Dear Editor,
Psychiatrists, as much as other physicians, are for legal and ethical reasons obliged to inform their patients about risks and benefits of medical treatments (“risk communication”). In practice this implies, for e.g., psychiatrists explaining risks and benefits of different antidepressants to patients, also including information on the likelihood of these risks and benefits. In doing so, most psychiatrists communicate probabilities “verbally”, i.e., by using terms such as “likely”, “rare” or “often”. Despite the frequent use of these verbal expressions, it is to date unknown what psychiatrists actually mean when using them.
We surveyed psychiatrists attending the congress of the German Psychiatric Association held in November 2008 and asked participants what frequencies they mean when using 10 colloquial expressions for probabilistic information face to face with a patient suffering from depression/schizophrenia (Table 1). About 50% of the psychiatrists received these statements in a “depression” version (i.e., they were asked to imagine a depressed patient and talking about risks and benefits of an antidepressant) and the other 50% in a “schizophrenia” version (patient with schizophrenia, pros and cons of an antipsychotic). All participants were asked how many patients they meant with these statements (in percentage terms: “Of 100 patients, how many…?”), and they were requested for every item to specify a percent range (“__ % to __ %”).
Table 1 Psychiatrists’ perceptions (“from __ % to __ %”) of verbal expressions of probabilities.
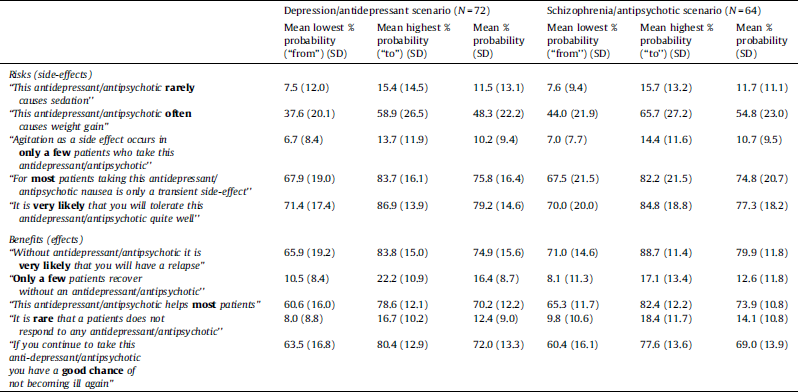
N = 143 psychiatrists (60 female, 83 male) participated in the study (age: M = 46.3 years). One hundred and fifteen psychiatrists were working in hospitals and 25 in private practice.
As can be seen from Table 1 and Fig. 1, the terms “most”, “often” etc. match an absolute risk of about 70–80% in the eyes of many psychiatrists, whereas the terms “rare”, “few”, etc. match 10–20%. There were no significant differences in psychiatrists’ ratings between the depression and the schizophrenia scenario. There was, however, considerable variation between individual psychiatrists’ perceptions of what frequencies are meant by these terms (Fig. 1).
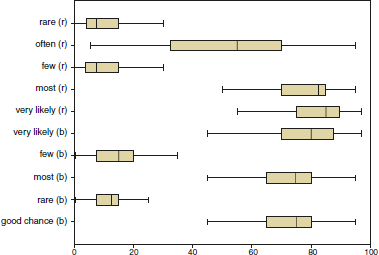
Fig. 1 Boxplots of psychiatrists’ ratings of verbal expressions of probabilities (means of ratings); (b = benefit, r = risk).
Looking at our results, patients can assume that many psychiatrists mean an absolute risk of 10–20% when talking about something that happens rarely or that affects few people and an absolute risk of about 70–80% for something happening often or affecting most people. While these numbers matched to certain verbal expressions might seem plausible, we believe these findings to be problematic for several reasons when looking at their possible impact on risk communication between psychiatrists and their patients.
First, there was considerable variation in the psychiatrists’ estimates. Thus, describing something as happening “often” can mean an absolute risk of 10 or 90%, depending on the individual doctor. Second, there might be a comparable amount of heterogeneity in the patients’ perceptions, too, making a congruence between the doctor's and the patient's perceptions unlikely. Finally, the psychiatrists’ perceptions of probabilities do not correspond to current conventions for package inserts (e.g. “very common”: ≥ 1/10; “common”: ≥ 1/100 to < 1/10, etc.). Thus it could happen that a doctor uses the term “rare” to mean 10–20% absolute risk, while the patient looking up the specific side-effect in the package insert finds the term “rare” meaning “< 1/1000”.
If, therefore, the psychiatrists’ use of verbal expressions for frequencies does not allow a reliable risk communication the validity of informed consent and the implementation of shared decision making Reference Hamann, Leucht and Kissling[3] are seriously threatened.
To foster insight of patients as well as congruence between patients’ and physicians’ perceptions, it has been recommended to account for characteristics of the evidence (e.g., magnitude of an effect, consistency of evidence) as well as for characteristics of the patient (e.g., desire for information, cognitive capacity) when presenting statistical evidence Reference Epstein, Alper and Quill[1]. One recommended way is the use of frequency statements in terms of absolute frequencies (e.g. “40 of 100 patients taking this drug…”) Reference Gigerenzer and Edwards[2]. Even more helpful might be the use of individualized or personalized risk communication (i.e., information is tailored to a patient's personal risk status) but evidence is often too poor to allow for this approach. Finally, the adoption of graphical tools Reference Kurz-Milcke, Gigerenzer and Martignon[4] (e.g., population diagrams) or the implementation of decision aids [5] might help patients reaching at informed decisions.
Future efforts to improve risk communication in psychiatry have to address two major fields: making sound data available as a basis for good risk communication, and teaching as well as assisting psychiatrists in risk communication.





Comments
No Comments have been published for this article.