A dietary supplement (DS) is defined as a vitamin, a mineral, an herb or other botanical, an amino acid, a nutritional substance intended for ingestion to supplement the diet by increasing the total dietary intake, or a concentrate, metabolite, constituent, extract or combination of any ingredient described(1). As socio-economic status improves, DS use becomes increasingly prevalent among children and adolescents in developed countries to compensate for nutritional deficits, improve health conditions and prevent diseases(Reference Yoon, Park and Kang2,Reference Park and Lee3) . For instance, nearly one-third of infants, children and adolescents use DS in the USA(Reference Bailey, Gahche and Thomas4–Reference Jun, Cowan and Tooze6), mostly in the form of multivitamin–minerals(Reference Bailey, Gahche and Thomas4–Reference Jun, Cowan and Tooze6). The use of DS was reported to be associated with higher income, higher household food security levels and higher household education levels in the USA(Reference Jun, Cowan and Tooze6).
While public interest in DS use among children has increased, studies on the prevalence and related factors in paediatric DS use are scarce, worldwide, except for in the US Research on DS use in the Korean paediatric population is also extremely limited and is mostly limited to specific regions and age groups(Reference Kang, Kim and Jung7). This study aimed to investigate the prevalence of each type of DS through all age groups and the related factors affecting the habits of DS use among Korean children and adolescents, using the most recent nationally representative data.
Methods
Subject
The data were collected from the Korean National Health and Nutrition Examination Survey (KNHANES), conducted by the Korea Centers for Disease Control and Prevention between 2015 and 2017. The study population was confined to subjects aged 1–18 years, who completed a 24-h food recall questionnaire during the survey. The 24-h food recall questionnaire included the type and product name of the DS consumed by the subjects over the past 24 h, the amount of single use and the frequency of DS intake during the day. Participants without anthropometric measurements were excluded. After exclusion, a total of 4380 children and adolescents aged 1–18 years (1777 boys and 1665 girls) were enrolled in this study.
Data collection and study variables
The weight and height of the participants were measured using a digital weighing scale and a stadiometer to the nearest 0·1 kg and 0·1 cm, respectively. BMI was calculated by dividing body weight (kg) by the square root of height (m). For subjects aged ≥2 years, BMI status was grouped into three groups according to the sex and age-specific BMI percentile(Reference Kim, Yun and Hwang8): normal (<85th percentile), overweight (≥85th percentile and <95th percentile) and obese (≥95th percentile). Height status was organised into three groups according to the sex and age-specific height percentile(Reference Kim, Yun and Hwang8): short (<15th percentile), average (≥15th percentile and <85th percentile) and tall (≥85th percentile).
The household income group was categorised according to the quartile values of equalised household income. Birth weight (kg) and feeding patterns during infancy (breast-feeding, formula feeding and mixed feeding) were surveyed in subjects under 4 years of age. Birth weight was organised into three groups: <2·5 kg, 2·5–3·9 kg, ≥4·0 kg. Participants who had a history of atopic dermatitis, asthma and CHD were defined as having chronic diseases. There were no participants who reported other chronic diseases, such as cancer, hypothyroidism, diabetes mellitus and hepatitis.
Whether or not the subject typically used the nutrition facts label was surveyed only in participants over 10 years old. The frequency of weekly breakfast intakes was divided into three groups: 0–2, 3–4 and 5–7 times/week.
Statistical analysis
The statistical analyses were performed using SPSS version 25.0 (SPSS, Inc.). Sampling weights were used to consider the complex, multistage, probability sampling design for all analyses. The Complex Samples General Linear Model was used to calculate the mean and se of the scale variables, and the Complex Samples Crosstab procedure was used for categorical or ordinal variables. The Complex Samples Logistic Regression procedure was used to identify demographic and dietary habits (OR and 95 % CI) associated with DS use. P-values were two-tailed for all analyses, and a P-value of <0·05 was considered significant.
