Overweight and obesity presents a major public health challenge to the current and future health of the population. The most recent Scottish Health Survey showed that 65 % of adults in Scotland were overweight and 27 % were obese. It is predicted that by 2030 over 40 % of adults will be obese( Reference Bromley, Dowling and Gray 1 ). Higher BMI is associated with an increased risk of morbidity and mortality from a range of conditions including hypertension, heart disease, stroke, type 2 diabetes and several cancers( 2 ). In 2011 it was predicted that there were 100 000 obese adults in Grampian, 55 170 of whom were on the register held though the Quality and Outcomes Framework system( Reference Pittendreigh 3 ).
To tackle this major public health problem, NHS Grampian sought to commission a feasibility study of a commercial weight management service for adults with a BMI of ≥30 kg/m2, to help them to achieve and maintain a healthier weight. The study was conducted in Aberdeen city centre and suburbs. Aberdeen is situated in the North East of Scotland. Of the 283 data zones in Aberdeen, nine are among the most deprived of all Scottish data zones( 4 ). Less than 8 % of the total city population lives in data zones representing the most deprived 20 % of the Scottish population( 4 ).
The present study explored the feasibility of a community pharmacy-based referral service to a commercial weight management service, Scottish Slimmers (SS). SS was founded in 1980 and has a proven record of enabling successful weight loss. It is a lifestyle-based, group weight-loss programme which offers weekly meetings at community venues, a nutritionally balanced eating plan and advice on physical activity, aiming to produce moderate weight loss( 5 ). We hypothesized that the provision of this signposting service through community pharmacies could increase access to this weight management service. Community pharmacies in Scotland are involved in a number of formal signposting initiatives like optometry referrals( 6 ), as well as out-of-hours services such as dental care included within the minor ailment service( 7 ). They can also refer patients to other social care providers, for example for child protection issues( 8 ).
The Scottish population regularly attends community pharmacies, with 85 % of the population in Scotland using pharmacies in Scotland within a year( Reference Porteous, Bond and Hannaford 9 ).
The purpose of the weight management signposting study was to assess the feasibility of community pharmacists providing a weight management signposting service. Specifically, we wanted to:
1. compare the uptake of a pharmacy-based signposting service;
2. compare retention rates of clients signposted through pharmacies;
3. compare the effect of different models of voucher provision on retention and weight;
4. explore the effect of a pharmacy-based signposting service on client weight;
5. explore clients’ opinions regarding the provision of the signposting service; and
6. explore pharmacy staff members’ experience of providing a pharmacy-based signposting service.
Methods
The feasibility study used a prospective cohort design and included qualitative interviews with clients and pharmacy personnel. SS collected weight and attendance data. The setting was community pharmacies in Aberdeen City, Scotland. The study was conducted between November 2013 and June 2014. Ethical approval was given by the College of Life Sciences and Medicine Ethics Review Board, University of Aberdeen.
Pharmacies
Using the local Health Board register, community pharmacies in Aberdeen City that were in close proximity (20 minutes’ walking distance) to SS classes were identified. To be eligible to participate, pharmacies were required to have a private consultation room. Each pharmacy was provided with promotional materials relating to the referral service. Pharmacies received a payment of £50 to participate as well as £5 per client recruited.
Client recruitment
Each pharmacy had a recruitment target of twenty clients. Inclusion criteria for clients were age ≥18 years and BMI≥30 kg/m2. Women who were pregnant, adults with eating disorders, or people attending community or commercial weight management groups in the previous three months were not eligible.
All members of pharmacy staff were trained to recruit clients. A researcher (J.I.) provided on-site training to the responsible pharmacist and available staff. The pharmacists then trained the remaining staff who were unavailable. Training involved the process for recruiting clients, measuring the clients’ BMI, voucher allocation and data collection.
Once trained, pharmacy staff approached potentially eligible clients if they: (i) purchased weight-loss products; (ii) asked for advice about weight loss; or (iii) enquired about the study as a result of promotional information displayed in the community pharmacies.
