The most obvious role of the immune system is to protect the individual from the harmful effects of pathogenic organisms they encounter, which can include bacteria, viruses, fungi and parasites. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in late 2019. Although human subjects have been previously exposed to many coronaviruses, SARS-CoV-2 was new to the human immune system. As a result, there was no pre-existing immunity against it, perhaps explaining why the virus spread so rapidly and caused such severe illness; this illness is called coronavirus disease discovered in 2019 or COVID-19. The extent of the health, societal and economic consequences that occurred due to the presence of SARS-CoV-2 and the severity of COVID-19 has focused attention on the devastation infectious illness can cause and on the importance of having a well-functioning immune system. The immune system can be weakened through disease, use of certain medications and several aspects of poor lifestyle as well as with ageing. It has been known for decades that inadequate nutrition impairs immunity(Reference Scrimshaw and SanGiovanni1–Reference Calder5) and during the SARS-CoV-2 pandemic, nutrition emerged as a potentially important factor influencing infection with the virus and severity of the resulting disease(Reference Calder5–Reference Calder, Carr and Gombart7). This review will provide an overview of the immune system and then describe the effects of frailty, obesity, selected micronutrients, long-chain n-3 fatty acids and the gut microbiota on immunity and susceptibility to infection including data from the SARS-CoV-2 pandemic where relevant. Some text is reused in modified form from a previous publication(Reference Calder6).
Overview of the immune system
The central role of the immune system is to protect against pathogenic bacteria, viruses, fungi and parasites that the individual is exposed to. It is clear that a weakened immune system places the individual at risk of becoming infected and of infections being more severe, even fatal. The immune system also has other important roles. One of these is to assure tolerance to environmental exposures that are non-threatening (e.g. harmless bacteria and components of food) and to the individual itself. A breakdown in such tolerance can lead to disease (e.g. food allergy in the case of loss of tolerance to food and autoimmunity in the case of loss of tolerance to self). In addition, the immune system clears dead and dying host cells and cellular debris, plays a role in surveillance against cancerous cells and tumours and is involved in wound healing. It has now emerged that the immune system also plays a role in whole-body metabolic homoeostasis(Reference Zmora, Bashiardes and Levy8). For example, cytokines such as TNF and IL-6 released during the inflammatory response induce insulin resistance in classic metabolic organs such as skeletal muscle and adipose tissue, perhaps as a strategy to divert energy-yielding substrates to the immune system during infection(Reference Grimble, Calder and Caballero9). When considering the wide range of roles for the immune system, it is clear that strategies to support the immune system and to ensure that it acts at the right time, in the right place and in the right context are vitally important to human health and wellbeing.
The four functional features of the immune system are:
(1) To act as a barrier to prevent entry of pathogens and other harmful environmental exposures. The skin and the mucosal lining of the gastrointestinal (GI), respiratory and genitourinary tracts are obvious barriers to entry. There are also antibodies and antimicrobial proteins in secretions such as saliva and tears, while the acid pH of the stomach can kill many bacteria. Commensal organisms on the skin and within the GI tract could also be considered part of this immune barrier since they may act to prevent colonisation by pathogens.
(2) To recognise structures (e.g. on microbes or of microbial origin) and to identify the source of those structures as harmful or harmless. There are two general recognition/identification systems. The first is recognition of general structural features of microbes (or of damaged tissue), termed molecular patterns (hence microbe-associated molecular patterns and damage-associated molecular patterns), by so-called pattern recognition receptors. The second is recognition of antigens through the interaction of antigen-presenting cells with antigen-specific T lymphocytes.
(3) To eliminate organisms that have been identified as harmful. There are multiple cellular mechanisms to achieve this. Phagocytosis is the process of engulfing entire microbes, usually bacteria, and then digesting them intracellularly. Neutrophils, monocytes, macrophages and dendritic cells are the main phagocytes. Coating of microbes with antibodies makes phagocytosis more effective. Natural killer cells and cytotoxic T lymphocytes destroy target cells through causing formation of pores in the membrane that permit the transfer of granzymes that induce apoptosis of the target cell; typical targets for these cell types are virally infected host cells and cancer cells.
(4) To maintain immunological memory of encounters. This is achieved through generation of memory T and B lymphocytes during an immune response. Memory cells can be very long lived and allow for a faster and stronger immune response upon re-exposure to the initial triggering structure. The memory response is the basis of vaccination.
When considering these features, it is evident that the immune system is highly complex and sophisticated in its function and regulation. It includes many different cell types, many communicating molecules and multiple functional responses. These are generally classified into innate (sometimes called natural) and acquired (sometimes called adaptive) immunity as shown in Fig. 1. Innate immunity includes the barrier functions and also the inflammatory response and some cellular responses such as natural killer cell activity and phagocytosis. The innate immune response is induced rapidly upon infection or injury. Acquired immunity takes longer to be activated but is antigen specific. It involves T lymphocytes and B lymphocytes. There are multiple phenotypes of T lymphocytes, including helper T cells, cytotoxic T cells and regulatory T cells, each with a specialised role and a typical profile of production of cytokines. Helper T cells regulate the function of other cell types through production of cytokines; there are several subclasses of helper T cells each with different roles including in anti-bacterial and anti-viral defences (type-1 T helper cells) and in anti-parasite defences (type-2 T helper cells). Helper T cells regulate the activity of cytotoxic T cells and phagocytes and control which classes of antibodies are produced by B lymphocytes. Cytotoxic T lymphocytes kill target virally infected cells and tumour cells through induction of apoptosis. Regulatory T cells are important controllers of the activity of other cell types, as their name suggests. B lymphocytes mature into antibody-producing plasma cells. Antibodies are antigen-specific immunoglobulins and these can coat microbes neutralising them and targeting them for phagocytosis.
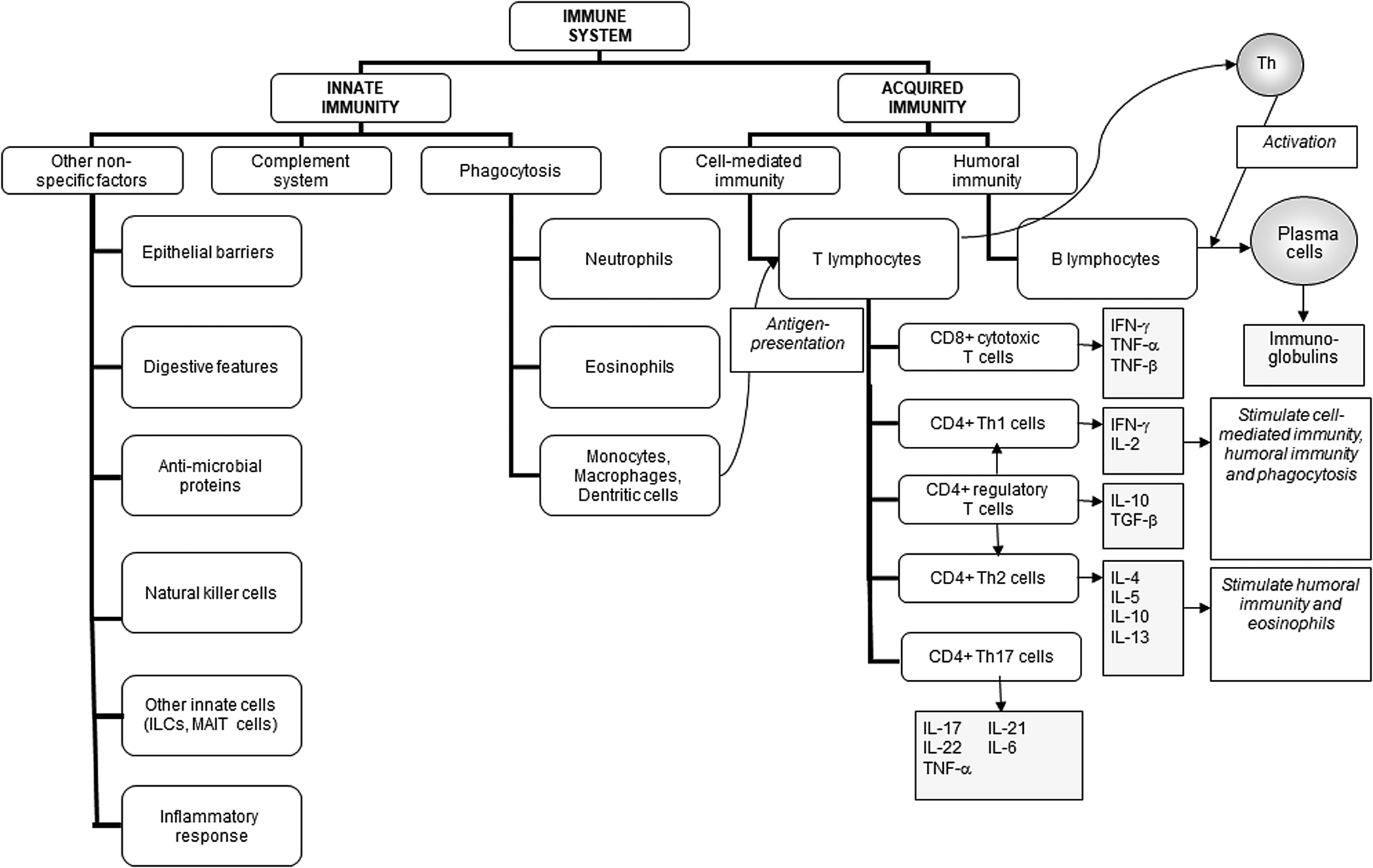
Fig. 1. Components of the immune system and their division into innate and acquired immunity. IFN, interferon; ILC, innate lymphoid cell; MAIT, mucosal associated invariant T; TGF, transforming growth factor; Th, T helper. Reproduced from(Reference Calder6) (CC BY licence).