Results
The prevalence of dietary supplements
The overall prevalence and types of DS use in subjects are presented in Fig. 1. A total of 20·3 % of children and adolescents used DS. The most consumed DS was probiotics and prebiotics (26·9 % of all DS use), with similar proportions of multivitamin/mineral supplements consumed (25·9 %). Other DS, which included miscellaneous types of botanical supplements, Fe and propolis, accounted for 124 % of all DS types. As a single nutrient, vitamin C and n-3/fish oil accounted for 6·9 %, vitamin D for 5·9 %, Ca and Zn for 3·8 % and red ginseng extract for 3·1 %.

Fig. 1 The prevalence and types of dietary supplement use among Korean children and adolescents. ![]() , 26·9 % Pro/prebiotics;
, 26·9 % Pro/prebiotics; ![]() , 25·9 % multivitamin/mineral supplements;
, 25·9 % multivitamin/mineral supplements; ![]() , 12·4 % others (botanical supplements, iron etc.);
, 12·4 % others (botanical supplements, iron etc.); ![]() , 11·4 % vitamin C;
, 11·4 % vitamin C; ![]() , 6·9 % ω-3/fish oil;
, 6·9 % ω-3/fish oil; ![]() , 5·9 % vitamin D;
, 5·9 % vitamin D; ![]() , 3·8 % calcium;
, 3·8 % calcium; ![]() , 3·8 % zinc;
, 3·8 % zinc; ![]() , 3·1 % red ginseng
, 3·1 % red ginseng
Types of dietary supplement by age group
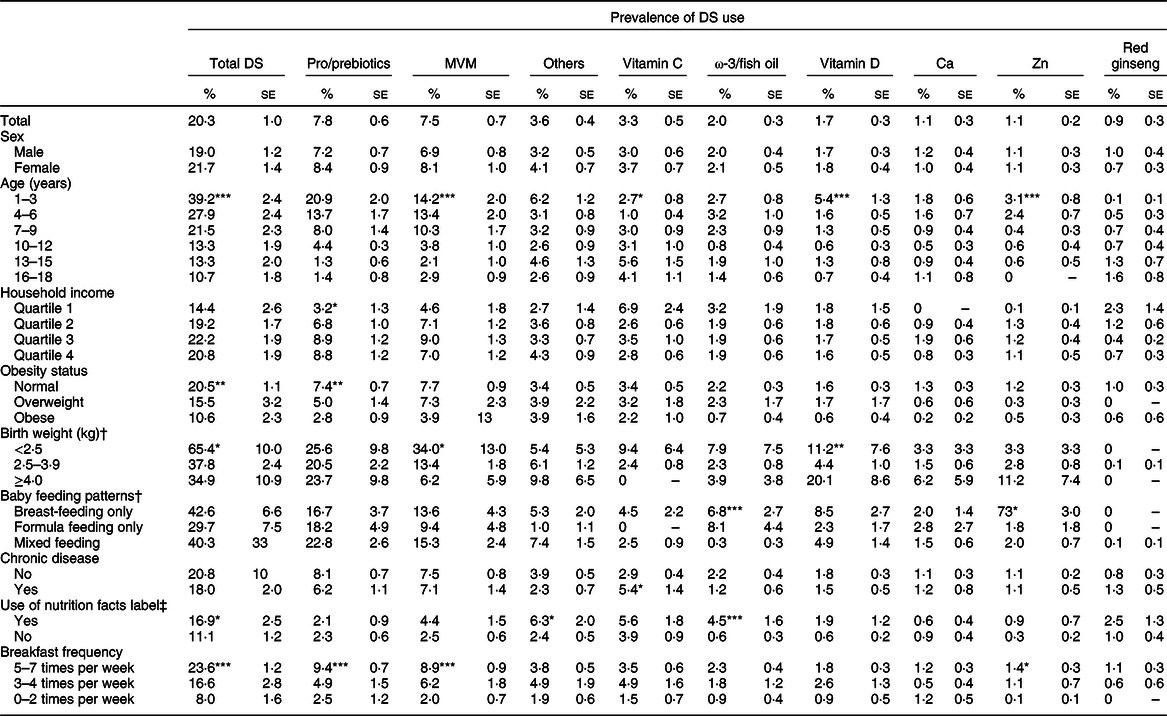
The prevalence of DS use by age group and DS types is presented in Fig. 2. Total DS intake was 39·2 % at 1–3 years old, 24·8 % at 4–9 years old and 12·3 % at 10–18 years old. In the 1–3-year-old age group, the most commonly used DS was probiotics and prebiotics (20·9 %), followed by multivitamin/mineral supplements (14·2 %), and others (6·2 %). In the 4–9-year-old age group, multivitamin/mineral supplements (119 %) were used most frequently, followed by probiotics and prebiotics (10·9 %) and others (3·1 %). Whereas in the 10–18-year-old age group, the most commonly used DS was vitamin C (4·3 %), followed by others (3·2 %), and multivitamin/mineral supplements (2·9 %).