All clients who expressed an interest in participating were provided with an information sheet after discussion with a member of pharmacy staff regarding whether there was a suitable SS class they could attend. Potential participants had their weight and height measured to calculate their BMI. If their BMI was ≥30 kg/m2, the client was invited to participate. Clients were advised that if they had any concerns regarding their health they were to contact their general practitioner regarding their suitability to participate. Clients with a BMI of <30 kg/m2, thus not eligible for the present study, were advised of the nearest SS class.
Voucher allocation was initially randomized by client uptake to explore what effect, if any, this would have on class attendance, with the hypothesis that more frequent contact with the pharmacy might achieve more consistent class attendance. As such, consecutive clients were offered vouchers in one of three ways: (i) twelve vouchers provided at the recruitment visit; (ii) weekly vouchers issued every week for 12 weeks; or (iii) four vouchers issued on three occasions.
If clients were unable to collect vouchers on a weekly or monthly basis however, they were given all twelve vouchers at the recruitment visit. Voucher allocation was recorded in the client pharmacy log by pharmacy personnel. The original recruitment period was from April 2014 to July 2014. However, due to lower-than-anticipated recruitment from some pharmacies, the recruitment period was extended until the end of August 2014, with some pharmacies agreeing to recruit more than twenty clients (Fig. 1).
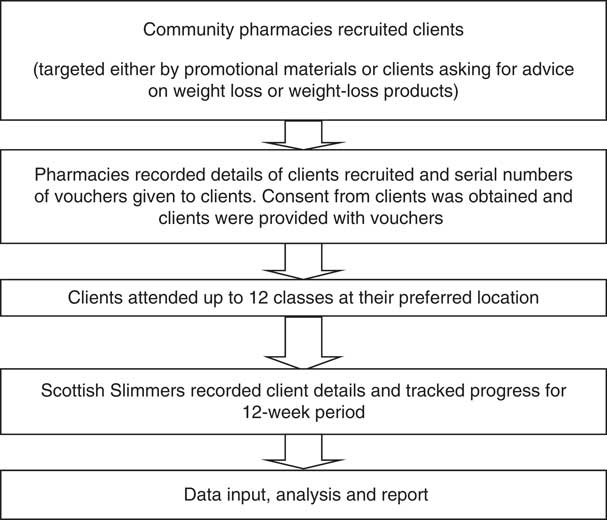
Fig 1 Client recruitment process for the present study evaluating a community pharmacy signposting service to a commercial weight-loss provider
Quantitative data sources
Client characteristics
Pharmacy staff recorded clients’ names, addresses, telephone contact details, weight, height, voucher serial numbers, date of collection of vouchers and obtained client consent. These details were recorded in the client pharmacy log, which was stored securely. A record was also kept of the number of clients who declined participation and, if known, the reason for refusal. Clients who wished to think about participation were invited to return later. If they did not return within the duration of the study, they were categorized as a ‘refusal’.
Weight measurement and attendance at Scottish Slimmers’ classes
SS also recorded client contact details, calculated BMI, logged dates attended, client weight and voucher serial numbers. These details were stored securely by the SS coordinator. NHS Grampian personnel liaised with SS and the research team to facilitate data collection and provision. The Scottish Index of Multiple Deprivation (SIMD; http://www.gov.scot/Topics/Statistics/SIMD, Scottish Datazone version) was calculated using each client’s postcode.
Quantitative outcome measures
Quantitative outcome measures were the following:
1. the number of clients who were offered/requested the service;
2. the number of clients who consented to use the service;
3. persistence of client attendance at SS classes; and
4. weight changes of clients referred from the community pharmacy-based service.
Analysis
The quantitative data derived from clients and pharmacies were entered into a database in the statistical software package IBM SPSS Statistics version 22, with a 10 % accuracy check being performed by a member of the department administrative staff (H.R.). The data were analysed using descriptive statistics. We analysed weight change data with the last observation carried forward( Reference Steiner 10 ) and the baseline observation carried forward( Reference Cresswell and Mander 11 ) to take account of missing data.
