COVID-19 was declared a pandemic by the WHO in March 2020 and has since evolved into an unprecedented public health crisis leading to economic and social crises. In several countries, the COVID-19 pandemic has disrupted access to food, led to food shortages, loss of disposable household income, increased food prices and altered dietary practices(Reference Torero1). The pandemic has threatened millions of families living with or at risk for development of food insecurity(Reference Paslakis, Dimitropoulos and Katzman2). In a world where nutrition-related issues, including obesity, malnutrition and food insecurity, already impact the majority of its population(3), further exacerbation of food insecurity, malnutrition and obesity imposed by the COVID-19 pandemic are expected and likely to magnify disparities in healthy lifestyle behaviours, aggravating the global burden of diet-related chronic diseases(Reference Huizar, Arena and Laddu4). In addition, malnutrition has been associated with a higher risk for SARS-CoV-2 infection and, when contracted, more severe cases (e.g. hospitalisation, mechanical ventilation)(Reference Gao, Zheng and Wang5). In particular, malnutrition is suggested to contribute to obesity just as obesity may contribute to malnutrition, and both are driven by unhealthy dietary behaviours, especially in the presence of food insecurity(Reference Swinburn, Kraak and Allender6).
Food insecurity is generally defined as consistent worry or concern about access to adequate amounts of affordable and nutritious foods at all times(Reference Coleman-Jensen, Rabbitt and Gregory7). Conceptualisations of food insecurity in high-income countries primarily focus on the economic aspect; for example, the Household Food Security Survey Module(8), which is commonly used in the USA and Canada, measures uncertain or inadequate access to food due to financial constraints. The lack of consistent access to nutritious foods has been found associated with chronic physical and mental health problems(Reference Martin, Maddocks and Chen9).
In Belgium, strict confinement measures to curb the spread of COVID-19 were introduced on 13 March 2020. The confinement measures included closure of hotels, bars and restaurants as well as schools/universities, non-essential industries and cultural, recreational or sportive activities.
The aim of the current study was to assess different levels of food insecurity in Belgium and associations with changes in nutritional habits among the adult population during the COVID-19 confinement measures.
Methods
Three online health surveys were organised during the confinement period. The first COVID-19 health survey was launched 3 weeks after the start of the confinement (2 April), the second survey took place 2 weeks later (16 April) and the third one was distributed on 28 May 2020. All three surveys were developed with LimeSurvey version 3 and were available online for 1 week.
Sampling and recruitment
No sampling was performed. Recruitment of adults residing in Belgium was done through launching the surveys on the website of Sciensano and other health-related organisations (health insurance, community centers, etc.), through snow balling and by the press and social media.
People who had indicated in a given survey that they would like to take part in the next one received an invitation through the e-mail address they provided.
Study population
The data for the purposes of this study were derived from the second and the third COVID-19 health survey, as the second survey included specific questions on changes in nutrition-related behaviours while the third survey included questions on household food insecurity. In total, 53 419 Belgian adults participated in the second survey, while 37 409 participated in the third survey. In total, 15 849 participants mentioned in survey 3 that they participated in the previous surveys, agreed to link their data and provided an email address for the linkage. For 8640 participants, the data from survey 2 and survey 3 could effectively be linked based on e-mail, gender, year of birth and post code.
Variables
Food Insecurity
The questions on food insecurity at the household level were derived from the USDA Household Food Security Survey Module(8) and enquired about the last 30 d. For the following three questions, it was asked whether they were often true, sometimes true or never true for the household (option do not know/refused was also foreseen):
– I/We worried whether my/our food would run out before I/we got money to buy more
– The food that I/we bought did not last, and I/we did not have money to get more
– I/we could not afford to eat healthy balanced meals
Three indicators were created:
– Often or sometimes feared that food would run out before there is money to buy more over the last month (yes/no).
– Often or sometimes the food purchased did not last long enough, and there was no money to buy more over the last month (yes/no)
– Often or sometimes not being able to afford to eat a healthy and balanced diet over the last month (yes/no)
Changes in dietary behaviours
For four selected food groups (the same ones as included in the regular Health Interview Surveys), the question ‘Has the consumption of the following foods increased, remained unchanged or decreased since the start of the confinement (13 March 2020)?’ was included:
-
1. Fruits, excluding juice squeezed from fresh fruit or made from concentrate
-
2. Vegetables or salad, excluding potatoes and fresh juice or juice made from concentrate
-
3. Sugared soft drinks, i.e. lemonade, cola or ice tea (not include ‘light’)
-
4. Sweet or salty snacks such as candy, chocolate, cake, biscuits, ice cream, chips, etc.
Changes in weight status
A question on change in weight status since the start of the confinement (13 March 2020) was included with the following answer options: (1) Yes, lost weight (2) Yes, gained weight (3) No, my body weight remained stable (4) Don’t know/refused.