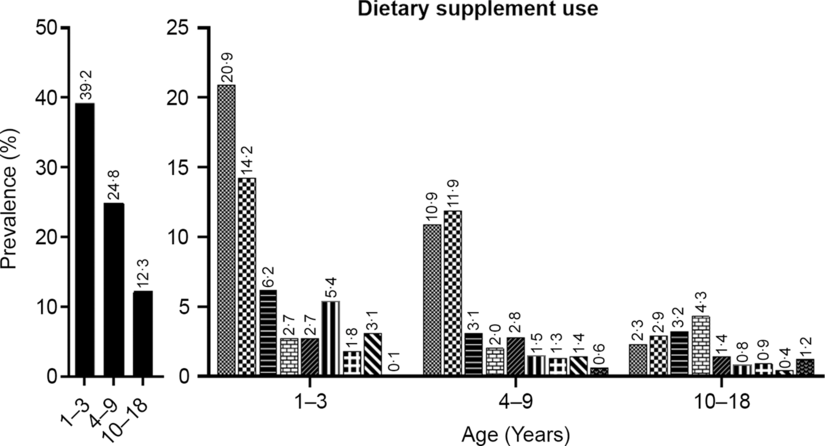
Fig. 2 Types of dietary supplement use by age group. ![]() , Any dietary supplements;
, Any dietary supplements; ![]() , pro/prebiotics;
, pro/prebiotics; ![]() , Multivitamin/mineral;
, Multivitamin/mineral; ![]() , others including botanical supplements, Fe and propolis;
, others including botanical supplements, Fe and propolis; ![]() , vitamin C;
, vitamin C; ![]() , ω-3/fish oil;
, ω-3/fish oil; ![]() , vitamin D;
, vitamin D; ![]() , calcium;
, calcium; ![]() , zinc;
, zinc; ![]() , red ginseng
, red ginseng
General characteristics of the study participants
The general characteristics of the study participants are presented in Table 1. The mean age of DS users was statistically significantly younger than that of non-users and was 7·5 and 9·0 years old, respectively (P < 0·001). The proportion of participants who were under 6 years of age was higher in DS users (50·9 %), compared with non-users (26 %). There were no significant differences in the proportions of sex, household income, height status and chronic disease status according to DS use. A lower prevalence of obesity in DS users was noted, compared with non-users (5·6 % v. 11·2 %, P < 0·001). About three times higher proportion of low birth weight in subjects under 4 years of age was found in DS users than in non-users (9·0 % v. 3·1 %, P = 0·023). However, there were no significant differences in feeding patterns in infancy according to DS use. DS users were more likely to use nutrition facts labels (29·8 % v. 20·6 %, P = 0·035) and more likely to eat breakfast at least five times a week, compared with non-users (84·5 % v. 69·6 %, P < 0001).
Table 1 General characteristics of the study population

DS, dietary supplement.