Immune cells communicate with one another and with cells considered to be outside of the immune system. Some of this communication relates to transferring immunological information about the nature of the initial structure that was recognised (e.g. harmful v. harmless; bacterial origin v. viral origin) ensuring that the correct response is initiated. Other communication is regulatory in nature resulting in up- or down-regulation of specific cellular responses (e.g. phagocytosis, cytotoxic T lymphocyte activity, antibody production, metabolism). These two types of communication are interlinked and provide bidirectional interaction between innate and acquired immunity. For example, phagocytes, which are part of innate immunity, process and present antigens to T lymphocytes initiating the acquired immune response. As mentioned earlier, cytokines produced by T lymphocytes regulate the activity of phagocytes and natural killer cells while antibodies (produced by B lymphocytes) coat bacteria enhancing phagocytosis. Hence the immune response is a series of dynamic cellular interactions that are coordinated in such a way as to enable the most appropriate outcome which, in the case of exposure to a pathogen, is clearance of that pathogen with a retained immunological memory of the encounter. Fig. 2 shows a generalised depiction of the immune response to viral infection highlighting some of the key cellular interactions.
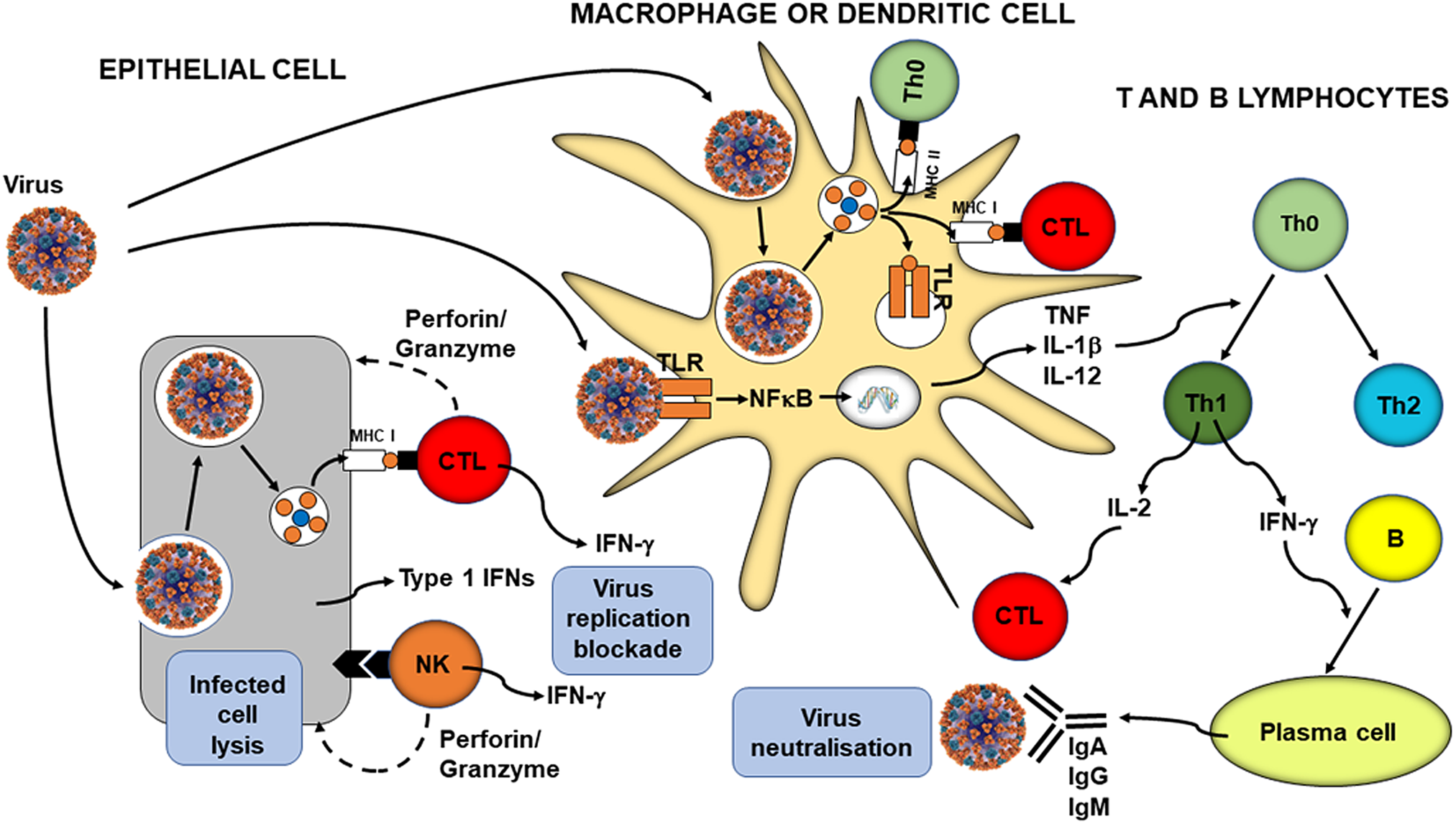
Fig. 2. Overview of anti-viral immunity. B, B cell; CTL, cytotoxic T lymphocyte; IFN, interferon; MHC, major histocompatibility class; NK, natural killer cell; Th, helper T cell; TLR, toll-like receptor. Reproduced from(Reference Calder5) (CC BY NC licence).