Socio-demographic characteristics
Gender, educational attainment (secondary school diploma or less v. higher education), household composition (living alone, couple without child(ren), couple with child(ren), living alone with child(ren), living with parents, family, friends and other) and average monthly household’s net income (after deducting taxes and social security contributions) (less than 1500 euro per month, 1500–2000 euro per month, 2000–2500 euro per month, 2500–5000 euro per month and more than 5000 euro per month) were defined as socio-demographic covariates which could have a possible association with food insecurity.
Data analysis
The indicators for food insecurity were described by household composition and education level. Since the study sample was biased at the level of region (underrepresentation of the Flemish Region and overrepresentation of the Walloon Region), gender (overrepresentation of women), age group (underrepresentation of the youngest (18–24) and oldest (65+)) and educational attainment (underrepresentation of the low educated), post-stratification weights were calculated using Labor Force Survey (LFS) 2016 data as auxiliary database. The calculation of the weights was based on cross classified LFS 2016 data on age, gender, province and education.
As ordered logistic regression was not possible due to proportional odds assumptions not being met, multinomial logistic regression models were used to determine the associations between self-reported changes in dietary behaviours or weight status as the dependent variables and food insecurity indicators as the independent variables, adjusted for gender, household composition, educational attainment and average monthly disposable household income. Both crude and adjusted OR with 95 % CI and the P-value were presented. All the analyses were performed with SAS® 9.4.
Results
Food insecurity in Belgium
About 10·4 % of Belgian adults (10·8 % of women and 8·9 % of men) often or sometimes feared food shortages over the last month (May 2020). This percentage was lowest among over-65s (5·0 %) and highest among the age group 25–44 years (13·4 %). There were large differences between individuals according to the household composition: the fear of food shortage was highest among single parent families with children (26·7 %) and single persons (14·7 %) and lowest among couples without children (6·2 %). There was a significant difference between individuals with a diploma of secondary education or lower (13·0 %) and individuals with a diploma of higher education (3·8 %) (Fig. 1).
