Introduction
Awareness and knowledge of concussion and post-concussion symptoms have grown significantly in the last two decades, contributing to recognition that it is a significant public health issue for Australia and globally (Bazarian, Reference Bazarian2019; Evans, Reference Evans2021). The term concussion is frequently used interchangeably with mild traumatic brain injury (mTBI); however, it is generally considered the beginning of the mTBI spectrum (Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021). Traumatic brain injury (TBI) is an injury to the brain caused by external force or trauma to the head with significant variation in causes, severity of injury and outcomes (O’Reilly et al., Reference O’Reilly, Wilson and Peters2018). Severity classifications include mild, moderate and severe. The lack of universal definition for mTBI and concussion is problematic with respect to both research and clinical practice. An expert panel, led by Silverberg and Iverson, is currently undertaking a review to update the definition of mTBI to address this issue (Silverberg et al., Reference Silverberg, Iverson, Arciniegas, Bayley, Bazarian, Bell and Whitehair2021). The most widely used definition is by the American Congress of Rehabilitation Medicine (ACRM) from 1993, ‘a traumatically induced physiological disruption of brain function’ as a result of headstrike or ‘the brain undergoing an acceleration/deceleration movement’ in conjunction with any of the following: a brief loss of consciousness (less than 30 min), post-traumatic amnesia of less than 24 h, a period of confusion and a Glasgow Coma Scale score of 13–15 (ACRM, 1993, p. 86; Quinn et al., Reference Quinn, Mayer, Master and Fann2018). Concussion may occur in the absence of loss of consciousness or results on imaging (Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021; Silverberg et al., Reference Silverberg, Iverson, Arciniegas, Bayley, Bazarian, Bell and Whitehair2021).
Of all TBI cases, mTBI is estimated to represent 80–90% and equate to approximately 42 million cases worldwide each year (Chen et al., Reference Chen, Lin, Huda and Tsai2020; Quinn et al., Reference Quinn, Mayer, Master and Fann2018). Despite typically requiring less health and disability resources than more severe injuries, due to their volume, mTBI accounts for majority of the economic burden (Nguyen et al., Reference Nguyen, Fiest, McChesney, Kwon, Jette, Frolkis and Gallagher2016; Theadom et al., Reference Theadom, Starkey, Barker-Collo, Jones, Ameratunga and Feigin2018). Typical causes include sports-related injuries, falls, road trauma, assaults and combat injuries. Awareness of concussion has increased, influenced significantly by high profile cases from sport, public health campaigns and acknowledgement of combat-related TBI (Evans, Reference Evans2021; Simpson-Jones & Hunt, Reference Simpson-Jones and Hunt2019). It is thought the rising incidence is partly due to more people seeking medical attention and increased confidence of those diagnosing (Langer et al., Reference Langer, Levy and Bayley2019). Incidence estimates are likely underestimated as they are typically calculated from hospital admissions and many people who sustain a concussion do not present to hospital. They may see a General Practitioner (GP) or not seek medical input at all (Lee et al., Reference Lee, Amatya, Judson, Truesdale, Reinhardt, Uddin and Khan2019; Prince & Bruhns, Reference Prince and Bruhns2017). The traditional opinion that people sustaining concussion do not require intervention as the majority recover has been challenged. It is now understood that 15–30% of people who sustain a concussion go on to suffer persistent post-concussion symptoms (PPCS) for months or even years. Whilst this may be considered a minority of cases, the impact of persistent symptoms on function and quality of life are significant (Möller et al., Reference Möller, Lexell and Wilbe Ramsay2021; Popov et al., Reference Popov, Mercier, King, Fung and Debert2021). Larson-Dupuis & De Beaumont (Reference Larson-Dupuis and De Beaumont2016, p. 1237) stated simply and accurately, ‘mild injury severity…does not mean mild consequences’.
In addition to the confusion surrounding mTBI definitions, PPCS remains a controversial topic with ongoing debate. Varying terms are used including prolonged post-concussion (or post-concussive) symptoms, difficult concussion, post-concussion syndrome (PCS) and more recently PPCS (Makdissi et al., Reference Makdissi, Cantu, Johnston, McCrory and Meeuwisse2013; Zasler et al., Reference Zasler, Haider, Grziboweki and Leddy2019). PCS has been defined by criteria from either the DSM-IV or ICD-10, with these two diagnostic tools containing important differences such as the DSM-IV requiring immediate onset of symptoms when the ICD-10 does not. Of note, the DSM-V does not include PCS and directs those diagnosing to either mild or major neurocognitive disorder due to TBI (Polinder et al., Reference Polinder, Cnossen, Real, Covic, Gorbunova, Voormolen and von Steinbuechel, N2018; Quinn et al., Reference Quinn, Mayer, Master and Fann2018). Recently, several authors have argued that the term ‘syndrome’ should not be used as this suggests a consistency which does not exist for concussion given the heterogeneity of symptoms and presentations. Their preferred term is PPCS (Popov et al., Reference Popov, Mercier, King, Fung and Debert2021; Rickards et al., Reference Rickards, Cranston and McWhorter2020; Zasler et al., Reference Zasler, Haider, Grziboweki and Leddy2019). For the purposes of this study, the term PPCS will be used. There is also debate regarding the timeframe for classification of ‘persistent’ symptoms beyond expected recovery time, typically either over 14 days or 3 months (Polinder et al., Reference Polinder, Cnossen, Real, Covic, Gorbunova, Voormolen and von Steinbuechel, N2018; Zasler et al., Reference Zasler, Haider, Grziboweki and Leddy2019). Further complexity is added to the discussion due to 1. symptoms not being specific to TBI, 2. commonly occurring symptoms may be misattributed to concussion and 3. debate regarding aetiology being neurogenic (biological/ from primary injury) or psychogenic (pre-morbid psychopathology or personality characteristics) or both (Broshek et al., Reference Broshek, De Marco and Freeman2015; Prince & Bruhns, Reference Prince and Bruhns2017).