Qualitative data sources
Client experience of the referral service
Telephone interviews were conducted with clients, based on voucher allocation. A random sample of clients was selected( Reference Pittendreigh 12 ) from each of the three voucher allocation methods and those contactable by telephone were interviewed to explore their attitudes and opinions about the future delivery of the service.
Written consent to participate in an interview was obtained at the point of recruitment. Verbal consent was sought prior to starting the interview, which was recorded with each client’s consent.
Pharmacy staff members’ experience of the referral service
Pharmacy personnel were given the option of either attending a focus group or participating in a telephone interview to explore their experience of the service and to obtain suggestions for future service delivery. The intention was to derive evidence from each of the participating pharmacies.
Qualitative outcome measures
Qualitative outcome measures were the following:
1. client experience of, and satisfaction with, the referral service; and
2. pharmacist and pharmacy support staff experience of, and satisfaction with, the provision of the service.
Analysis
The qualitative data were digitally recorded, transcribed verbatim by a research secretary and checked for accuracy by the researcher (J.I.). Thematic analysis of the transcripts was performed using the themes included in the topic guide, as well as newly emergent themes (by J.I.).
Results
Of the twenty-three community pharmacies invited, ten consented to participate, five of which were situated in deprived areas (SIMD score=1–2; Table 1). Of the 145 clients enquiring about the service, sixteen were excluded due to age, BMI or health reasons (Fig. 2). Of the 129 clients recruited, ninety-seven attended at least one SS class.
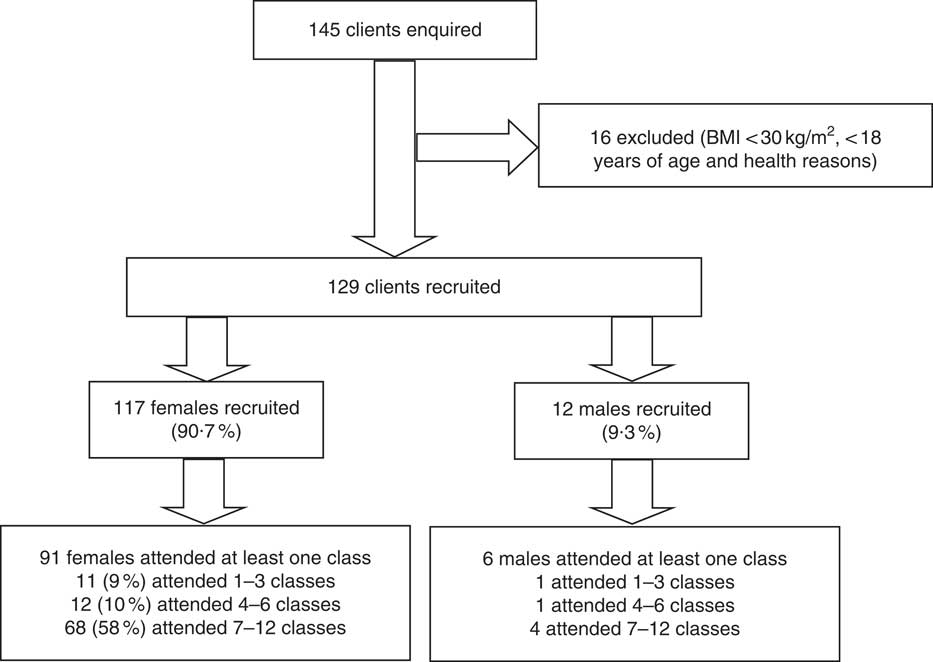
Fig. 2 Flowchart detailing client retention for the present study evaluating a community pharmacy signposting service to a commercial weight-loss provider
Table 1 Characteristics of the pharmacies participating in the community pharmacy signposting service to a commercial weight-loss provider, Aberdeen City, Scotland, November 2013–August 2014
SIMD, Scottish Index of Multiple Deprivation (SIMD score=1, most deprived; SIMD score=5, most affluent); SS, Scottish Slimmers; small chain, >10 pharmacies; large multiple, >30 pharmacies.