All immune cells are generated in the bone marrow and most mature there. The exception to this is T lymphocytes which mature in the thymus. Bone marrow and thymus are referred to as primary lymphoid organs. Immune cells circulate in the blood stream, where they are commonly referred to as leucocytes, and in lymph. However, most immune cell interactions occur in secondary lymphoid organs where the cells can come into close contact with one another. Secondary lymphoid organs include the spleen and lymph nodes. Although most human research is conducted on immune cells isolated from blood, these reflect only the minority of immune cells in the human body. It is estimated that about 70 % of immune cells in human subjects are associated with the wall of the GI tract in structures collectively referred to as the gut-associated lymphoid tissue (GALT)(Reference Mowat10). The GALT is designed to interact with the gut luminal contents and to provide a means of communication between these and the host immune system. There are discrete structures in the GALT such as Peyer's patches and immune cells move between these and other immune compartments such as lymph nodes, carrying and sharing immunological signals, including antigens. The importance of the GALT is to assess the luminal contents in order to make immunological decisions and respond accordingly (e.g. active response for defence purposes against pathogens or tolerogenic response to harmless organisms or food components)(Reference Mowat10). It is now recognised that there is movement of immune cells between the GALT and other mucosal surfaces such as the lungs (i.e. there is a gut–lung immune axis)(Reference Ma, Wang and Wang11) meaning that immunological information gathered at the gut level can be used elsewhere.
The immune system changes in ageing and this is exaggerated by frailty
Immune competence can decrease with age; this has been termed immunosenescence(Reference Pawelec, Larbi and Derhovanessian12,Reference Agarwal and Busse13) . There are multiple contributors to immunosenescence including decline in components of both innate and acquired immunity. These include:
(1) decreased output of immune cells from bone marrow;
(2) thymic involution with decreased production of naïve T lymphocytes, meaning decreased capacity to respond to newly encountered antigens;
(3) fewer T lymphocytes in the bloodstream;
(4) an altered balance of naive to memory T lymphocytes in the bloodstream (fewer naïve and more memory cells) but many of the memory T cells are senescent and do not respond well, meaning decreased capacity to respond to previously encountered antigens;
(5) decreased antigen presentation activity by dendritic cells;
(6) decreased phagocytosis, respiratory burst and bacterial killing by neutrophils;
(7) decreased cytotoxicity of natural killer cells and cytotoxic T lymphocytes towards virally infected and tumour cells;
(8) decreased ability of T lymphocytes to proliferate and to produce important cytokines such as IL-2 and interferon-γ;
(9) altered antibody production by B lymphocytes.
Hence, older people can show a broad range of immune impairments, making them more susceptible to infections(Reference Yoshikawa14). The increased susceptibility of older people to SARS-CoV-2 infection and to severe outcome from COVID-19 including greater likelihood of hospitalisation, intensive care unit admission, mechanical ventilation and death is well described(Reference Bonanad, García-Blas and Tarazona-Santabalbina15,Reference Zheng, Peng and Xu16) . Immunosenescence also impairs responses to vaccination, which is well known for the routine seasonal influenza vaccine(Reference Goodwin, Viboud and Simonsen17,Reference Pera, Campos and López18) and there is evidence of poorer responses to COVID-19 vaccines in older compared with younger adults(Reference Müller, Andrée and Moskorz19) (Fig. 3). Of course, not all older people show immune impairments, so it is important to identify those factors that make these more or less likely to occur. Nutrition may be important in this regard: immune decline is less in older people with better micronutrient intake or status(Reference Lesourd20). Furthermore, amongst older people, undernutrition promotes immune decline and frailty results in significant immune impairments. Yao et al.(Reference Yao, Hamilton and Weng21) reported that responses to all three strains within a seasonal influenza vaccine (responses measured as anti-vaccine antibody titres) were much lower in frail compared with non-frail older (72–95 years of age) people; responses of the pre-frail were intermediate. During a post-vaccination follow-up period, 50 % of the frail older people developed influenza-like illness and 30 % developed confirmed influenza; figures in the non-frail group were 10 and 5 %, respectively, and again the pre-frail were intermediate between the frail and non-frail groups(Reference Yao, Hamilton and Weng21). That immune impairments seen with frailty are of clinical significance comes from observations that less well-nourished hospitalised older people had a greater risk of infections than those who were better nourished(Reference Schneider, Veyres and Pivot22,Reference Paillaud, Herbaud and Caillet23) . Frailty is associated with poorer outcome from COVID-19 amongst older people(Reference Maltese, Corsonello and Di Rosa24), as confirmed in the meta-analysis of Zhang et al.(Reference Zhang, Jiao and Cao25) (Fig. 4).
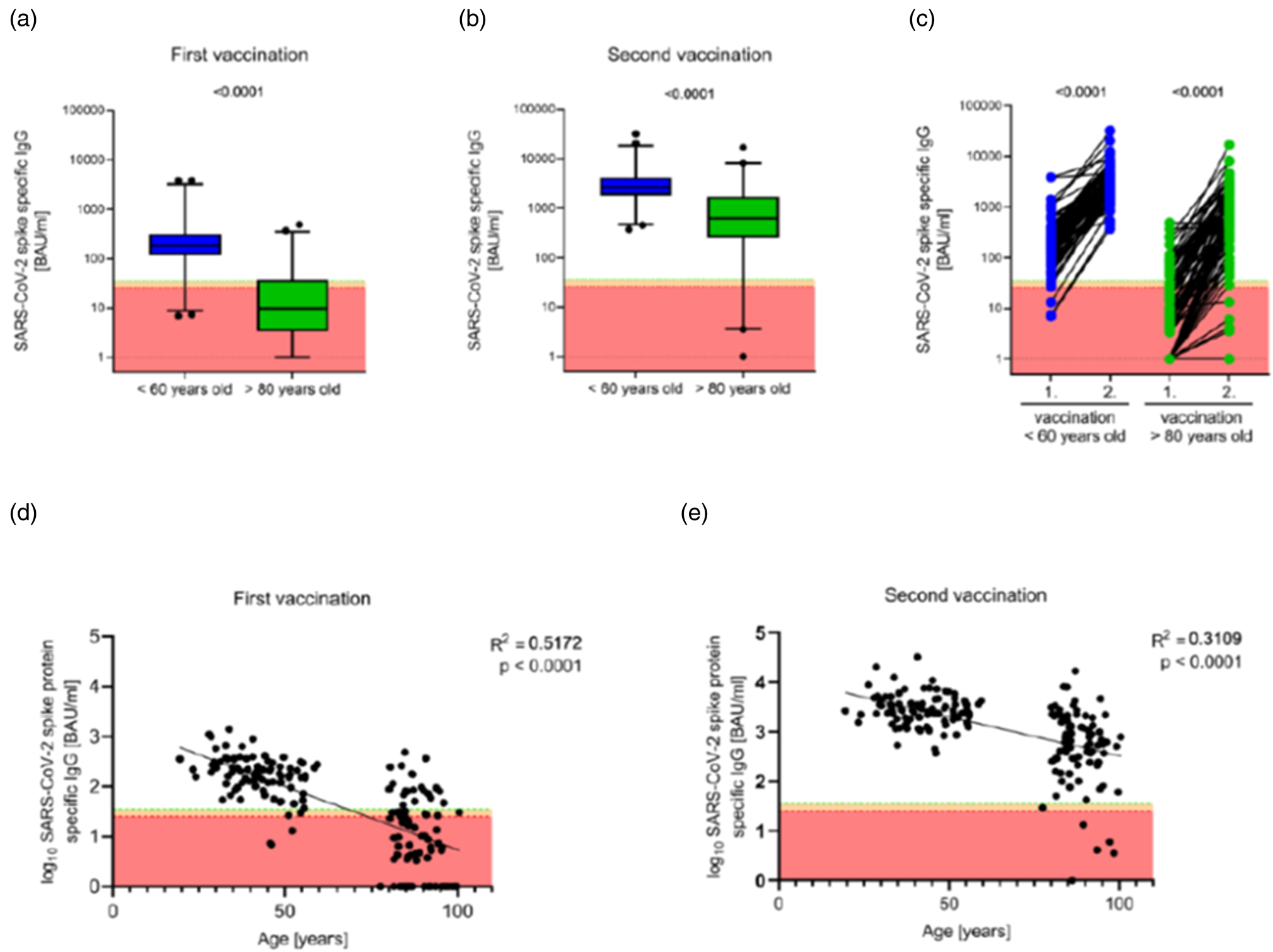
Fig. 3. Anti-SARS-CoV-2 spike protein-specific IgG titres following vaccination of younger and older adults with the Pfizer coronavirus disease 2019 vaccine. (A, B) Antibody titres 17–19 d after the first (A) and second (B) vaccination. Boxes span the interquartile range; the line within each box denotes the median and whiskers indicate the 2⋅5 and 97⋅5 percentile values. (C) Pairwise comparisons of antibody titres between the first and second vaccination within the two age groups are shown. (D, E) Linear correlations between participant's age and antibody titre after first (D) and second (E) vaccination. BAU, binding antibody units; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2. Reproduced from(Reference Müller, Andrée and Moskorz19), with permission from Oxford University Press.