TBI’s heterogeneous nature is a distinguishing feature of the condition, and this remains true when discussing prolonged concussion. The range of and often interrelated symptomatology adds to the complexity. Recent work has distinguished five subtypes of concussion symptoms: cognitive, headache/migraine, vestibular, ocular motor and anxiety/mood, as well as an associated condition of sleep disturbance. Of note, study results differed between adult and paediatric patients with prevalence ratios in concussion patients verses control groups for all five subtypes available for adults only (Lumba-Brown et al., Reference Lumba-Brown, Teramoto, Bloom, Brody, Chesnutt, Clugston and Ghajar2020). A range of skills and expertise are required to address all the potential issues. It is on this basis alone that many authors argue an interdisciplinary approach is required in management and treatment (Bazarian, Reference Bazarian2019; Schneider, Reference Schneider2019).
There is a wide variability in terms used when discussing the bringing together of various clinical disciplines: interdisciplinary, multidisciplinary, interprofessional, multiprofessional or multimodal (Bazarian, Reference Bazarian2019; Chamberlain-Salaun et al., Reference Chamberlain-Salaun, Mills and Usher2013). This further inconsistency adds to the confusion and difficulty for research and clinical practice. These terms are frequently used interchangeably or left undefined in the literature. In contrast they may be used to distinguish different approaches. Multidisciplinary refers to two or more disciplines who typically work in silos and have their own goals with the patient, whereas interdisciplinary or interprofessional work is collaborative to achieve outcomes more than would otherwise be achieved (Chamberlain-Salaun et al., Reference Chamberlain-Salaun, Mills and Usher2013; Morley & Cashell, Reference Morley and Cashell2017). In interdisciplinary work, there is understanding of each other’s roles and overlap between roles is recognised. A range of disciplines may be included within an interdisciplinary approach for concussion depending on individual need: Rehabilitation Physician, Physiotherapy, Exercise Physiology, Neuropsychology, Clinical Psychology, Speech Pathology, Occupational Therapy, Social Work, Ophthalmology, Rehabilitation Nursing and/or Dietician (Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021; Neumann et al., Reference Neumann, Gutenbrunner, Fialka-Moser, Christodoulou, Varela, Giustini and Delarque2009). Interdisciplinary and collaborative practice in healthcare have been established as best practice, demonstrating a variety of benefits including, but not limited to, quality and safety, patient outcomes, patient engagement and staff satisfaction (Clarke & Forster, Reference Clarke and Forster2015; Morley & Cashell, Reference Morley and Cashell2017; Pabian et al., Reference Pabian, Oliveira, Tucker, Beato and Gual2017). An interdisciplinary approach is recommended for concussion management by the Ontario Neurotrauma Foundation, a world- renowned organisation whose Clinical Practice Guidelines are referenced by experts in the field (Ontario Neurotrauma Foundation, 2018). Despite this, and the important distinction between terms, multidisciplinary is most used in literature (Chamberlain-Salaun et al., Reference Chamberlain-Salaun, Mills and Usher2013). In acknowledgement of the distinct meaning and recommendations for interdisciplinary practice, the term interdisciplinary was chosen for this research question and will be used throughout the paper.
In the past decade, large volumes of research have been completed into mTBI and concussion, particularly with respect to sports-related concussion and combat-related injuries (Armistead-Jehle et al., Reference Armistead-Jehle, Soble, Cooper and Belanger2017; Brush et al., Reference Brush, Ehmann, Olson, Bixby and Alderman2018). Considerable research specific to children and adolescents has been completed. As it is established that concussion treatment for this population is distinct from that of adults, this research will focus only on adults (Makdissi et al., Reference Makdissi, Davis and McCrory2014; Purcell et al., Reference Purcell, Davis and Gioia2019). Recognition of concussion as a heterogeneous and complex condition is not new. Iverson, Zasler and Lange, in 2007, discussed the need for a biopsychosocial model of care and McCrea and Powell, in Reference McCrea and Powell2012, outlined their clinic’s interdisciplinary approach to evaluation and treatment (McCrea & Powell, Reference McCrea and Powell2012). Despite the large volumes of research there remains a lack of clarity within definitions; for diagnosis and best practice for PPCS. In contrast, understanding concussion, the complexity and heterogeneity of the condition could provide the explanation as these very factors are what make research difficult (Arbabi et al., Reference Arbabi, Sheldon, Bahadoran, Smith, Poole and Agrawal2020; Kenzie et al., Reference Kenzie, Parks, Bigler, Lim, Chesnutt and Wakeland2017).
There are systematic literature reviews on various assessments or treatments for mTBI, concussion and PPCS and some of these include discussion of interdisciplinary practice (Harris et al., Reference Harris, Rafeedie, McArthur, Babikian, Snyder, Polster and Giza2019; Makdissi et al., Reference Makdissi, Schneider, Feddermann-Demont, Guskiewicz, Hinds, Leddy and Johnston2017). Systematic reviews also exist on the management and treatment for TBI more broadly which may include reference to interdisciplinary practice (Arbabi et al., Reference Arbabi, Sheldon, Bahadoran, Smith, Poole and Agrawal2020; Möller et al., Reference Möller, Lexell and Wilbe Ramsay2021). There has not been a systematic review specifically focused on the effectiveness of an interdisciplinary approach for the treatment of PPCS, to the authors’ knowledge. Therefore, the objective of this review is to examine the evidence for the interdisciplinary approach in treatment of persistent post-concussion symptoms in adults. This evidence will inform health services, clinicians, sports administrators and researchers with regard to concussion clinic and rehabilitation team design and service delivery.
