self-management seem like a tangible goal. There is certainly scope for developing further resources to assist HPs in this regard; HPs have an important role to play in providing key support to patients, as illustrated in this study, but education resources that patients can use on an ongoing basis to supplement structured education programmes delivered in health-care settings are also required. Importantly, such resources may also be valuable to patients who experience a delay between their diagnosis and receipt of more structured dietary education.
Acknowledgements
The authors would like to thank the people with type 2 diabetes who volunteered to participate in this study. This study was supported by a research grant from The Sugar Bureau (United Kingdom). The funding source had no involvement in the research process and the authors are solely responsible for the results and conclusions herein. The authors have no competing interests to declare. Ethical statement: We confirm that all personal identifiers have been removed or disguised so the patients described are not identifiable and cannot be identified through the details of the story.