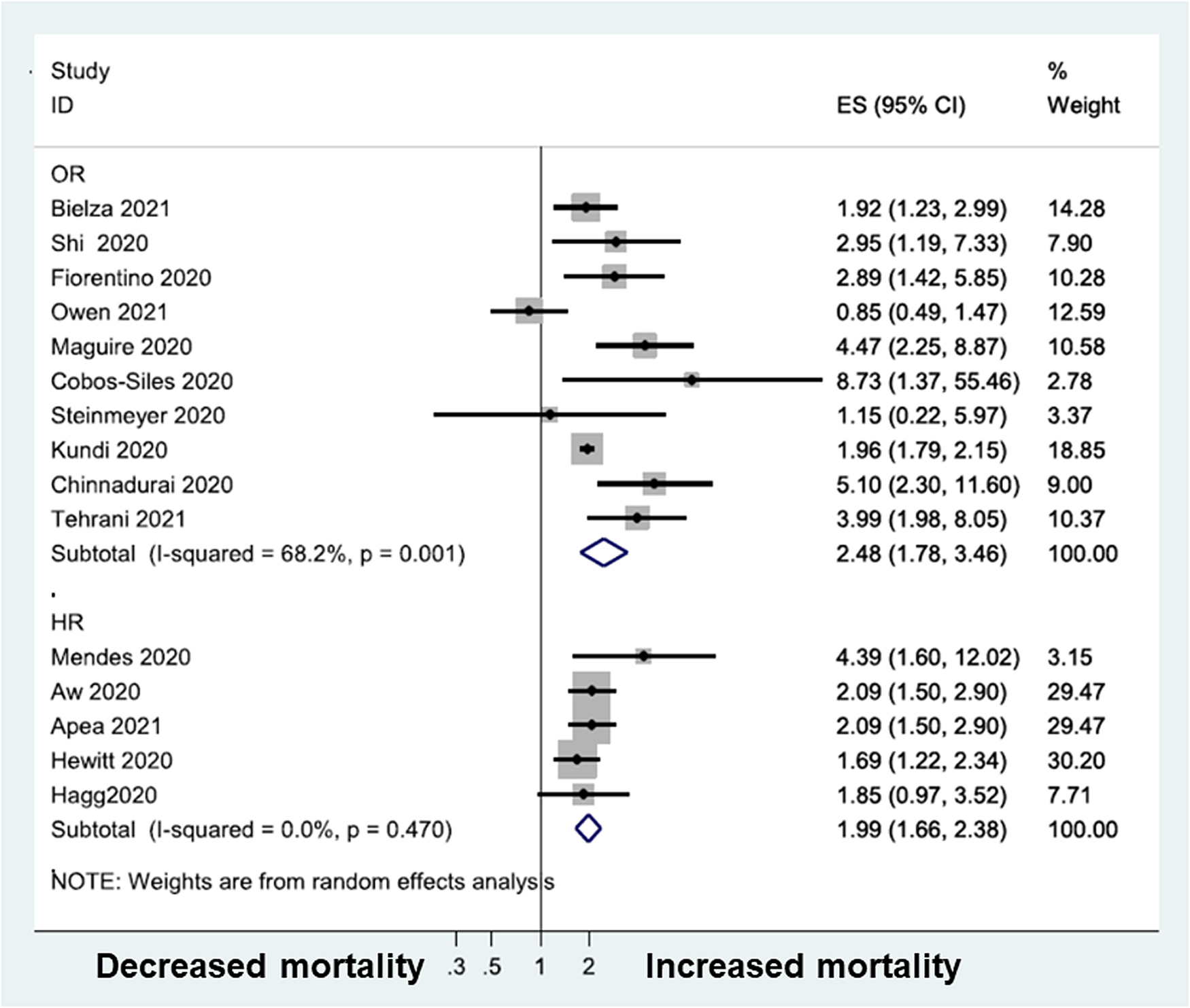
Fig. 4. Meta-analysis of the association of frailty with mortality amongst patients with COVID-19. Non-frail is defined as the reference group. COVID-19, coronavirus disease discovered in 2019; ES, effect size; HR, hazard ratio; OR, odds ratio. Reproduced from(Reference Zhang, Jiao and Cao25) (CC BY NC SA licence).
The immune system changes in those living with obesity
Immune competence can be diminished with obesity(Reference Milner and Beck26), with impairments in the activity of natural killer cells, helper and cytotoxic T lymphocytes, and B lymphocytes and decreased production of antibodies and the cytokine interferon-γ. This means that, compared with healthy weight individuals, those living with obesity have increased susceptibility to a range of infections(Reference Huttunen and Syrjänen27). During the 2009 H1N1 influenza A virus pandemic, those living with obesity showed delayed and weakened anti-viral responses to infection and showed poorer recovery from disease compared with healthy weight individuals(Reference Honce and Schultz-Cherry28). Vaccinated individuals living with obesity had twice the risk of influenza or influenza-like illness than healthy weight individuals, indicating poorer protection from vaccination in those with obesity(Reference Neidich, Green and Rebeles29). Sheridan et al.(Reference Sheridan, Paich and Handy30) investigated the responses of immune cells taken from the blood of healthy weight individuals and those with overweight or obesity to the influenza vaccine in vitro. Exposure of blood immune cells to the vaccine increased the number of activated cytotoxic T cells, the number of granzyme-expressing cytotoxic T cells and the number of interferon-γ-producing cytotoxic T cells, all key components of anti-viral immunity. However, the responses of cells from individuals living with obesity were reduced by 40 %, almost 60 and 65 %, respectively. Cells from individuals with overweight showed responses intermediate between those from healthy weight individuals and those living with obesity. Similar findings for the response of blood cells to the pandemic H1N1 influenza A virus were reported by Paich et al.(Reference Paich, Sheridan and Handy31). Thus, obesity is linked to multiple immune impairments, including to responses involved in protection against viruses.
There are multiple reports that adults living with obesity were more susceptible to severe COVID-19 and to mortality from COVID-19 than healthy weight adults and there are several meta-analyses of such studies. One systematic review and meta-analysis of twenty-two studies from seven countries in North America, Europe and Asia, reported that obesity is associated with an increased likelihood of more severe COVID-19 symptoms, requiring hospitalisation, being admitted to an intensive care unit, needing invasive mechanical ventilation and developing acute respiratory distress syndrome(Reference Zhang, Lewis and Moley32) (Figs 5 and 6). The studies included in this systematic review dichotomised individuals as living with obesity or not, but large datasets from the UK and the USA report that there is a continuous positive relationship between BMI (above about 25 kg/m2) and adverse outcomes from COVID-19(Reference Gao, Piernas and Astbury33,Reference Kompaniyets, Goodman and Belay34) .