Methods
In accordance with the Preferred Reporting Items for Systematic and Meta-Analysis (PRISMA) guidelines, a systematic literature search was undertaken (Page et al., Reference Page, Moher, Bossuyt, Boutron, Hoffmann, Mulrow and McKenzie2021a). It was not preregistered with PROSPERO. Between 11 and 14 August 2021, five electronic databases were searched: CINAHL (EBSCOhost), Informit, ProQuest (Health & Medicine), PubMed and Scopus. A further search of Google Scholar and references of identified articles was completed to ensure all possible relevant evidence was included.
The search strategy included key terms for concussion, utilising the Boolean operator ‘OR’: concussion, ‘post-concussion’, ‘post concussion’, postconcussion, ‘post-concussive’, ‘post concussive’ or postconcussive. The Boolean operator ‘AND’ was then utilised to combine the concussion terms with key terms for interdisciplinary, again utilising ‘OR’: interdisciplinary, ‘inter-disciplinary’, multidisciplinary, ‘multi-disciplinary’, or interprofessional. Relevant MeSH Terms (brain concussion, post concussion syndrome, post concussion symptoms) were included where appropriate. Consultation with a librarian from the University of New England (UNE) and Barwon Health was completed to finalise the search strategy. The search was limited to literature published between 2011 and 2021 to return contemporary evidence.
Inclusion and exclusion criteria
Firstly, the records were manually screened from titles and abstracts for relevance to the literature review by both authors. Studies were included if they were published in peer-reviewed journals, in English, human studies, included adults (over 16 years) who had sustained a concussion, and included a focus on an interdisciplinary approach. Studies were excluded if they were commentaries only, review articles, included paediatric and/or adolescent (0–18 years) participants only, and if focused on evidence for a single discipline only. The full text of potential studies was then reviewed manually and included if available in full text, original research (randomised controlled trials (RCTs), quasi-experimental designs or cohort studies), and addressed the utilisation of an interdisciplinary approach for the treatment of persistent concussion symptoms or post-concussion syndrome. Articles were excluded if they were not available in full text, not freely available through either UNE or Barwon Health libraries, focused on the acute period of concussion (within the first 2 weeks), case study only, description only of an intervention, or focused on single discipline intervention; even if within an interdisciplinary approach.
Data extraction
The first author extracted data using a standardised data extraction form and the second author confirmed the extracted information. The data extraction form was grouped into two sections. The first section was related to the characteristics of included studies such as authors, year of publication, study design and setting, intervention, and demographics of the study participants. The second section documented information on the measures, assessments and outcomes of the included studies.
Quality appraisal
Quality appraisal was undertaken to determine the methodological quality and risk of bias of the included studies. The ‘Critical Appraisal Skills Program (CASP) RCT Checklist’ was utilised for the RCTs and the ‘Appraisal Tool for Cross-Sectional Studies’ (AXIS) was used for the non-randomised quantitative and cross-sectional studies. The CASP RCT Checklist is a commonly used appraisal tool, considered user-friendly and contains eleven questions about internal and external validity (Long et al., Reference Long, French and Brooks2020). The first three questions are screening questions, followed by eight further questions focusing on specific criteria. Each question can be answered ‘Yes,’ ‘No’ or ‘Can’t tell.’ The AXIS tool is newer and was developed to address the gap at the time for critical appraisal of non RCT studies, which were being acknowledged as important in evidence-based practice (Downes et al., Reference Downes, Brennan, Williams and Dean2016; Ma et al., Reference Ma, Wang, Yang, Huang, Weng and Zeng2020). It contains twenty questions and, similar to the CASP checklist, each question is answered ‘Yes,’ ‘No’ or ‘Don’t know.’ Quality appraisal was completed independently by two reviewers for each included article with variance discussed and resolved.
Results
Search results
The electronic database search identified 815 records. Further searching of references lists and Google Scholar did not identify any additional records. Duplicates were removed, leaving 336 records for which the title and abstracts were screened according to the inclusion criteria and a further 293 were removed. A total of 43 articles were sought, with four either being unavailable in full text or not freely available. The 39 obtained were reviewed with inclusion and exclusion criteria applied and six were deemed to meet criteria for this review. Several articles provided a comprehensive account of an interdisciplinary treatment approach for concussion and included reference to relevant evidence, however, were excluded as descriptions of current programmes only, not comparative studies (Chen et al., Reference Chen, Kouts, Rippee, Lauer, Smith, McDonald and Filardi2020; Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021; McCrea & Powell, Reference McCrea and Powell2012). Bauman et al. (Reference Bauman, MacDonald, Glatt, Doktor-Inglis and McLean2019) reported on a study conducted within an interdisciplinary care programme, however, as the purpose was to determine the value of a ‘treatment passport’ within this context, it was excluded. The UNE subject mentor provided guidance and opinion regarding the inclusion and exclusion of articles and thus a consensus was obtained. See Fig. 1 for the PRISMA flow diagram of included studies.

Figure 1. PRISMA flow diagram of included studies (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow and Moher2021b).