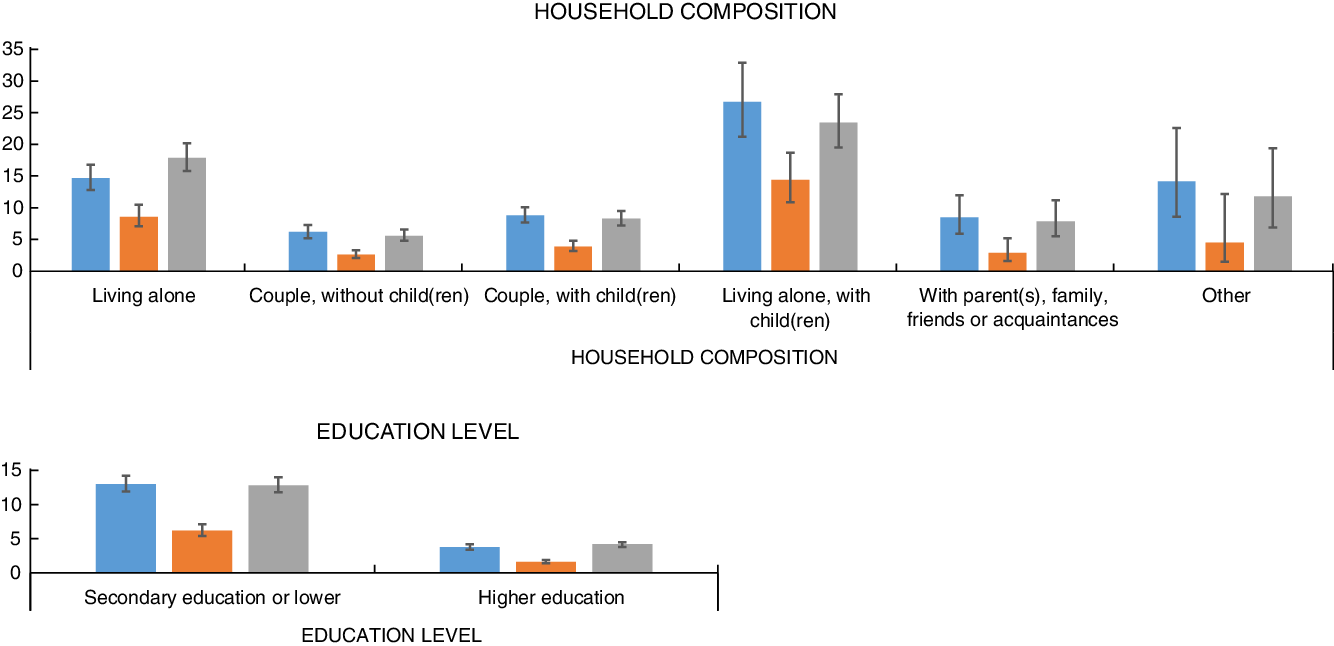
Fig. 1 Percentage (95 % CI) of the population aged 18 years and over who often or sometimes feared food shortages (n 30 114), who effectively suffered from food shortages (n 30 065) and who could not afford to eat a healthy and balanced diet (n 30 093) during the confinement measures according to the household composition (above) and education level (below); third COVID-19 Health Survey Belgium 2020. ![]() , % Fear for shortage;
, % Fear for shortage; ![]() , % Shortage;
, % Shortage; ![]() , % Could not afford a balanced, healthy diet
, % Could not afford a balanced, healthy diet
About 5·0 % of Belgian adults (5·2 % of women and 4·8 % of men) were often or sometimes short of food and had no money to buy more over the last month (May 2020). This percentage was lowest among over-65s (2·1 %) and highest among the 25–34 and 35–44 age groups (6·1 and 6·7 %, respectively). Also for this indicator there were large differences between individuals according to the household composition: the percentage of individuals experiencing food shortages was highest among single parent families with children (14·4 %) and single persons (8·6 %) and lowest among couples without children (2·6 %) (Fig. 1). There was a significant difference between individuals with a diploma of secondary education or lower (6·2 %) and individuals with a diploma of higher education (1·6 %) (Fig. 1).
About 10·3 % of Belgian adults (10·0 % of women and 9·6 % of men) could often or sometimes not afford to eat a healthy and balanced diet over the last month (May 2020). This percentage was lowest among the over-65s (5·2 %) and highest among the 25–34 age group (13·6 %). The percentage of individuals who could not afford to eat healthy and balanced food was highest among single parent families with children (23·4 %) and single persons (17·9 %) and lowest among couples without children (5·6 %). There was a significant difference between individuals with a diploma of secondary education or lower (12·8 %) and individuals with a diploma of higher education (4·2 %) (Fig. 1).