* Birth weight and feeding patterns during infancy were surveyed in the subjects <aged 4 years.
† Use of nutrition facts label was surveyed in subjects aged ≥10 years.
The types of dietary supplements consumed by the study subjects according to the subjects’ characteristics
Adjusted proportions of DS types consumed by the study population, according to the demographics and lifestyles, are presented in Table 2. Younger participants consumed more multivitamin/mineral supplements, vitamin D and Zn than older participants. The only DS type intake that increased with age was vitamin C. Although most of the DS types were consumed more in the normal-weight subjects than in the obese subjects, pro/prebiotics was the only DS type that showed a statistically significant difference according to obesity status. The subjects who were born with low birth weight showed as high as 65·4 % of the total DS use and demonstrated higher use of multivitamin/mineral supplements and vitamin D than those without low birth weight. n-3/fish oil supplement use was significantly more prevalent in the breast-/formula feeding group than in the mixed feeding group. In contrast, Zn supplement use was significantly higher in the breast-feeding group than the other feeding pattern groups. Multivitamin/mineral and vitamin D supplements were also more frequently used in the breast-feeding group, compared with the formula or mixed feeding group, which was not statistically significant. The vitamin C intake rate was significantly higher in children and adolescents with chronic diseases than in those without chronic diseases, while the total DS use rate was not significantly different among these groups. The type of DS that showed higher intakes in adolescents who check the nutrition facts labels was n-3/fish oil and other supplements. Subjects who had breakfast more than five times a week showed significantly higher use of pro/prebiotics, multivitamin/mineral supplements and Zn than those who did not.
Table 2 Types of dietary supplements consumed by Korean children and adolescents
DS, dietary supplement; MVM, multivitamin/mineral supplements.
*P < 0·05, **P < 0·01, ***P < 0·001. CSTABULATE was conducted to compare the prevalence of dietary supplements uses within the variables.
† Birth weight and feeding patterns during infancy were surveyed in subjects < aged 4 years.
‡ Use of nutrition facts label was surveyed in subjects aged ≥10 years.
Factors associated with DS use
Independent predictors (OR (95 % CI)) associated with DS use, according to the age groups, are presented in Figure 3. In children aged < 4 years, a history of low birth weight was the only significant factor associated with DS use (3·38 (95 % CI 1·47, 7·77)). In children aged 4–9 years, higher household income (Q3, 3·31 (95 % CI 1·28, 8·55); Q4, 2·62 (95 % CI 1·01, 6·84)) and higher breakfast frequency (3–4/week, 3·24 (95 % CI 1·10, 9·50); 5–7/week, 3·30 (95 % CI 1·35, 8·11)) were significant predictors for DS use. On the other hand, older age (0·87 (95 % CI 0·80, 0·95)) and obesity (0·48 (95 % CI 0·23, 0·97)) were found to be factors of decreased use of DS. For adolescents aged 10 years and older, higher breakfast frequency (5–7/week, 2·72 (95 % CI 1·31, 5·66)) and use of nutrition facts labels (1·58 (95 % CI 1·05, 2·38)) were identified as predictors associated with DS use.