A summary of the characteristics of included studies for this review is provided in Tables 1 and 2. The six included studies shared a focus on determining if an interdisciplinary treatment approach was beneficial, however, they were heterogenous in purpose, study design, setting, population, terms used, interdisciplinary approach, treatment provided, follow-up and measures used. Three RCTs and three studies of interdisciplinary programmes with no control group (two of which were retrospective) were included. All studies included a goal of reducing symptoms, but varied in their purpose from evaluating neurocognitive function, to return to play (RTP) and return to work (RTW). The studies included 685 participants with persistent concussion symptoms, 407 (59.5%) male and 278 (40.5%) female. Three studies had majority of female participants (all over 64%) and three of male (56.7–89.1%). See Table 1 for a list of characteristics for the included studies.
Table 1. Characteristics of included studies
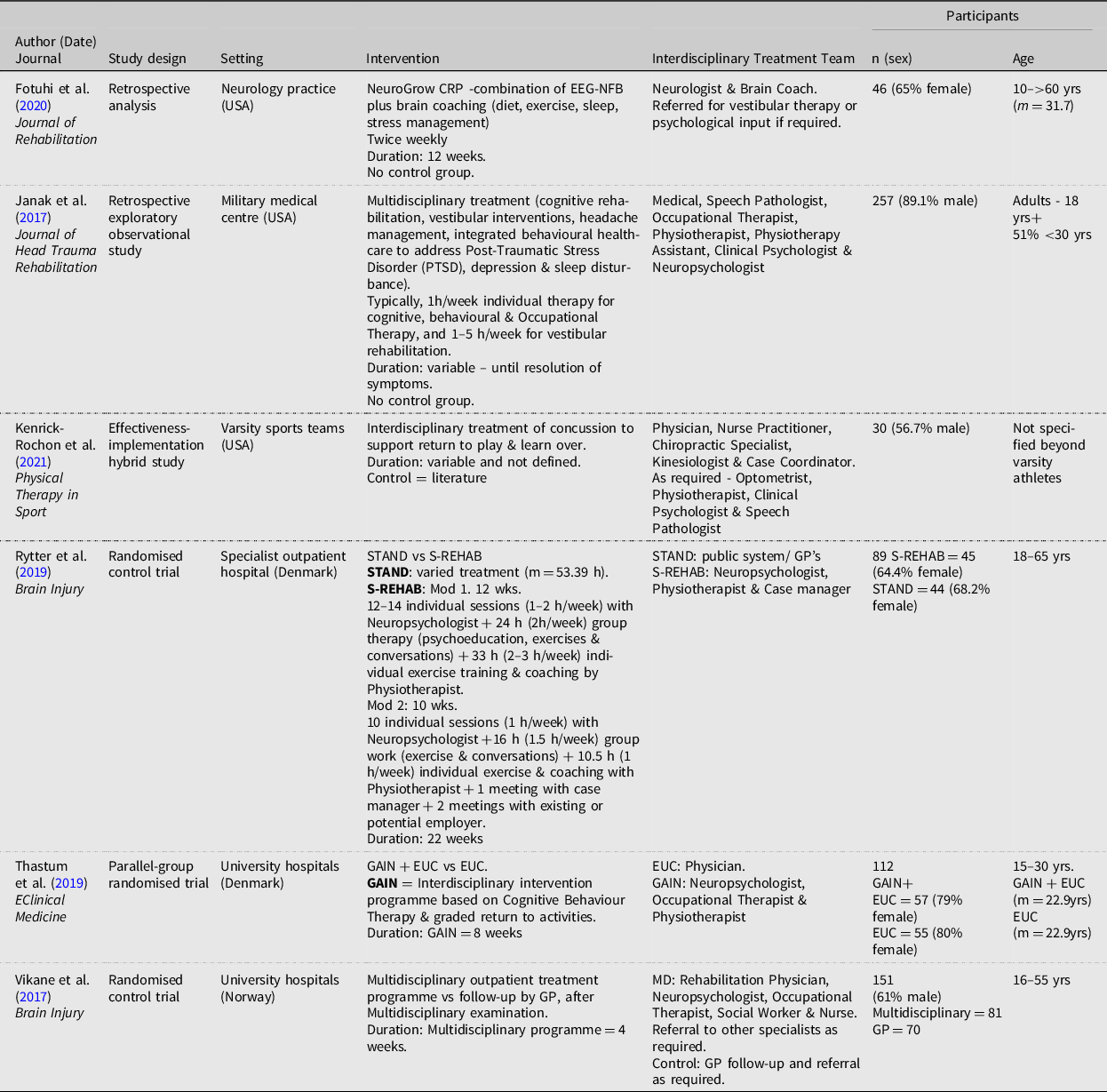
Abbreviations: EEG-NFB = electroencephalogram-based neuro-feedback, EUC = Enhanced Usual Care, GAIN = Get going After concussion, GP = General Practitioner, m = mean, NeuroGrow CRP = NeuroGrow Concussion Recovery programme, PTSD = Post-Traumatic Stress Disorder, S-REHAB = Specialised interdisciplinary rehabilitation programme, STAND = Standard Care, wk = week.
Table 2. Measures and outcomes of included studies

Abbreviations: EEG = electroencephalogram, EUC = Enhanced Usual Care, GAIN = Get going After concussIoN, PCS = Post-concussion Syndrome, PTSD = Post-traumatic Stress Disorder, S-REHAB = Specialised interdisciplinary rehabilitation programme, * = common measure used.