Eight of the ten pharmacies recruited clients to the service. Of these eight pharmacies, three recruited fewer than ten clients while the remainder either met or exceeded the original recruitment target (n 20). In all but one pharmacy, the weight management service was delivered by either the pharmacist or other pharmacy staff (i.e. dispensing technician, pre-registration student or a pharmacy manager). In the remaining pharmacy, the service was delivered solely by non-pharmacist personnel (i.e. pharmacy counter staff). Client demographics are presented in Table 2. Most participants were female; 6 % (n 6) were male. Most clients who attended the SS classes were between 40 and 70 years of age and over half of attendees (53 %, n 51) lived in more deprived areas of Aberdeen. The majority of clients (63 %, n 61) attended a class within 7 d of recruitment. Most clients had visited the pharmacy before; but for six clients recruitment occurred on their first visit to the community pharmacy. Nearly 40 % (n 38) of clients who attended classes had visited the pharmacy to ask for advice regarding weight loss or to sign up for the service. Most clients (63 %, n 58) opted to receive all twelve vouchers at one time, with 28 % (n 26) and 9 % (n 8) opting for monthly and weekly supply, respectively.
Table 2 Characteristics of clients at each community pharmacy participating in the community pharmacy signposting service to a commercial weight-loss provider, Aberdeen City, Scotland, November 2013–August 2014
M, male; F, female; SIMD, Scottish Index of Multiple Deprivation (SIMD score=1, most deprived; SIMD score=5, most affluent); SS, Scottish Slimmers.
Small chain pharmacies (pharmacies with fewer than ten stores) recruited the most clients (n 39) from deprived areas. Independent single-outlet pharmacies recruited most clients living in more affluent areas (n 20). Over 50 % (n 51) of clients who participated lived in areas with SIMD score of 1 or 2 (i.e. most deprived areas).
The median number of classes attended was 12 (interquartile range=6·5–12). Fifty-one clients (53 %) attended all twelve classes. Women were more likely to attend seven to twelve classes compared with men: sixty-eight women (58·1 % of those recruited) v. four men (33·3 % of those recruited).
At baseline, the mean weight of clients was 99·4 (sd 17·5) kg and their mean BMI was 37·8 (sd 6·0) kg/m2. All clients had a BMI calculated at their community pharmacy of ≥30 kg/m2; however, four had a BMI<30 kg/m2 based on their measurements taken at an SS class. For the ninety-seven clients who attended at least one class, mean weight change calculated using the last observation carried forward was −3·70 (sd 8·43) kg over the 12-week period, representing a mean weight loss of −3·7 % of initial weight (Table 3). The mean weight change using the baseline observation carried forward was −2·86 (sd 8·43) kg and this represented −2·8 % of initial weight. Additionally, 34 % (n 35) of clients lost 5 % of their body weight and four lost 10 % over 12 weeks.
Table 3 Weight change characteristics over a 12-week period of clients (n 97Footnote *) participating in the community pharmacy signposting service to a commercial weight-loss provider, Aberdeen City, Scotland, November 2013–August 2014
LOCF, last observation carried forward; BOCF, baseline observation carried forward.
* One hundred and twenty-nine clients were recruited, but ninety-seven attended classes.
Client interviews
Twenty clients were randomly selected for a telephone interview, of whom thirteen were interviewed. Eight interviewees received all their vouchers at the start, four received monthly vouchers and one client obtained vouchers on a weekly basis. Three of the clients interviewed had never attended classes. The ten remaining clients had varying attendance. Six clients attended twelve classes and continued to attend classes (self-payment). One client mentioned that she had completed the twelve free classes but could not afford to attend further classes. Three clients were still attending classes and indicated that they intended to complete all twelve classes. Illustrative quotes are presented for clients’ attitudes and opinions of the service in Table 4. Quotes include a code that incorporates each client’s identification number, voucher allocation method, weight change and interview quote line number.
