Traditionally, telepsychiatry has been practised as a method of delivering care to hard-to-reach populations.Reference Hassan and Sharif1 A number of publications have demonstrated both its effectiveness and its acceptability.Reference Hilty, Yellowlees, Parrish and Chan2 To accommodate the practice, the American Psychiatric Association (APA) has had guidelines for telepsychiatry for some years.Reference Von Hafften3 Australia has similar guidelines, as does the Royal College of Psychiatrists.4,Reference Von Hafften5 The APA concluded that ‘Telepsychiatry is equivalent to in person care, in diagnostic accuracy, treatment effectiveness, and patient satisfaction. It saves time, money and other resources, while patient confidentiality parallels in-person care’.Reference Von Hafften5 On 17 March 2020, the APA issued further guidelines to enable easier access to telepsychiatry.6 On 31 March 2020, following the swift transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA these guidelines made social distancing an obligation for the clinician. The APA did recognise that videoconferencing may not be ideal in the course of routine care, but in the current times of the pandemic it was deemed essential. Europe had a similar response, with Public Health England strongly urging the use of technology to offer virtual ward rounds to those over 70, the pregnant and those with pre-existing medical conditions. The COVID-19 pandemic has undoubtedly increased the urgency of exploring telepsychiatry in sub-Saharan Africa and specifically in Kenya.Reference Adepoju7,Reference Jaguga and Kwobah8 However, as practitioners rush to implement mental healthcare on a virtual platform, few papers from sub-Saharan Africa describe this experience in a care setting. This case study seeks to address this gap.
Case study
Effect of the pandemic on mental health service provision in Kenya
Following the declaration of the COVID-19 pandemic on 21 March 2020, the world order changed in a way not seen before. In Kenya, rural and urban residents were separated from their mental health providers as social distancing became the new norm. Face-to-face consultations were not only impossible to achieve following the lockdowns but they were also discouraged.
Kenya at the time did not have a regulatory framework for telemedicine but in response to the dictates of the pandemic, the Medical Practitioners and Dentists Council was able to license qualified applicants within 48 hours of application. Chiromo Lane Medical Centre was granted a licence on 5th May 2020 to practice virtual medicine and thus formalised a practice it had been forced into by the pandemic.
The setting
Chiromo Lane Medical Centre (now Chiromo Mental Health Hospital) was established in 1997 by a group of mental health workers who saw the growing mental health needs of Kenyans needing delivery of care in a dignified and private setting. It is a private healthcare facility that primarily serves the large and growing fee-paying middle class. It has 160 beds, and serves both in- and out-patients in three locations in the city of Nairobi. Thirty psychiatrists have admitting rights to the hospital and all are computer literate to varying degrees. Its main catchment area is Nairobi and the surrounding counties, but patients from the East African region are also seen regularly.
The challenge
The first case of COVID-19 was reported in Kenya on 13 March 2020. The Kenyan government had anticipated the arrival of the virus as Nairobi and Mombasa are major air transport hubs. In the early stages, all the reported infected cases were imported, with all having a recent history of air travel. Local transmission was officially reported on the 15 March.Reference Muraya9 The government response was swift and decisive and 2 days later, schools, universities and places of worship were closed in quick succession. Subsequently, restriction of movement orders were issued under the Public Order Act and Nairobi and Mombasa Counties were inaccessible to the rest of the country.Reference Kagwe10 A number of other counties were also put in lockdown, as were some areas within the cities of Nairobi and Mombasa, where transmission was noted to be rapidly increasing. This sudden cessation of movement caught many Kenyans off guard. Many were away from their usual place of residence, and still others were far from their mental health providers.
The crisis
The response to the pandemic had unforeseen medical consequences. Patients lacked access to usual medical care. Calls were received from patients who had appointments they could not keep, and others were short on medication. The risk of relapse of stable patients was increasing by the day and the institution had to respond urgently. The stress associated with the pandemic, especially the social distancing and lockdown measures, also seemed to fuel the demand for new mental health consultations.
The opportunity
That the hospital serves the greater East African region meant that treating patients remotely had been discussed once in a while but never seriously. The pandemic brought this matter back on to the table. One of the authors had used Zoom for non-medical teleconferencing and, in the absence of any other alternative, the decision to implement the new technology was made. The teams involved took the challenge and within a few days, remote consultations became the norm for a number of specialists. The first patient was seen via zoom on 7 April 2020. To the surprise of all, the call went without incident and all concerned seemed happy that the first day went without a hitch and patients and medical staff expressed a sense of relief that work was continuing in the novel situation. Then the problems started. At first the problems were related to the technology itself. The phones and computers used proved inadequate for the purpose and so new hardware was quickly purchased. The bandwidth proved to be inadequate in the area and a new provider was identified and things gradually improved.