Setting and population
There was substantial variation between settings and population for the studies. The participants in Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) were recruited from their hospital admission, whilst participants in the remaining studies may or may not have been hospitalised following their injury. Fotuhi et al. (Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) and Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) required participants to have had persistent symptoms for more than 90 days and 6 months, respectively. The remaining studies included participants with varying times since injury and symptoms, therefore, were not exclusively addressing PPCS. One study was specific to a military population and thus included blast injury, which would not be the case for the general population (Janak et al., Reference Janak, Cooper, Bowles, Alamgir, Cooper, Gabriel and Orman2017). One study was specific to varsity athletes and sports-related concussion (Kenrick-Rochon et al., Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021). A further study included only young adults (15–30 years) (Thastum et al., Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019), whilst the remaining three studies included a broader age range and drew from the general population (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020; Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019; Vikane et al., Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017). Of note, Fotuhi et al. (Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) included a small number of adolescents. One study excluded participants with a history of or current psychiatric and/or chronic pain, whereas another only excluded those with severe psychiatric, neurological, or other medical disease. The remaining studies did not articulate such criteria.
Terms and definitions
Within the included studies, there was consistency in identifying concussion as a mTBI and qualifying that whilst most patients recover within weeks, some continue to experience symptoms for months or even years. As discussed previously, estimates regarding the incidence of prolonged symptoms vary and this was reflected across the studies: 10–15% (Thastum et al., Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019), 10–30% (Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019), up to 25% (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) and 5–20% (Vikane et al., Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017). Kenrick-Rochon et al. (Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021) and Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) noted the varied terminology used, PPCS or PCS, and lack of consensus for if these terms should be utilised at greater than 14 days or greater than 30 days. Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) noted that the diagnosis of PCS remains controversial and the shift from using the term PCS to PPCS. Two studies included only patients with PCS, applying the criteria of symptoms for over 90 days (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020; Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019), whilst the remaining studies included participants who had concussion and/or met criteria for PCS.
Interdisciplinary intervention undertaken – length and intensity
The interdisciplinary intervention applied in each study varied widely, as did the timeframe and intensity (see Table 1). Fotuhi et al. (Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) utilised only a Neurologist and Brain Coach for the intervention delivered, however, the Brain Coach provided a multidisciplinary intervention which included dietary, exercise, sleep and stress management education and advice. In addition, referrals were made as required for vestibular therapy and psychological input. Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) and Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) utilised three disciplines only (Neuropsychology, Physiotherapy and Case Manager, and Neuropsychology, Occupational Therapy & Physiotherapy respectively) for their intervention. Other studies utilised a wide range of disciplines, such as Janak et al. (Reference Janak, Cooper, Bowles, Alamgir, Cooper, Gabriel and Orman2017) who included seven disciplines (Medical, Speech Pathology, Occupational Therapy, Physiotherapy, Physiotherapy Assistant, Clinical Psychology & Neuropsychology).
The interventions undertaken ranged from three to four weeks (Kenrick-Rochon et al., Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021; Vikane et al., Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) to a 22-week programme (Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019). Intensity varied from 2 h per week (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) to approximately 6 h per week (Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019). Several studies did not specify a specific or regular intensity of intervention and for some studies intervention delivered was highly variable, dependent on individual need (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020; Kenrick-Rochon et al., Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021; Vikane et al., Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017).
Measures and assessment
There was also significant variation between measures used and the timing of the pre- and post-treatment assessment. See Table 2 for full details of the measures, testing and outcomes included in the studies. Majority of studies reported specifically the measures used, however, Kenrick-Rochon et al. (Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021) reported only that their testing was composed of neurocognitive, balance and reaction time testing, and a visual screening questionnaire, thus posing a barrier to duplicating the study. There was little similarity in measures used between studies. A total of 19 measures were specified across the studies, with the Rivermead Post-concussion Questionnaire (RPQ) being the only test common to more than one study. Two measures used by Fotuhi et al. (Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) were ‘in house’ tests and thus not validated. Additional to these measures, EEG brain mapping was utilised by Fotuhi et al. (Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020) and Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) referenced, without further explanation, a questionnaire regarding treatment received, and measured days to sustainable RTW. All studies completed pre- and post-treatment testing, however, varied regarding timing. Three studies nominated immediate assessment following treatment, with one also including a further 6 months follow-up (Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019). As their purpose was to clear players for return to sport as soon as possible, Kenrick-Rochon et al. (Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021) completed regular assessment until symptoms resolved and clearance to play was able to be given. Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) and Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) completed follow-up assessment (3 months follow-up, and 6 and 12 months, respectively). Thus, three studies provided evidence for the longer-term outcomes of the intervention (Rytter, et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019; Thastum et al., Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019; Vikane et al., Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017).
Outcomes
Benefits of an interdisciplinary approach were found in all included studies, however, varied in nature and significance. Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) and Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) found their interdisciplinary treatment provided meaningful benefits to the participants, including significant reductions in post-concussion symptoms. Additionally, reductions in depression, perpetuating illness perceptions and illness behaviours were reported by Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019). The improvements reported by Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) remained at 6 month follow-up, except for two factors, indicating sustained benefit. Reduction in both PPCS and Post Traumatic Stress Disorder (PTSD) symptoms were found by Janak et al. (Reference Janak, Cooper, Bowles, Alamgir, Cooper, Gabriel and Orman2017), however, as this was an exploratory observational study a causal relationship cannot be confirmed. Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) also found significantly reduced post-concussion symptoms in the intervention group as compared to control group. Whilst the authors acknowledged the lack of agreed upon definition for a valid reduction in post-concussion symptoms, they argued that the reduction found was significant due to the reduced symptom burden for participants. However, Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) found no significant difference between groups for either their primary (days to sustainable RTW at 12 months post injury) or secondary outcome measures (Hospital Anxiety and Depression Scale, Glasgow Outcome Scale - Extended and Patient’s Global Impression of Change). The authors suggest the lack of difference regarding RTW could be explained by the intervention resulting in excessive focus on symptoms and difficulties after concussion and negatively impacting RTW. The study design allowed for the GP to refer onto other specialties as required in the control group, thus, the participants may have received necessary treatment for their issues, similar to the intervention participants. Similarly, there were mixed results reported by Fotuhi et al. (Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020). They found significant improvement following intervention for several domains such as attention, cognitive flexibility, executive functioning, verbal and working memory, reaction time and sustained attention. Improved scores on the brain fitness calculator and concussion symptoms questionnaire were also found, however, there was no significant change for visual memory, processing speed and simple attention.