Table 4 Clients’ and pharmacists’ attitudes and opinions of the community pharmacy signposting service to a commercial weight-loss provider
GP, general practitioner.
Awareness of the scheme was mostly derived through promotional materials displayed in the pharmacies. Three clients indicated they had become aware of the study through word of mouth from family or friends. Most clients stated that they signed up for the study immediately. One male client stated he needed some time to think about it before he signed up.
Reasons for deciding to take part in the scheme were influenced by other health problems. Specific health issues included leg ulcers, diabetes, raised blood sugar levels, increased blood pressure, heart problems and arthritis.
The free availability of the classes appeared to be an incentive to enrol in the study. For some clients, their decision to participate was a spur-of-the-moment decision and others spoke about peers (family members, friends) attending SS classes and this was an incentive to participate.
At the time of interview, three clients had not attended a class. The reasons for non-attendance ranged from changes to personal circumstances, illness or holiday, to the friends they had signed up with not attending the classes.
Some clients were unsure of who they had initially spoken to regarding the study. The majority thought they had initially spoken to pharmacy counter staff. Two clients had been given appointments to return to discuss with the pharmacist and enrol in the study. Privacy was mentioned by two clients within the context of their experience of the service. One client stated that she would not have liked to ask or discuss the study if there had been other people waiting in the pharmacy. Most clients reported that they had been taken into a consultation room to discuss the study and to be weighed to assess their eligibility for the study. These clients indicated that this was a satisfactory arrangement. One client stated that if there had not been a private area she would not have taken part in study. Clients commented that pharmacy staff were supportive of their weight management attempts.
All the clients interviewed who had attended classes had lost weight, were complementary about the classes and appeared satisfied with their weight loss. There were comments on how encouraging and good the leaders were, as well as on the useful information they received. The majority of clients interviewed were happy to discuss their weight with pharmacy staff, primarily because they had been taken into the pharmacy consultation room. Another client indicated that she was initially embarrassed discussing her weight and there were other comments of ‘nobody being comfortable’ discussing their weight. All clients interviewed considered the pharmacy staff to be either very good or excellent in terms of professionalism.
Voucher allocation varied across the clients interviewed. There appeared to be a preference for vouchers to be allocated less frequently than weekly (i.e. monthly or all at once). When clients were asked if they intended to carry on with the classes, most of them stated that they would.
All interviewed clients considered had positive attitudes towards the signposting service. There were comments about clients being happy to approach pharmacy staff and it being a convenient service. A large number of the clients interviewed commented on the fact it was a free service. Two clients had negative comments regarding the service and this was about having to pay for classes after the initial 12-week service, even if they did not attend.
There were suggestions about how the service could be improved. One client suggested that more members of staff could have received training and several clients commented on how busy the pharmacy was and the need for more staff. Two clients thought that there could have been more leaflets available to take away and read. Several clients thought that more vouchers could be allocated if their BMI was rated as obese.
One client mentioned that she had not considered going to her general practitioner about her weight. The majority of clients stated that they probably would not have done anything about their weight and just carried on with their current eating habits, if this service had not been available.
Pharmacy personnel interviews
Five pharmacists and two dispensing technicians (from seven pharmacies) participated in a telephone interview. Table 4 presents pharmacists’ attitudes and opinions of the service; the quotes include a code that incorporates each pharmacist’s identification number and interview quote line number.
Reasons for participating included the importance of supporting research alongside the fact that obesity is a major health issue. One pharmacist commented on the ‘local’ issue of service provision and the idea of being able to help people with their weight management.
Pharmacies used different methods to deliver the service and some operated an appointment system. Some pharmacies considered appointment systems to be difficult due to unpredicted increases in workload.
In most instances, clients approached the pharmacy staff; however, one member of pharmacy staff mentioned having a discussion with a client about weight-loss medication and informing them about the service. In some pharmacies, the counter staff completed the entire consultation and they were confident to do this. Two pharmacists spoke of training all the pharmacy staff regarding the study.