Associations between changes in nutritional habits during confinement and different indicators of food insecurity in Belgium
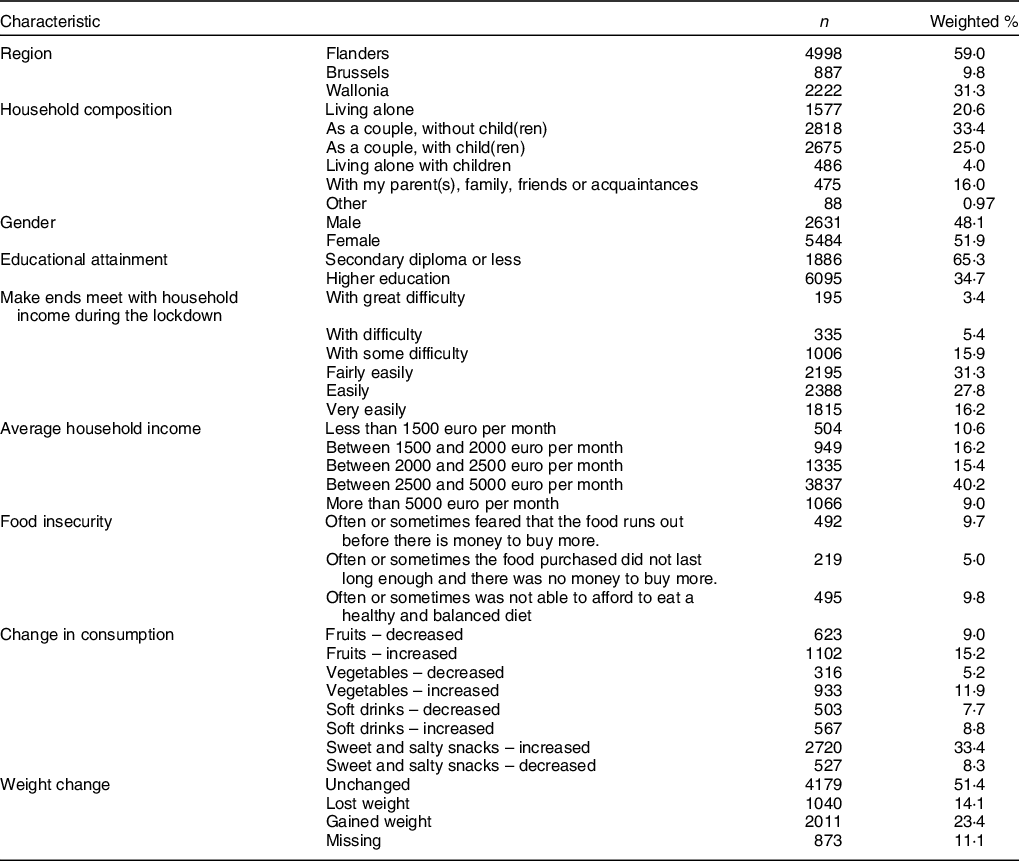
The regression analyses included 23·1 % of participants from survey wave 3, for which a link could be made to the results on nutritional behaviour changes included in survey wave 2. About 52 % of those participants were female, 21 % was living alone and 4 % living alone with children. About 35 % of those participants attained higher education. About 25 % of these participants had some or great difficulty to make ends meet (Table 1).
Table 1 Study population characteristics (n 8122); second and third COVID-19 health survey, Belgium 2020
Adults who often or sometimes feared over the last month that food would run out before there is money to buy more during confinement had significantly higher odds of decreased v. unchanged fruit (3·53; 95 % CI = 2·06, 6·05) and vegetable (5·42; 95 % CI = 2·90, 10·11) consumption and significantly higher odds of increased v. unchanged soft drink consumption (3·79; 95 % CI = 2·20, 6·54), adjusted for socio-demographic covariates. Similar results were found for adults who often or sometimes ran out of food over the last month before acquiring sufficient financial means to buy more (fruit: 3·59; 95 % CI = 1·69, 7·61; vegetables: 7·58; 95 % CI = 3·45, 16·66; soft drinks: 3·97; 95 % CI = 1·79, 8·79) and for adults who often or sometimes were not able to afford a healthy and balanced diet over the last month (fruit: 4·05; 95 % CI = 2·39, 6·86; vegetables: 6·74; 95 % CI = 3·68, 12·35; soft drinks: 2·96; 95 % CI = 1·69, 5·19). For sweet and salty snack consumption and weight change the results were mixed. Adults who were food insecure according to all three indicators had significantly higher odds of both decreased v. unchanged and increased v. unchanged sweet and salty snack consumption. The same was found for weight change (Table 2).
Table 2 Associations between changed consumption of certain food groups (decreased and increased v. unchanged) or weight status (decreased and increased v. unchanged) during the confinement measures and food insecurity measured by three different indicators by means of crude and adjusted* OR with 95 % CI and p-value; second and third COVID-19 health survey, Belgium 2020
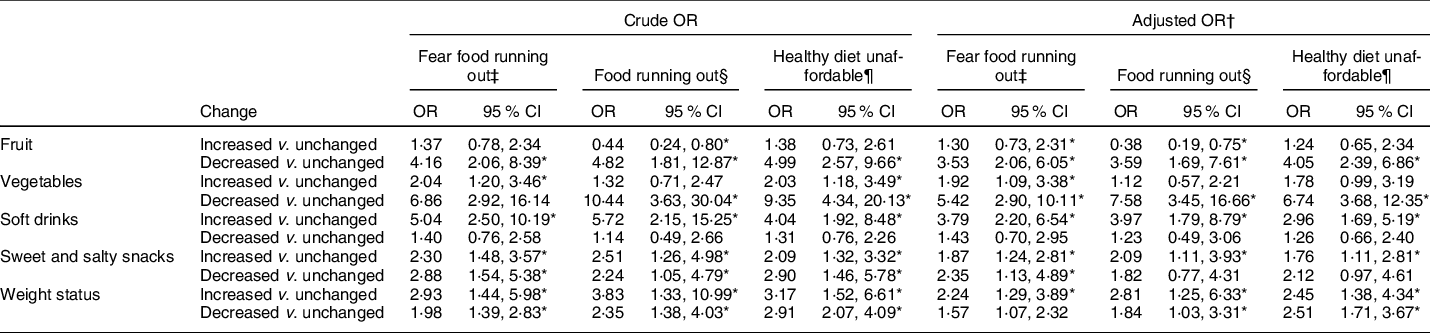
* P < 0·01.