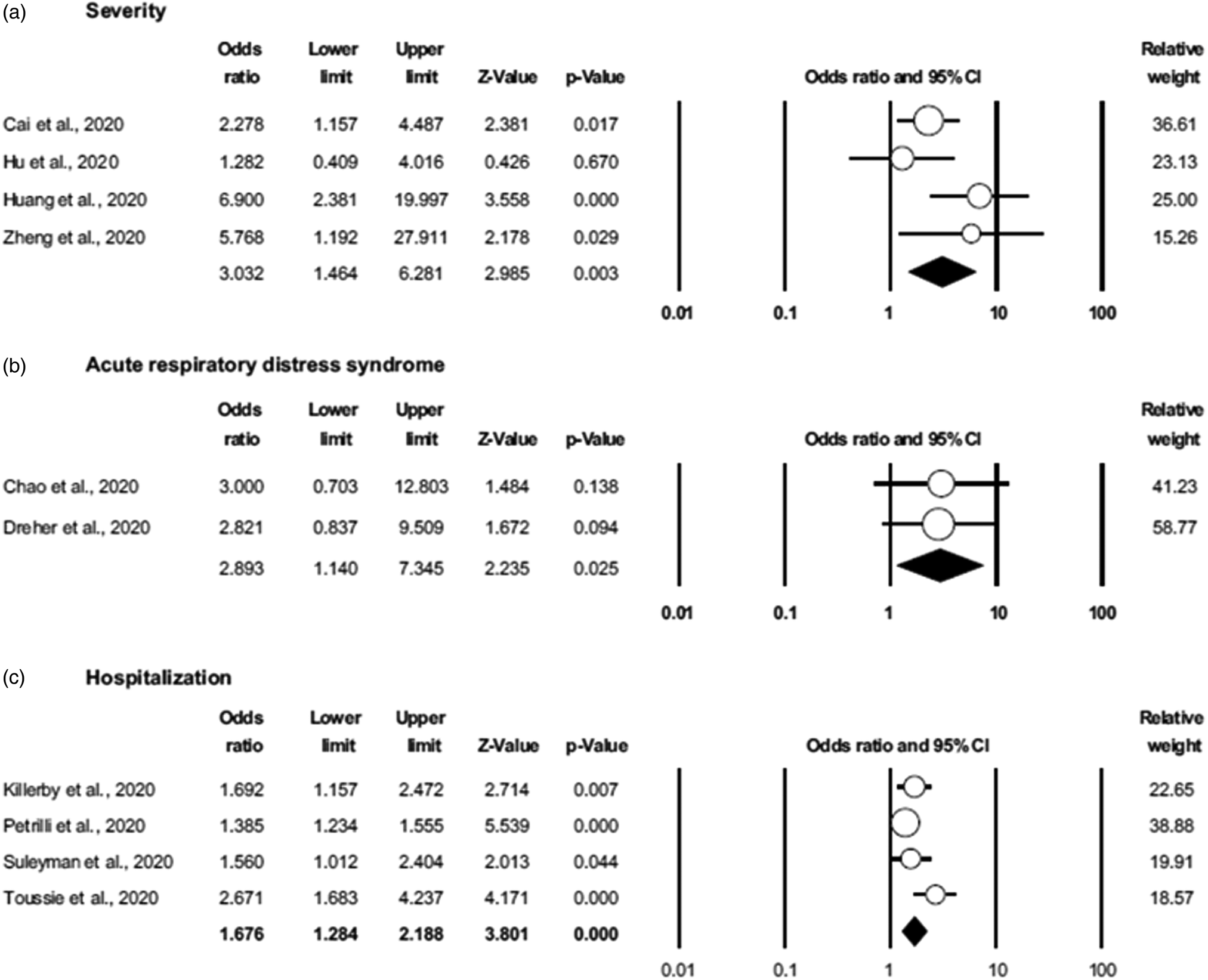
Fig. 5. Association of obesity with severe COVID-19 outcomes: (A) severe COVID-19; (B) developing acute respiratory distress syndrome and (C) being hospitalised. Non-obese is defined as the reference group. COVID-19, coronavirus disease discovered in 2019. Reproduced from(Reference Zhang, Lewis and Moley32) (CC BY licence).
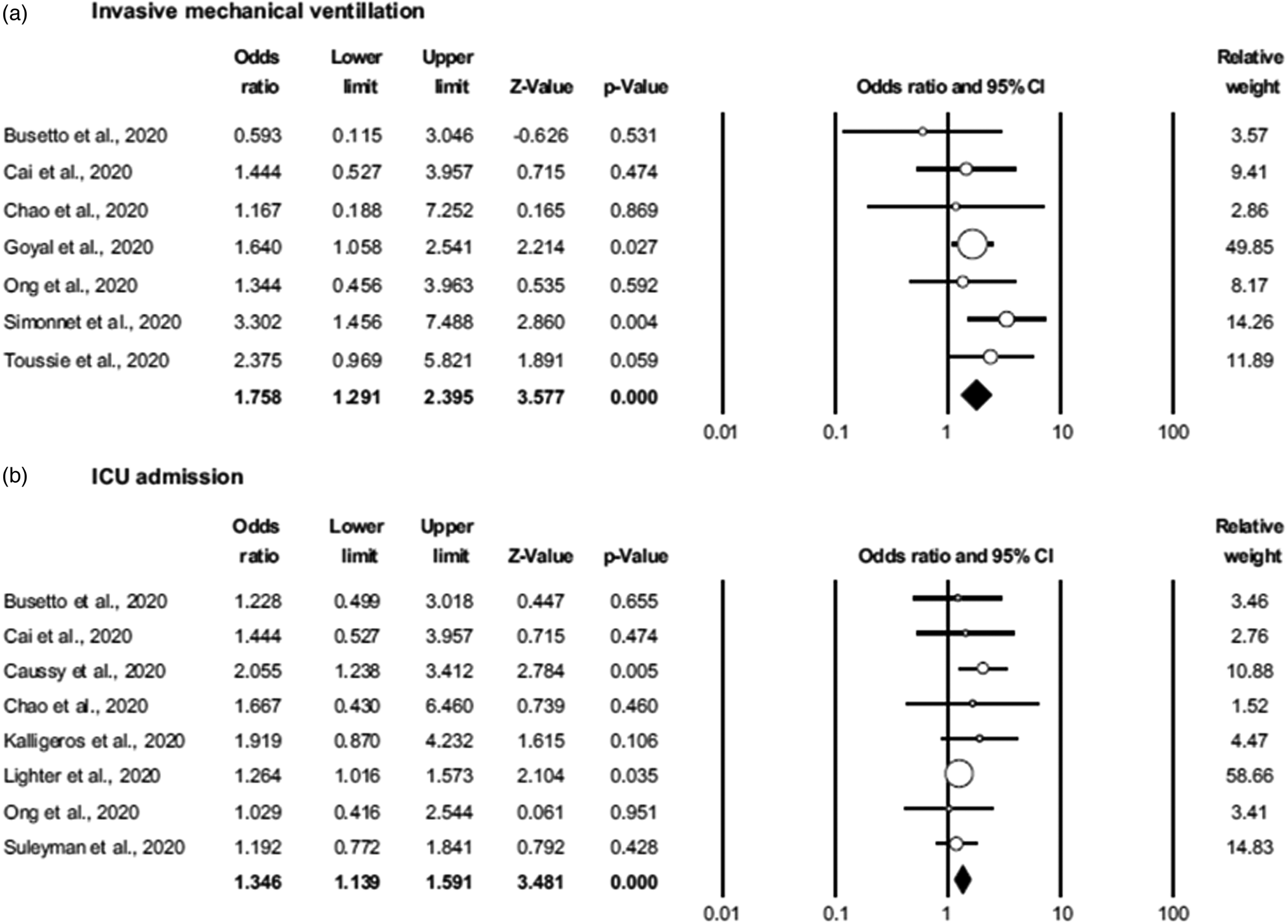
Fig. 6. Association of obesity with severe COVID-19 outcomes (A) requiring invasive mechanical ventilation; (B) admission to the intensive care unit in the setting of COVID-19. Non-obese is defined as the reference group. COVID-19, coronavirus disease discovered in 2019; ICU, intensive care unit. Reproduced from(Reference Zhang, Lewis and Moley32) (CC BY licence).