Quality appraisal results
There was no disagreement between reviewers for the CASP RCT checklists. The minimal difference initially found on two of the three AXIS tools was discussed and resolved. Only one of the six included studies met all criteria, an AXIS assessed study (Janak et al., Reference Janak, Cooper, Bowles, Alamgir, Cooper, Gabriel and Orman2017). The remaining two AXIS assessed studies met almost all criteria (missing two to three only); both lacking detail regarding non-response bias concerns, one not appropriately measuring risk factor and outcome variables, and one omitting whether ethics approval or consent were obtained (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020; Kenrick-Rochon et al., Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021). None of the RCTs assessed fully met the CASP criteria as ‘blinding’ was not possible for the interventions applied, however, this was the only factor lacking in the Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) RCT. Inability to ‘blind’ is a common difficulty in complex rehabilitation studies (Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019). Treatment allocation was blinded by Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) and Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) ‘blinded’ the statistician with respect to group allocation. Neither Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) or Vikane et al. (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) were able to report precisely on the contribution of the intervention due to variables present. See Tables 3 and 4 for full results of the quality appraisal.
Discussion
This systematic review highlights the current challenges of seeking and developing evidence for treatment of PPCS. Within the vast amounts of available literature on mTBI and concussion, only a small number of published research studies which specifically investigated the evidence for interdisciplinary treatment of PPCS in adults were identified. Overall, the studies found an interdisciplinary approach to be beneficial, however, the challenges of inherent heterogeneity, lack of clarity for definitions and diagnosis, and mixed results were apparent. These challenges are well documented in broader literature and are problematic for TBI research efforts (Kenzie et al., Reference Kenzie, Parks, Bigler, Wright, Lim, Chesnutt and Wakeland2018; Polinder et al., Reference Polinder, Cnossen, Real, Covic, Gorbunova, Voormolen and von Steinbuechel, N2018). Traditionally, RCTs are considered gold standard for research, however, this is being questioned for the heterogenous condition that is TBI or concussion. Research into rehabilitation, the context within which PPCS is commonly addressed, does not fit well with the use of RCTs either (Horn et al., Reference Horn, Corrigan and Dijkers2015). The strict controls required result in evidence based on select subpopulations which then limits translation back to the general population (Menon & Maas, Reference Menon and Maas2015). Systematic reviews of evidence within the TBI context have consistently resulted in determining a lack of high-quality research and evidence-based treatments or inability to analyse the significantly varied results (Arbabi et al., Reference Arbabi, Sheldon, Bahadoran, Smith, Poole and Agrawal2020; Heslot et al., Reference Heslot, Cogné, Guillouët, Perdrieau, Lefevre-Dognin, Glize and Azouvi2021; Möller et al., Reference Möller, Lexell and Wilbe Ramsay2021). Comparative effectiveness research (CER) has somewhat recently been suggested as an alternative. CER is ‘designed to inform healthcare decisions by providing evidence on the effectiveness, benefits and harms of different treatment options’, and utilising a variety of information sources and evaluating multiple treatments to determine outcomes more applicable to the real-world (Horn et al., Reference Horn, Corrigan and Dijkers2015, p. 174; Wheble & Menon, Reference Wheble and Menon2016). CER may be well placed to address the issue of evidence for TBI and rehabilitation.
The interdisciplinary interventions applied in all identified studies were found to reduce post-concussion symptoms across the symptom subtypes: headache/migraine, vestibular, cognitive, ocular motor and anxiety/mood (Lumba-Brown et al., Reference Lumba-Brown, Teramoto, Bloom, Brody, Chesnutt, Clugston and Ghajar2020; Rytter et al., Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019; Thastum et al., Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019). Improvements in physical health, illness perceptions, PTSD and depression were also reported (Fotuhi et al., Reference Fotuhi, Ebadi, Dwivedy, Miles, Yeom, Tittle and Nadeem2020; Janak et al., Reference Janak, Cooper, Bowles, Alamgir, Cooper, Gabriel and Orman2017; Thastum et al., Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019). These results are consistent with broader studies and current opinions expressed in literature, advocating that the complex and heterogenous nature of PPCS requires a multimodal approach utilising the specialist knowledge and skills from a variety of disciplines (Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021; Schneider, Reference Schneider2019). A study by Vargo et al. (Reference Vargo, Vargo, Gunzler and Fox2016) examined referral patterns in a concussion clinic and found allied health, such as Physiotherapy, Speech Pathology, Neuropsychology and Occupational Therapy, were regularly referred to, with referrals to more than one discipline occurring in approximately 15% of cases. Studies from various disciplines’ perspectives, such as Neuropsychology or Occupational Therapy, have argued the benefit of inclusion of their specific expertise (Caplain et al., Reference Caplain, Chenuc, Blancho, Margue and Aghakhani2019; Cooper et al., Reference Cooper, Bunner, Kennedy, Balldin, Tate, Eapen and Jaramillo2015; Harris et al., Reference Harris, Rafeedie, McArthur, Babikian, Snyder, Polster and Giza2019). A systematic review by Möller et al. (Reference Möller, Lexell and Wilbe Ramsay2021) found there may be benefits from multidimensional management and team-based interdisciplinary care compared with usual care. Bailey et al. (Reference Bailey, Meyer, Briskin, Tangen, Hoffer, Dundr and Smith2019) reported that their multidisciplinary concussion management programme demonstrated the need for multidisciplinary management and meaningful recovery from the programme. Clinical Practice Guidelines for rehabilitation in TBI strongly recommend an interdisciplinary approach, however, there has previously been limited evidence for the management of chronic symptoms in mTBI (Lee et al., Reference Lee, Amatya, Judson, Truesdale, Reinhardt, Uddin and Khan2019). This review contributes to addressing this by providing evidence for the interdisciplinary approach for PPCS.