† Adjusted for gender, household composition, education level, region, average disposable household income.
‡ Fear food running out: Often or sometimes fear that the food runs out before there is money to buy more over the last month.
§ Food running out: Often or sometimes the food purchased did not last long enough and there was no money to buy more over the last month.
¶ Healthy diet unaffordable: Often or sometimes not being able to afford to eat healthy and balanced food over the last month.
Discussion
This population-weighted online survey conducted during the COVID-19 confinement measures in Belgium found that food insecurity was considerably high, in particular for adults living alone, with or without children. However, it is important to note that we do not have baseline data to compare these figures to levels of food insecurity in Belgium before the start of the COVID-19 pandemic. The study showed that the risk for adverse changes in most dietary behaviours was significantly higher among those experiencing food insecurity, from not being able to afford a healthy diet, to actually running out of financial means to buy sufficient food. Changes in food prices and disposable household income may also have impacted dietary behaviours during confinement.
Strengths of the survey include the large sample, limitations include convenience sampling, the use of multinomial logistic regression, self-reported intake and weight status, different assessment timing for food insecurity and nutritional habits, lack of data on ethnicity, limited information on dietary habits and the lack of baseline measures on food insecurity for Belgium as part of national surveys.
Food insecurity has been scarcely assessed in Belgium. It is not part of the regular health interview surveys or the food consumption surveys. The best estimate currently available is Eurostat’s food poverty indicator: In 2018, 8·8 % of people 16 years or older in Belgium declared that they were unable to afford a meal with meat, chicken, fish (or vegetarian equivalent) every second day(10). In 2019, 168 476 people (about 1·5 % of the population) used at least once the services of the Belgian Federation of Food Banks. This number has been growing steadily since 2005(11).
The United Nations World Food Program has estimated that, due to COVID-19, 265 million people could face acute food insecurity by the end of 2020, almost doubling the number of people under severe threat of food insecurity around the world(12). A study in Vermont among a convenience sample of 3219 respondents found that there was nearly a one-third increase (32·3 %) in household food insecurity since COVID-19 (P < 0·001), with 35·5 % of food insecure households classified as newly food insecure(Reference Niles, Bertmann and Belarmino13). Respondents experiencing household food insecurity had higher odds of facing food access challenges and utilising coping strategies, including two-thirds of households eating less since COVID-19 (P < 0·001). The rise in food insecurity prevalence in the USA has induced a 98 % increase in the demand and reliance on receiving food from local food banks and an increase in enrollment and service expansion of supplemental nutrition aid programmes(14).
Due to rising levels of food insecurity in several countries, altered dietary habits, such as shown in this study, and the link between malnutrition and severity of SARS-COV-2 infection, the COVID-19 pandemic has presented numerous clear opportunities to shift unhealthy eating behaviours and unhealthy food environments to those that promote healthier dietary behaviours. A stronger response from governments is urgently needed to tackle the multiple burdens of malnutrition and food insecurity to protect public health from ongoing and future pandemics. Monitoring of food insecurity should be included in planned and ongoing population health surveys.
The continuity of food assistance programmes combined with tailored efforts to ensure access to diverse and nutritious diets to vulnerable population groups are paramount to alleviate food insecurity and the cascading effects leading to negative health outcomes.
In conclusion, food insecurity during the COVID-19 confinement measures in Belgium was associated with adverse changes in most dietary behaviours. A strong government response is needed to tackle malnutrition and food insecurity to protect public health from ongoing and future pandemics.
Acknowledgements
Acknowledgements: The authors would like to thank all the individuals who participated in the COVID health surveys in Belgium. Financial support: No funding was obtained for this study. Conflicts of interest: The authors declare they have no conflicts of interest in regard to this study. Authorship: K.D. and S.D. lead the surveys; S.D., R.C., F.B. and S.V. contributed to the development of the surveys; R.C., F.B. and S.V. conducted the analyses; S.V. wrote the paper; all authors critically revised draft versions of the manuscript and approved the final version. Ethics of human subject participation: The survey was approved by the Human Ethics Committee of Ghent University Hospital.