Many nutrients are important in supporting the immune system to function
It has been known for decades that poor nutrition (generalised undernutrition, micronutrient deficiency) is associated with immune impairments, increased susceptibility to infection and poor outcome from infection, with especially severe consequences in infants and children(Reference Scrimshaw and SanGiovanni1–Reference Calder and Jackson3). As described elsewhere(Reference Calder4) nutrition plays multiple roles in supporting the immune system since the diet provides:
(1) fuels for the immune system to function;
(2) building blocks for the synthesis of RNA, DNA, proteins (antibodies, cytokines, receptors, acute phase proteins, etc.) and new cells;
(3) specific substrates for the production of immune-active metabolites (e.g. arginine as a substrate for nitric oxide);
(4) regulators of immune cell metabolism (e.g. vitamin A, zinc);
(5) nutrients with specific antibacterial or anti-viral functions (e.g. vitamin D, zinc);
(6) regulators that protect the host from the oxidative and inflammatory stress imposed by the immune response (e.g. vitamin C, vitamin E, zinc, selenium, long-chain n-3 fatty acids and many plant polyphenols);
(7) substrates for the intestinal microbiota which in turn modulates the immune system (see later section).
Beyond generalised undernutrition, the role of micronutrients in supporting the immune system has been widely studied, as reviewed elsewhere(Reference Gombart, Pierre and Maggini35–Reference Eggersdorfer, Berger and Calder37). Multiple micronutrients play multiple important roles in supporting multiple components of the immune response (Table 1), so it is no surprise that deficiency in one or more of these has adverse consequence for immunity and infection. The roles of vitamins A, C and D and zinc, copper and iron are well explored, but B vitamins, vitamins E and K, selenium, magnesium and others all have roles(Reference Calder4,Reference Calder5,Reference Calder, Carr and Gombart7,Reference Gombart, Pierre and Maggini35–Reference Eggersdorfer, Berger and Calder37) . With regards to SARS-CoV-2 infection and COVID-19 there has been much interest in micronutrients, mainly vitamin D and zinc, but also many others(Reference Calder5).
Table 1. Summary of the effects of various micronutrients on different aspects of immunity
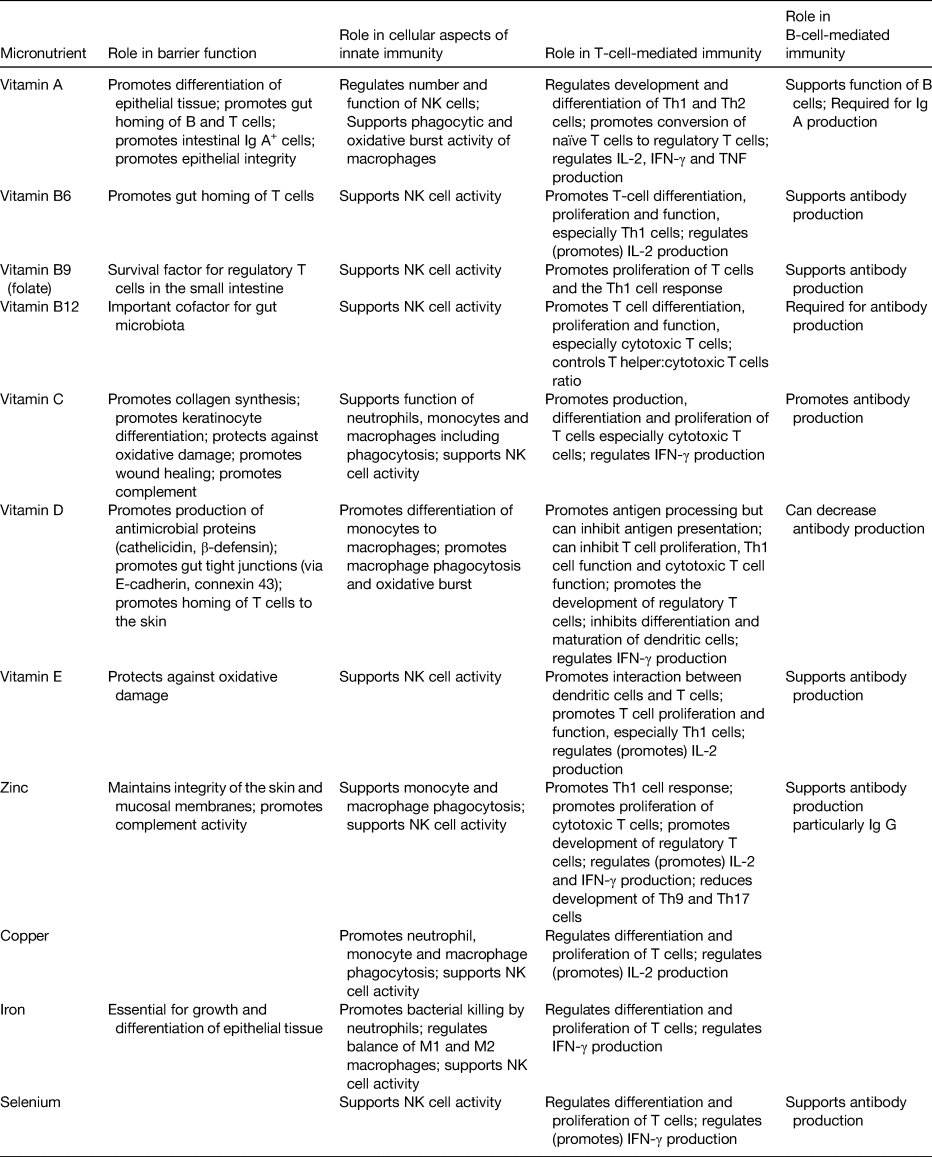
IFN, interferon; NK, natural killer; Th, T helper.
Reproduced from(Reference Calder6) (CC BY licence).
Vitamin D has pleiotropic actions within the immune system and supports the activity of several cell types(Reference Prietl, Treiber and Pieber38,Reference Chirumbolo, Bjørklund and Sboarina39) . Some immune cell types, including dendritic cells and macrophages, can produce the active form of vitamin D suggesting it is important to immunity. Vitamin D promotes the production of antimicrobial proteins such as cathelicidin. Vitamin D deficiency impairs the response to the seasonal influenza vaccine(Reference Lee, Lin and Lei40) and meta-analyses of randomised controlled trials of vitamin D supplementation report reduced incidence of respiratory tract infections(Reference Martineau, Jolliffe and Hooper41,Reference Jolliffe, Camargo and Sluyter42) . Multiple studies report an association between low vitamin D status and increased susceptibility to, and severity of, COVID-19(Reference Merzon, Tworowski and Gorohovski43–Reference Kaufman, Niles and Kroll45) while data from the UK BioBank showed that using vitamin D supplements was associated with decreased risk of a positive test for SARS-CoV-2 after controlling for multiple confounders(Reference Ma, Zhou and Heianza46). Many meta-analyses report that vitamin D deficiency (or low vitamin D status) is associated with an increased risk of severe COVID-19, hospitalisation with COVID-19 and mortality from COVID-19(Reference Pereira, Dantas Damascena and Galvão Azevedo47). A report from an Italian residential care home showed that a bolus of vitamin D reduced mortality from COVID-19(Reference Cangiano, Fatti and Danesi48) and a number of trials with different study designs suggest that vitamin D can be used to treat COVID-19(Reference Entrenas Castillo, Entrenas Costa and Vaquero Barrios49–Reference Ling, Broad and Murphy51). However, while some meta-analyses of such trials report that vitamin D supplementation can reduce COVID-19 severity as determined by hospitalisation, need for intensive care unit admission or mortality(Reference Kümmel, Krumbein and Fragkou52,Reference Pal, Banerjee and Bhadada53) other meta-analyses report no significant effect on such outcomes(Reference Beran, Mhanna and Srour54). Reasons for these different findings relate to the exact studies included and the extent of adjustment for confounders. Consequently, it is uncertain whether vitamin D can be used to treat people with COVID-19, although there are some supportive data for this.