Interviewees did not hold strong views regarding the different methods of voucher allocation. There were positive comments regarding the promotional material.
Most pharmacy staff reported that the referral service was not time-consuming, with most estimating around 10 min for the initial consultation. The administrative packs for clients also helped reduce workload. One pharmacist mentioned that twenty clients was a manageable number, but if it were to be expanded to more people there would need to be an appointment system.
All the pharmacists and pharmacy staff thought the training in groups was sufficient. When asked if individual staff training would have been a better option, comments were varied; some interviewees thought it would have been a good idea, but others did not consider it necessary. One pharmacist commented that if it was to be rolled out as an NHS service, it would be better to have a training evening.
Most pharmacists considered that the payment offered was adequate while one commented that it did not compare favourably with another service that they provided.
One pharmacist thought it would be good to inform the client’s general practitioner of their participation in the service. There were two additional comments from pharmacists that the BMI chart utilized in the study was too low; that is, it did not provide higher BMI (e.g. >40 kg/m2) as a lot of clients had a BMI above this value.
Five out of seven of the pharmacy staff interviewed considered that the study had been a success because they had signed up several clients. Interviewees also spoke of clients coming back to the pharmacies to tell them how they were getting on. One staff member mentioned that clients seemed to like the idea that they were not limited to attending one class in a set location, they could choose to attend classes in other parts of the city.
Of the two pharmacies where no clients were recruited, one pharmacist thought it was because they could not promote the service enough; that is, it was company policy to display certain promotional material in prominent places only, such as window displays. The other pharmacist thought they were unsuccessful because they were unable to approach clients and none of their customers appeared interested.
Pharmacy staff appeared positive and willing to provide the service in the future. The interviewees from two pharmacies that recruited no clients stated they would be happy to provide the service in the future, although they would have to consider alternative promotional strategies.
Discussion
The present paper is the first published evaluation of a community pharmacy-based signposting service to a commercial weight management organization. This feasibility study is novel in that it assesses community pharmacies as a source of referring people who are obese to a weight management service. The service is also free of charge, which allows inclusion of all customers. The prospective, mixed-methods approach provided a holistic evaluation of this service. It was found that community pharmacy customers found this method of being referred to a commercial slimming organization acceptable and it is therefore a feasible option for health-care governing bodies to consider.
The main study limitations stem from the fact that it was a small-scale study run over a period of 12 weeks; therefore, the results may lack generalizability in terms of service providers and users. Community pharmacies were recruited from within Aberdeen City and therefore results may not be representative of the whole Scottish population, as more rural communities have not been included. Pharmacy personnel were unable to proactively recruit clients (due to constraints placed by the College Ethics Review Board) except in limited circumstances whereby customers enquired about weight-loss advice or products, and, as such, service uptake was mostly dependent upon customers approaching pharmacy staff. Due to time constraints, interviews were not completed with clients who attended only a few SS meetings.
Variation in client recruitment across pharmacies could be partially attributed to variable footfall. In addition, the non-recruiting pharmacies were situated in a city centre where customers might be more transient and possibly have less of a relationship with pharmacy staff. Two-thirds of participating clients visited their community pharmacy at least once per month; this may indicate that an existing relationship with a pharmacy may be beneficial in achieving service uptake( Reference Brown, Todd and O’Malley 13 ). The intention of the study was to focus on pharmacies in deprived areas in an attempt to reach clients. The SIMD value for a pharmacy will not necessarily reflect client SIMD and this is particularly true for city-centre pharmacies with high customer footfall. Despite these limitations, over half the clients who participated were from more deprived areas in Aberdeen City. Additionally, it is likely that uptake of the service will have been amplified due to the vouchers being free of charge. Men use pharmacies much less frequently than women( Reference Boardman and Avery 14 ) and only six male clients were recruited to the study.