The evidence from this review builds on a broader evidence base for interdisciplinary practice. It has been established as best practice in various healthcare domains such as quality and safety, rehabilitation, and stroke recovery (Bosch & Mansell, Reference Bosch and Mansell2015; Clarke & Forster, Reference Clarke and Forster2015; Singh et al., Reference Singh, Küçükdeveci, Grabljevec and Gray2018). As discussed previously, interdisciplinary practice is distinguished from multidisciplinary in that clinicians work collaboratively and there is overlap of roles (Singh et al., Reference Singh, Küçükdeveci, Grabljevec and Gray2018). Rytter et al. (Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle2019) emphasised the strong coordination and collaboration between clinicians for their specialised interdisciplinary rehabilitation (S-REHAB) treatment as a study strength. The interprofessional treatment provided to varsity athletes was noted to have improved from the first to second year with suggestion that this contributed to the improved results (Kenrick-Rochon et al., Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021). However, due to the complexity of the S-REHAB intervention, it was not possible to determine exactly how the interdisciplinary approach contributed to results, or if it was the intensity or ability to accommodate individual needs or a combination. Similarly, it was not clear in Kenrick-Rochon et al.’s (Reference Kenrick-Rochon, Quesnele, Baldisera, Laurence and Grenier2021) study what part the additional variables of increased clinician experience and revision of the protocol may have played in contributing to the positive results. Notably, the study by Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) provided detail regarding their successful intervention and could be reproduced to further strengthen the evidence base.
There has long been debate regarding the aetiology of the diverse range of concussion symptoms, however, more recently there is acknowledgement that complex interactions between both neurogenic and psychogenic factors contribute (Jaganathan & Sullivan, Reference Jaganathan and Sullivan2019; Prince & Bruhns, Reference Prince and Bruhns2017). A biopsychosocial perspective and more patient-centred approach is useful when evaluating and treating the patient’s individual needs, irrespective of aetiology, with focus on functional and meaningful goals (Jaganathan & Sullivan, Reference Jaganathan and Sullivan2019; Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021). Interdisciplinary intervention accommodates this comprehensive approach and yet also allows for individual needs. The study by Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) is significant in this respect as their intervention encompassed the biopsychosocial model, current established treatments, all symptom subtypes, was clinically achievable, adaptable for individual need and included representative participants. Thastum et al. (Reference Thastum, Rask, Naess-Schmidt, Tuborgh, Jensen, Svendsen and Schröder2019) also included illness perception and behaviour in their study and found the intervention resulted in larger reductions of these factors, as compared to usual care. Similarly, Janak et al., (Reference Janak, Cooper, Bowles, Alamgir, Cooper, Gabriel and Orman2017) highlighted the importance of an expectation of recovery and that this method can avoid reinforcing negative illness perceptions and reduce the likelihood of symptoms from comorbidities being misattributed to concussion. The focus on symptoms in Vikane et al.’s (Reference Vikane, Hellstrøm, Røe, Bautz-Holter, Aßmus and Skouen2017) study was suggested as possible explanation for a lack of difference for RTW days. Concerningly, it is possible for patients and clinicians to attribute all PPCS symptoms to concussion and minimise other causes such as stress or anxiety (Broshek et al., Reference Broshek, De Marco and Freeman2015). No PPCS symptoms are specific to PPCS. Assessment and treatment must therefore be comprehensive, considerate of the individual presentation and history and encompass the multiple contributing aetiologies (Quinn et al., Reference Quinn, Mayer, Master and Fann2018; Wilber et al., Reference Wilber, Leddy, Bezherano, Bromley, Edwards, Willer and Haider2021).
Translating results from these studies is challenged by the significant heterogeneity. Sports-related concussion and the military setting are unique contexts from which results can not necessarily be generalised (Cooper et al, Reference Cooper, Bunner, Kennedy, Balldin, Tate, Eapen and Jaramillo2015; Dayton et al, Reference Dayton, Baker, Sheth, Tjong and Terry2020). As compared to the civilian population, the military population has higher incidence of mTBI, PPCS and comorbidities such as PTSD, depression or chronic pain (Jones et al., Reference Jones, Harasym, Miguel-Cruz, Chisholm, Smith-MacDonald and Brémault-Phillips2021; McGlinchey et al., Reference McGlinchey, Milberg, Fonda and Fortier2017). Due to the significant variation, it was not possible to complete meaningful comparative analysis of the identified studies. Other than the concept of interdisciplinary intervention, there were no similarities between studies; neither in included disciplines, dosage, type, intensity or length of treatment, measures, or evaluation. Several studies lacked detail regarding the treatment provided. There are many critical factors to interdisciplinary intervention which remain unclear and require further research.