Zinc supports the activity of many cells of the immune system(Reference Wessels, Maywald and Rink55), helps to control oxidative stress and inflammation and has specific anti-viral actions(Reference Read, Obeid and Ahlenstiel56) including inhibiting the replication of coronaviruses(Reference te Velthuis, van den Worm and Sims57). Zinc supplementation improves some markers of immunity especially in older people or those with low zinc intake(Reference Barnett, Dao and Hamer58) and improves vaccination responses(Reference Karlsen, Sommerfelt and Klomstad59). Meta-analyses of randomised controlled trials of zinc supplementation report reduced incidence of diarrhoeal and respiratory tract infections(Reference Aggarwal, Sentz and Miller60–Reference Hunter, Arentz and Goldenberg64). Multiple studies report an association between low zinc status and increased susceptibility to and severity of COVID-19(Reference Heller, Sun and Hackler65–Reference Lahaye, Parant and Haesebaert68). Some studies have reported that zinc supplementation in patients hospitalised with COVID-19 reduces risk of poor outcome including mortality(Reference Carlucci, Ahuja and Petrilli69,Reference Frontera, Rahimian and Yaghi70) and some meta-analyses support that zinc supplementation reduces mortality(Reference Olczak-Pruc, Szarpak and Navolokina71,Reference Tabatabaeizadeh72) . However, other meta-analyses report no effect of zinc on mortality and other clinically relevant outcomes(Reference Beran, Mhanna and Srour54). Thus, it is currently uncertain whether zinc can be used to treat people with COVID-19, although there are some supportive data for this.
In contrast to the large literature on vitamin D and zinc that has emerged during the pandemic, there has been less research on selenium. Nevertheless, selenium may have important roles in supporting the immune system in general(Reference Avery and Hoffmann73) and in promoting anti-viral immunity in particular(Reference Hiffler and Rakotoambinina74). Selenium supports the activity of many cells of the immune system and helps to control oxidative stress and inflammation. Extensive research in mice has shown that selenium deficiency impairs immune responses, increases susceptibility to viral infection, permits viruses (including influenza viruses) to mutate and allows normally weak viruses to become more virulent(Reference Beck, Handy and Levander75). Some studies show that selenium supplementation improves some markers of immunity especially in older people or those with low selenium intake; for example a supplementation study conducted in UK adults with marginal selenium status showed that selenium improved ex vivo anti-viral immune responses, promoted viral clearance and decreased viral mutation(Reference Broome, McArdle and Kyle76), although other studies have shown only modest effects of selenium supplements on immunity(Reference Ivory, Prieto and Spinks77). A recent meta-analysis of selenium and immune function identified that selenium supplementation increased natural killer cell activity and concluded ‘although some of the data suggested beneficial effects of selenium supplementation on immune function, the overall picture appears to be inconsistent and heterogeneous due to differences in trial duration and interventions, plus evidence of null and even detrimental effects’(Reference Filippini, Fairweather-Tait and Vinceti78). Several studies report an association between low selenium status and increased susceptibility to and severity of COVID-19(Reference Heller, Sun and Hackler65,Reference Moghaddam, Heller and Sun79,Reference Im, Je and Baek80) . There are no randomised controlled trials of selenium as a stand-alone nutrient in patients with COVID-19 reporting on clinical outcomes. Thus, it is currently uncertain whether selenium can be used to treat people with COVID-19.
Vitamin C supports the activity of some components of innate and adaptive immunity(Reference Carr and Maggini81,Reference Manning, Mitchell and Appadurai82) , as well as the physical barriers that limit entry to pathogens(Reference Maggini, Wintergerst and Beveridge83) and helps to control oxidative stress and inflammation. Vitamin C supplementation improves some markers of immunity especially in older people(Reference Jacob, Kelley and Pianalto84,Reference Chuangchot, Boonthongkaew and Phoksawat85) and a meta-analysis(Reference Hemilä and Chalker86) suggests that those under physical or physiological stress may show reduced incidence and duration of the common cold with vitamin C supplementation, especially if ‘high’ doses are used. Several studies report an association between low vitamin C status and increased susceptibility to, and severity of, COVID-19(Reference Arvinte, Singh and Marik87,Reference Chiscano-Camón, Ruiz-Rodriguez and Ruiz-Sanmartin88) . Some studies report that high dose vitamin C may reduce the risk of poor outcome in patients hospitalised with COVID-19(Reference Zhao, Ling and Li89,Reference Holford, Carr and Jovic90) and some meta-analyses support that vitamin C reduces mortality(Reference Olczak-Pruc, Swieczkowski and Ladny91). However other meta-analyses report no effect of vitamin C given orally or intravenously on mortality and other clinically relevant outcomes in patients with COVID-19(Reference Beran, Mhanna and Srour54,Reference Rawat, Roy and Maitra92–Reference Ao, Li and Yuan94) . Thus, it is currently uncertain whether vitamin C can be used to treat people with COVID-19.
Vitamin E supports the activity of some components of innate and adaptive immunity(Reference Meydani, Han and Wu95,Reference Lee and Han96) and helps to control oxidative stress and inflammation. Vitamin E supplementation improves some markers of immunity especially in older people(Reference de la Fuente, Hernanz and Guayerbas97,Reference Meydani, Barklund and Liu98) and enhances the response to some vaccines(Reference Meydani, Meydani and Blumberg99). Vitamin E may reduce the risk of upper respiratory tract infections(Reference Meydani, Leka and Fine100), although not all studies show this(Reference Graat, Schouten and Kok101). Studies report lower vitamin E status in those hospitalised with COVID-19 than in healthy controls(Reference Žarković, Jastrząb and Jarocka-Karpowicz102) and that vitamin E status is lower in those with more severe disease(Reference Neves, Pott-Junior and Yamashita103). There are no randomised controlled trials of vitamin E as a stand-alone nutrient in patients with COVID-19 reporting on clinical outcomes. Thus, it is currently uncertain whether vitamin E can be used to treat people with COVID-19.
The long-chain n-3 fatty acids EPA and DHA are anti-inflammatory(Reference Calder104) and are precursors to so-called specialised pro-resolving mediators(Reference Chiang and Serhan105). Thus, EPA and DHA could have a role in controlling the adverse inflammation associated with severe COVID-19 that is referred to as a ‘cytokine storm’. Furthermore, EPA and DHA modulate immune function, although findings in human trials have been inconsistent(Reference Calder104). A study in school children reported that increased daily intake of EPA and DHA decreased the risk of infection (mainly upper respiratory tract) and shortened the duration of illness(Reference Thienprasert, Samuhaseneetoo and Popplestone106). Hence there has been some interest in these n-3 fatty acids and COVID-19. Data from the UK BioBank showed that the habitual use of fish oil supplements, a source of EPA and DHA, was associated with a lower risk of hospitalisation with COVID-19 and COVID-19 mortality(Reference Ma, Zhang and Zeng107) and that higher DHA status was associated with a lower risk of infection with SARS-CoV-2, hospitalisation with COVID-19 and mortality from COVID-19(Reference Julkunen, Cichonska and Slagboom108–Reference Harris, Tintle and Perinkulam Sathyanarayanan110). Small studies reported that lower n-3 status was associated with more severe COVID-19(Reference Ramírez-Santana, Zapata Barra and Ñunque González111,Reference Zapata B, Müller and Vásquez112) and that hospitalised patients with a high n-3 status were less likely to die than those with lower n-3 status(Reference Asher, Tintle and Myers113). There are few trials of n-3 fatty acids in patients with COVID-19. One trial randomised critically ill patients with COVID-19 to a high-protein enteral formula providing EPA and DHA or to a control group that received the formula without added n-3 fatty acids; the n-3 group had better indicators of some, but not all, physiological functions at day 14 and had better survival at 1 month(Reference Doaei, Gholami and Rastgoo114). Because of the limited number of studies, it is currently uncertain whether long-chain n-3 fatty acids can be used to treat people with COVID-19, although there are some supportive data for this.