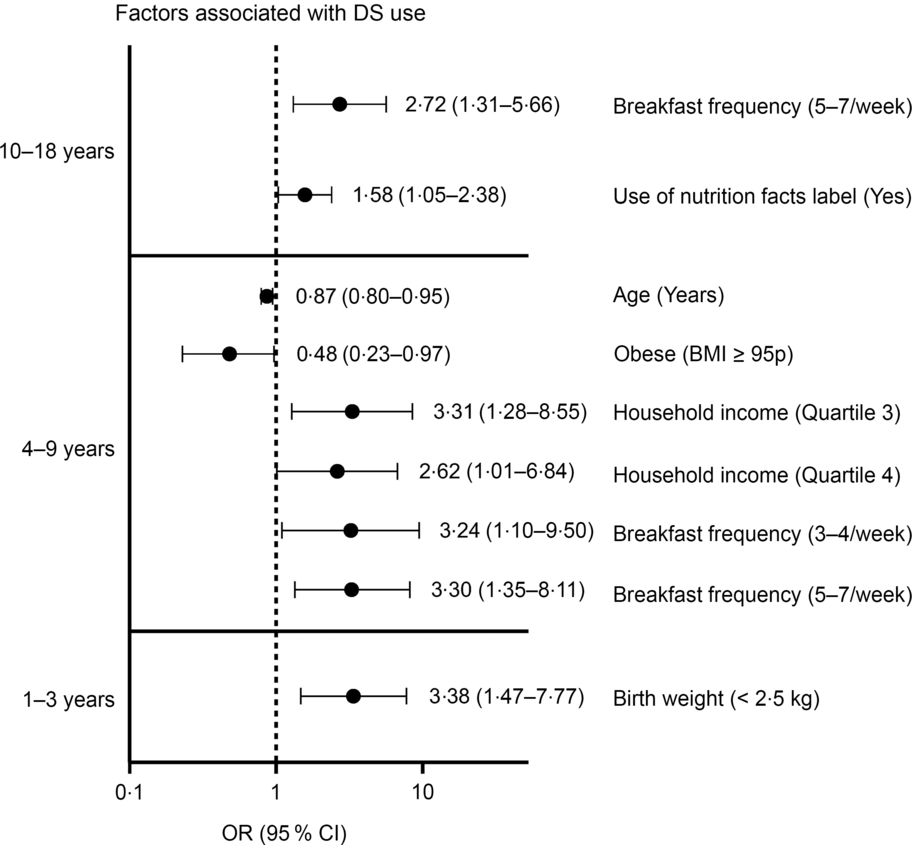
Fig. 3 Factors (OR and 95 % CI) associated with dietary supplement use. For aged 1–3 years, covariates include age, sex, quartiles of household income, baby feeding patterns (breast-feeding only, formula feeding and mixed feeding), chronic disease (yes v. no) and breakfast frequency (0–2, 3–4, 5–7 times/week). For aged 4–9 years, covariates include sex, chronic disease (yes v. no). For aged ≥ 10 years, covariates include sex, quartiles of household income and chronic disease (yes v. no). References: sex = boys, household income = quartile 1, birth weight ≥ 2·5 kg, baby feeding patterns = breast-feeding only, chronic disease = no, breakfast frequency = 0–2 times/week, obesity status = obese (BMI ≥ 95 percentile), use of nutrition facts label = no
Discussion
In this study, we assessed the prevalence of DS use in children and adolescents in Korea. The DS intake rate of Korean children and adolescents was about 20 %; the highest was 39 % in 1–3 years old, and the lowest was 12 % in teenagers. The highest intakes were pro/prebiotics and multivitamin/mineral supplements, followed by other DS, including botanical supplements, Fe and propolis. DS intake was associated with low birth weight at age 1–3 years; younger age, higher income, regular breakfast intake and lower BMI at age 4–9 years; and regular breakfast intake and use of nutrition facts labels at age 10–18 years.
In a previous study that used data from the KNHANES 2007–2009, DS use in the Korean paediatric population was about 34 %(Reference Yoon, Park and Kang9), which is significantly higher than that in our findings (20·3 %) from the KNHANES 2015–2017. Of note, the DS questionnaire conducted in the 2007–2009 survey was based on DS taken over the last 2 weeks, while that of the 2015–2017 survey was based on the 24-h food recall. Therefore, the lower DS use in the 2015–2017 survey compared with the 2007–2009 survey is likely due to the irregularity of DS use, rather than an actual decrease in DS use in this population. Furthermore, we found that DS use in toddlers was similar to that found in the previous study (40 %)(Reference Yoon, Park and Kang9), but among teenagers, DS use decreased considerably from 23 % to 12 %. These findings might be due to the irregularity of DS use among teenagers, compared with toddlers who are regularly provided with DS by their caregivers. Although a direct comparison is difficult due to the difference in age and survey method of DS use, the prevalence of DS use in this study was similar to that in Japan (8·0–20·4 %) and Germany (25·8 %), while lower than that in the USA (27–34·2%), UK (39 %) and Canada (42·5 %)(Reference Bailey, Gahche and Thomas4–Reference Jun, Cowan and Tooze6, Reference Bell, Dorsch and Mccreary10–Reference Shaikh, Byrd and Auinger15).