Staff training
It was thought that training staff to use and get accustomed to the new technology would pose a significant problem. This turned out to be the least of our problems. The age range of the staff involved was between 18 and 70 years and all had worked with social media in one form or another. All took to the technology easily and were able to master all the functions necessary for safe and confidential consultations very easily. Having identified a team leader for the actual training, a small group received direct training, and they then trained the rest of the team. All the nurses and psychologists were technology literate and were able to set up and run in- and out-patient consultations.
Mental health workers
The groups of mental health workers involved in this work were all associated with CLMC and reported prior exposure to the use of technology. Doctors, nurses and psychologists played different roles in the delivery of care. For the delivery of in-patient care, the nurses and psychologists worked in weekly shifts (to reduce the risk of infection) at the hospital, and the doctors worked remotely doing their ward rounds. A designated nurse kept the notes during the consultations, and the treatment plans were discussed and agreed by the teams in the usual way. Out-patient appointments were scheduled by the psychologists and patients were seen either at the hospital or at home. All mental health workers expressed satisfaction with the use of technology to deal with this emergency.
Strength of the response
The team was faced with a unique health crisis, the nature of which had not been seen before. The choices presented were bleak and involved interruption of healthcare delivery to a most vulnerable population. It involved the demonstration of creativity and team work and different team members spent many hours of research in diverse areas, including IT and regulatory frameworks as well as improvements to the experience of the technology by both therapist and patient. It was possible to build in lessons as we went along, without the restriction that would have been placed by a protocol.
Results
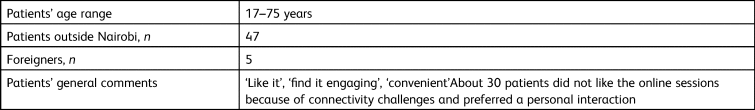
Tables 1 and 2 give general data on the implementation of telepsychiatry at the facility for the period from 7 April to 30 June 2020.
Table 1 Telepsychiatry at the Chiromo Lane Medical Centre, 6 April to 30 June 2020
Table 2 Patient demographics and comments on telepsychiatry
Limitations of the intervention
This was a single-centre initiative that took place in a middle-class urban setting during a most unusual global crisis. However, the high mobile phone penetrance and internet access in the countryReference Kemp11 speaks to the feasibility of scale up of telepsychiatry services in both public and private settings in Kenya. It might not be possible to replicate the findings in the absence of these characteristics. The short duration of the work also makes it possible that during future follow-up some of the benefits observed in both the patients and the mental health works could be lost.
Lessons learned
Many lessons were learned and some continue as challenges whereas others present unique opportunities for the practice of mental healthcare in Africa. This intervention has demonstrated that it is possible in an African country to rapidly shift platforms in a clinic setting. The response put in place did not have to be perfect but it had to address the greatest concern, which in our case was the continuation of care. We also learned the importance of resilience and the effectiveness of working in teams. The fear of technology was overcome by taking technophobic members of the team gently and most importantly identifying which team member had the best chance of helping those not familiar with technology. The other lesson was that our population could adapt to new ways of healthcare delivery in a short time. The importance of ensuring that we had the right training and equipment became obvious with time. It also became evident that geographical limitations can be overcome in an African setting via technology.
Conclusions
The COVID-19 pandemic has proved to be a major challenge to humanity and in its wake society has had to adapt in ways that none had foreseen. Nevertheless, the pandemic seems to have opened up avenues not considered before and made possible by the relatively high penetration of technology on the continent. This case study demonstrates not only the high level of adaptability of providers but also high levels of acceptability of technology in a crisis. Future studies measuring the effectiveness and acceptability of telepsychiatry in both private and public settings in Africa are warranted.
Acknowledgements
We thank the mental health providers and patients of the Chiromo facility.
Author contributions
F.N. prepared the first draft. L.O., A.N. and L.A. edited the first draft and final versions of the manuscript. All other authors provided data and reviewed the manuscript and approved the final version of the manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.






eLetters
No eLetters have been published for this article.