The gut microbiota is an important determinant of immunity
Commensal bacteria within the GI tract play a role in host immune defence creating a barrier against colonisation by pathogens and through the production of lactic acid and antimicrobial proteins which can directly inhibit the growth of pathogens. Commensal organisms also interact with the host's gut epithelium and GALT, through chemicals released from the bacteria or through direct cell-to-cell contact. Conversely the host immune system interacts with the gut microbiota through multiple mechanisms(Reference Ahern and Maloy115,Reference Samuelson, Welsh and Shellito116) . Hence, the interaction between the gut microbiota and the host immune system is bidirectional. Gut dysbiosis may result from inability to sustain commensals (e.g. through use of antibiotics or through poor lifestyle) which in turn would alter signals to the host immune system. Conversely, an ineffective host immune response may not be able to prevent pathogenic organisms from taking hold resulting in dysbiosis. Probiotic organisms, particularly some lactobacilli and bifidobacteria, or prebiotics that promote the growth of such organisms, are proposed as a strategy to support host immunity. Indeed, a large number of studies have examined the influence of various probiotic organisms, either alone or in combination, on immune function and infection in human subjects(Reference Lomax and Calder117). Some probiotic organisms appear to enhance innate immunity (particularly phagocytosis and natural killer cell activity) but they seem to have a less pronounced effect on acquired immunity(Reference Lomax and Calder117). Nevertheless, there are studies reporting improved responses to vaccination, especially with the seasonal influenza vaccine, in individuals taking probiotics as reviewed elsewhere(Reference Maidens, Childs and Przemska118). Systematic reviews and meta-analyses confirm that probiotics (or prebiotics) enhance the antibody response to seasonal influenza vaccination in adults(Reference Lei, Shih and Liu119,Reference Yeh, Shih and Liu120) . Systematic reviews and meta-analyses report that some probiotics can reduce the risk or duration of diarrhoea, including antibiotic-associated diarrhoea and Clostridium difficile-associated diarrhoea and reduce the incidence of, and improve outcomes in, respiratory infections (see(Reference Calder5) for references). Gut dysbiosis has been reported in patients with COVID-19(Reference Zuo, Zhang and Lui121), although the direction of causality is uncertain in such studies. Nevertheless, the evidence base about probiotics has created some enthusiasm for their role in the treatment of COVID-19. In a study in Italy, d'Ettorre et al.(Reference d'Ettorre, Ceccarelli and Marazzato122) treated patients hospitalised with COVID-19 with a cocktail of drugs and antibiotics or the same plus oral probiotics (five lactobacilli plus two bifidobacteria plus Streptococcus thermophilus): they found better resolution of diarrhoea and of other disease symptoms including respiratory disease in the group receiving probiotics. In a study in Mexicans with COVID-19 but not hospitalised, probiotics (three Lactiplantibacillus plantarum strains plus Pediococcus acidilactici) increased SARS-CoV-2-specific Ig M and G and decreased nasopharyngeal viral load, lung infiltrates and duration of both GI and non-GI symptoms, compared to placebo(Reference Gutiérrez-Castrellón, Gandara-Martí and Abreu123). In a Russian study treating patients hospitalised with COVID-19 with a mix of multiple lactobacilli and bifidobacteria decreased the risk of hospital-acquired diarrhoea but had no effect on other outcomes(Reference Ivashkin, Fomin and Moiseev124). Thus, overall findings with probiotic intervention in patients with COVID-19 are promising though somewhat inconsistent. This could relate to the actual probiotic strains being used and/or to the different characteristics and disease severity of the patients studied.
Is there an immune supporting diet?
The foregoing discussion would suggest that a diet that provides a good intake of quality protein, micronutrients, other essential nutrients, plant polyphenols and fibre (to promote a diverse gut microbiota) without an excess of energy would be one that gives the best opportunity for the immune system to function well, although supplements of some important nutrients such as vitamin D might also be required. In this regard it is important to note the trial of Gibson et al.(Reference Gibson, Edgar and Neville125) that reported that older people who normally consumed ≤two portions of fruits and vegetables daily and were randomised to consume >five portions daily for 16 weeks had a higher antibody response to pneumococcus vaccination than seen in the control group who retained their diet of ≤two portions daily. There have been several studies examining the association between diet quality and COVID-19-related outcomes. Five such studies(Reference Hou, Su and Chao126–Reference Yue, Ma and Accorsi130) have been recently included in a meta-analysis examining the association of adherence to a high-quality dietary pattern on COVID-19 outcomes(Reference Rahmati, Fatemi and Yon131); these were three cohort and two cross-sectional studies involving a total of over 4 million individuals. Adherence to a high-quality diet was associated with a 28 % (95 % CI 19, 36) decrease in SARS-CoV-2 infection and a 62 % (95 % CI 25, 80) decrease in hospitalisation with COVID-19. Both a plant-based diet and the Mediterranean diet were associated with a lower risk of infection.
Conclusions
A key role for the immune system is providing host defence against pathogenic organisms that the individual encounters and a well-functioning immune system is required for effective defence against such organisms. Impaired immunity predisposes to infections and to more severe infections and weakens the response to vaccination. A range of nutrients, most obviously micronutrients, play important roles in supporting the immune system to function well. The immune system can decline in later life and this is exaggerated by frailty. The immune system is also weakened with obesity, generalised undernutrition and micronutrient deficiencies. These all result in increased susceptibility to infection. Weakened immunity is an under-recognised result of ageing and of frailty, obesity and poor nutrient intake. Findings obtained during the SARS-CoV-2 pandemic add weight to what was already known about the effects of ageing, frailty and obesity on immunity and susceptibility to infection. Multiple observational studies made during the SARS-CoV-2 pandemic also support previous findings that multiple micronutrients including vitamins C, D and E, zinc and selenium and long-chain n-3 fatty acids are important for immune health, but whether these nutrients can be used to treat those already with COVID-19, particularly if already hospitalised, is uncertain from current inconsistent or scant evidence. The gut microbiota has emerged as an important determinant of immunity with much supportive pre-SARS-CoV-2 pandemic data on probiotics and GI and respiratory infections. There is gut dysbiosis in patients with COVID-19 but the direction of causality for this is unclear. Nevertheless, studies with probiotics report clinical improvements in patients with COVID-19. There is a strong inverse association between adherence to a healthy diet and risk of SARS-CoV-2 infection and hospitalisation with COVID-19 which is consistent with the effects of individual nutrients and other dietary components. Looking forward, it seems obvious that addressing frailty and obesity will be important to reduce the burden of future pandemics. This is the major lesson from the study of nutrition and immunity that is relevant for the battle with SARS-CoV-2 and the disease it causes, COVID-19, and for ensuring the population is better prepared for future pandemics. Going beyond that, strategies addressing current nutritional inadequacies that are widespread in the population (e.g. micronutrient insufficiency) are needed to ensure better support of the immune system across the population. This is the second lesson from the SARS-CoV-2 pandemic and nutritional considerations need to be a core part of the approach to preventing infections(Reference Calder, Carr and Gombart7,Reference Calder, Ortega and Meydani132) , optimising vaccine responses(Reference Rayman and Calder133) and promoting recovery from infection(Reference Bradbury, Wilkinson and Schloss134). Even so, supplements may be necessary to achieve the required intakes of some of the key immune supporting nutrients such as vitamin D. Overall, the focus should be on immune support as a preventative strategy for infection.
Financial Support
None.
Conflict of Interest
P. C. C. has current research funding about nutrition and immunity from the Medical Research Council (grant MR/T001879/1), Bayer Consumer Care and Tate and Lyle; has received study materials from DSM and Tate & Lyle and acts as an advisor/consultant to BASF, DSM, Cargill, Danone/Nutricia, Nutrileads, Bayer Consumer Care and Haleon.
Authorship
The author had sole responsibility for all aspects of preparation of this paper.