Eligible clients were required to have BMI≥30 kg/m2. Discrepant BMI values occurred with four clients between pharmacy and SS personnel, with the latter estimating BMI values of <30 kg/m2. This could be due to measurement error and/or it might be explained by the lag time between clients being recruited at pharmacies and the actual date they went to their first SS class; clients might have initiated weight loss prior to attending their first SS class.
The majority (63 %) of clients were given all twelve vouchers at baseline. Clients who were interviewed were not enthusiastic about collecting vouchers weekly but were more supportive of monthly collection.
Retention at SS classes was good, with fifty-one (53 %) clients. This rate compares favourably with previous studies, including studies of referring from primary care organizations( Reference Jolly, Lewis and Beach 15 , Reference Ahern, Olson and Aston 16 ), and is considerably higher than community pharmacy studies evaluating standalone weight management services( Reference Boardman and Avery 14 , Reference Stubbs, Pallister and Whybrow 17 ).
The mean weight change achieved by clients across their twelve SS classes was −2·86 kg using the baseline observation carried forward method. This equates to a loss of 2·8 % of initial weight. These results are comparable with similar evaluations, namely signposting from a primary care organization to a commercial weight management organization( Reference Jolly, Lewis and Beach 15 , Reference Ahern, Olson and Aston 16 ), and are better than standalone weight management methods( Reference Boardman and Avery 14 ). Peer support has been shown to facilitate adherence to healthy eating plans( Reference Robertson, Archibald and Avenell 18 ) and clients in the present study mentioned support from pharmacy staff as helping with their weight management. The additional support that pharmacy staff provided, whether formal or informal, was highlighted by clients during interviews and may be an advantage of community pharmacies compared with other primary health-care providers whose interaction might be more time-restricted.
All clients interviewed had positive attitudes towards the signposting service and the SS classes (although three had not attended a class at the time of their interview). Interviewees indicated that they were aware they were overweight and some perceived that this was having a negative impact on their health. Despite this, the majority of interviewees stated they would not have taken action about their weight if they had not participated in the study. Two interviewees who had not attended a class had heard of the signposting service from a friend or family member, who had suggested they participate. The lack of engagement with the service by these clients may have been due to a lack of readiness to address their weight( Reference Michie and Johnston 19 ).
Privacy was important to all interviewees and all were satisfied with their consultations taking place in a pharmacy consultation room. A number of clients interviewed indicated that further free provision of SS vouchers would be a good idea for those who had not reached their target weight or healthy BMI.
The community pharmacy staff interviewed were very positive about the study and indicated they would be happy to provide this type of service in the future. The signposting service was not perceived to have a substantial impact on workload.
Conclusion
In conclusion, the present study demonstrated the feasibility of providing a community pharmacy-based signposting service to a commercial weight management service. The signposting service was acceptable to both service users and providers. The effectiveness and cost-effectiveness of this service need to be evaluated to explore whether it is viable adjunct to existing weight management services for obese patients.
Acknowledgements
Acknowledgements: The research team would like to thank all community pharmacies that participated, and all staff and participants involved with the study; Mrs Hazel Riley for transcribing the interviews; and David Ritchie from Research & Data Management, University of Aberdeen. Financial support: The study was funded by NHS Grampian. NHS Grampian had no role in the design, analysis or writing of this article. The Health Services Research Unit is funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates. Scottish Slimmers had no involvement in the design, analysis and reporting of this study. Conflict of interest: None. Authorship: M.C.W. was the principal investigator and contributed to the design, delivery and evaluation of the study as well as the preparation and critical review of this manuscript. J.I. was the research assistant working on the project and was responsible for the delivery of the study and the preparation of this manuscript. L.A. advised on study design, supervised the analysis, and contributed to the preparation and revision of this manuscript. A.A. advised on study analysis and revised drafts of this manuscript. Ethics of human subject participation: The College of Life Sciences and Medicine Ethics Review Board, University of Aberdeen, gave ethical approval of the study. All clients gave their consent to participate.