This systematic review provides an evidence base for health services and clinicians to reconsider traditional rehabilitation service design and action the establishment of interdisciplinary teams for treatment of PPCS. Interdisciplinary practice accommodates the need for a comprehensive approach, encompassing the need for a biopsychosocial perspective and complex interactions present with PPCS (Jaganathan & Sullivan, Reference Jaganathan and Sullivan2019; Mashima et al., Reference Mashima, Waldron-Perrine, MacLennan, Sohlberg, Perla and Eapen2021). This review also highlights for clinicians and researchers the importance of consistent definitions and language to facilitate high-quality research.
Limitations of the study
There are numerous limitations to this systematic literature review. Firstly, due to time constraints prescribed by the UNE it was necessary to limit the scope to ensure achievability. Secondly, as the search included only published studies from five databases it is possible that relevant studies from other sources may have been missed. Also, non-English articles were excluded. However, given the prominence of the selected databases, high number of duplicate reports identified, additional searching on Google Scholar and manual searching of reference lists, it is unlikely that many, if any, were missed. Thirdly, key terms for ‘collaborative’ were not included in the search, alongside interdisciplinary, which may have limited results. Fourthly, the review did not include children or adolescents as this was deemed beyond the scope of the review. Finally, the heterogenous nature of the identified studies significantly limited the possible analysis and ability to provide recommendations regarding an interdisciplinary approach to treatment of PPCS in adults.
Conclusion
Persistent symptoms from concussion affect a significant number of people each year, both in Australia and globally, with estimates of mTBI representing 80-90% of all TBI cases and PPCS eventuating in 15–30% of cases (Möller et al., Reference Möller, Lexell and Wilbe Ramsay2021). The impact of long-term symptoms on function and quality of life can be substantial. The present systematic review identified only a small number of studies, however, did confirm evidence for a reduction in PPCS following interdisciplinary intervention. This is consistent with the established evidence-base for interdisciplinary practice within healthcare and current Clinical Practice Guidelines for TBI rehabilitation (Lee et al., Reference Lee, Amatya, Judson, Truesdale, Reinhardt, Uddin and Khan2019; Morley & Cashell, Reference Morley and Cashell2017). The variance in study design, population, intervention and outcomes did not enable larger or more specific recommendations regarding interdisciplinary practice to be made. Long-term challenges for research into PPCS remain, including the lack of clarity in definitions and diagnosis, the heterogenous nature of the condition and subsequent mismatch with traditional research models. Current research, such as the Silverberg and Iverson led expert panel working to update the definition of mTBI, will likely provide useful progress regarding clarifying necessary definitions (Silverberg et al., Reference Silverberg, Iverson, Arciniegas, Bayley, Bazarian, Bell and Whitehair2021). With evidence suggesting the way forward is multimodal intervention with capacity and flexibility for individualisation, new perspectives on determining evidence and the ability to replicate quality studies provides hope that some of the challenges inherent in TBI research can begin to be addressed (Horn et al., Reference Horn, Corrigan and Dijkers2015; Jaganathan & Sullivan, Reference Jaganathan and Sullivan2019). This review provides a foundation for further research into persistent symptoms following concussion for adults.
Table 3. Quality appraisal of RCTs using the CASP RCT checklist
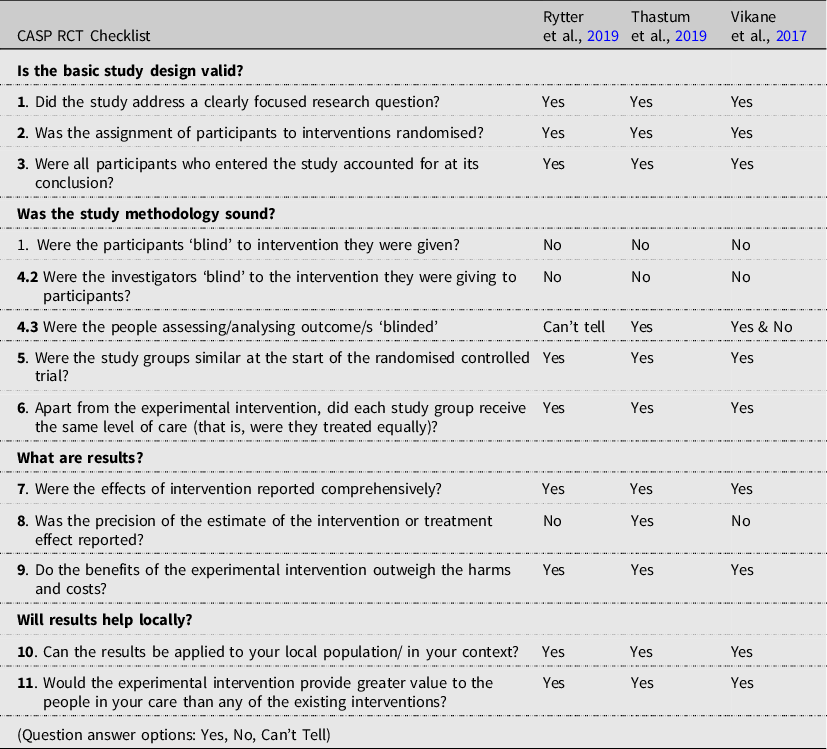
Table 4. Quality appraisal of non-randomised quantitative and cross-sectional studies using the Appraisal of Cross-Sectional Studies (AXIS)

Acknowledgements
The University of New England (UNE) database search and library guidance provided by the UNE library staff.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare no conflicts of interest.
Ethical standards
Not applicable.