Pro/prebiotics was the most commonly used DS by Korean children and adolescents. In particular, there was a high rate of pro/prebiotics use in toddlers aged 1–3 years. Pro/prebiotics are commonly used to treat constipation, acute infectious diarrhoea and antibiotics-associated diarrhoea and to prevent atopic dermatitis(Reference Ball, Kertesz and Moyer-Mileur16). However, the evidence of optimal form, number and strain of viable microbes of pro/prebiotics to reap the expected health benefits is weak(Reference Dalli, Uprety, Rakshit, Roos and Livney17). Also, there is a stability issue in which the number of microbes should be maintained during the product’s distribution period. Therefore, consumers should be careful to choose appropriate products that are permitted by the ministry of food and drug safety.
The second most consumed DS product among the Korean paediatric population was multivitamin/mineral supplements. Multivitamin/mineral supplements have been reported to contribute to increase the total daily intake of vitamins and minerals in adolescents(Reference Shaikh, Byrd and Auinger15,Reference Dwyer, Garceau and Evans18) . However, reckless DS use should be avoided for adolescents who are well-nourished because of the risk of an overdose of fat-soluble vitamins or minerals. In this study, DS users reported more regular breakfast intake and the use of nutrition facts labels, suggesting that there is a higher risk for overnutrition in DS users.
Moreover, children and adolescents have different nutritional needs, depending on the particular disease or health condition they possess(Reference Shaikh, Byrd and Auinger15). For example, breast-feeding infants and premature infants have increased vitamin D and Fe requirements(Reference Butte, Fox and Briefel19), and individuals with obesity have increased pyridoxine, vitamin D and Fe requirements(Reference Xanthakos20). However, in this study, most toddlers who underwent breast-feeding were not taking multivitamins or vitamin D supplements. Also, an extremely low percentage of children with obesity were using multivitamins and vitamin D supplements. In adolescence, the demand for Ca, Fe and Zn increases with rapid growth(Reference Butte, Fox and Briefel19). Therefore, DS use might be helpful to adolescents who often skip meals or those who are not provided with nutritionally sufficient meals because of their low socio-economic status. However, our study found that adolescents who eat breakfast regularly, have an interest in nutrition facts labels and those who are in a higher socio-economic status tend to consume DS more. This finding was consistent with a previous study based on the 2007–2009 survey(Reference Yoon, Park and Kang2) and other studies from the USA(Reference Bailey, Gahche and Thomas4–Reference Jun, Cowan and Tooze6,Reference Shaikh, Byrd and Auinger15) and Thailand(Reference Chen, Lin and Kao21,Reference Chuang, Yang and Chang22) . These results warrant the demand for public education on proper DS use in children and adolescents according to their nutritional condition.
In this study, we reported that a low birth weight under 2·5 kg is the main predictor of DS use in Korean toddlers. To the best of our knowledge, this is the first study to demonstrate the overall prevalence of DS use and DS types according to toddlers’ birth weight. Nearly 65·4 % of the Korean toddlers born with low birth weight were using DS, and the major DS types for these children were multivitamin/mineral and vitamin D supplements. Since preterm babies or those born with low birth weight have high requirements for Fe and vitamin D(Reference Agostoni, Buonocore and Carnielli23), we assume that their relatively high DS intakes were a result of a medical provider’s recommendations.
We acknowledge the following limitations of this study. First, since the KNHANES data are cross-sectional, analyses of DS use with the associated factors in the KNHANES cannot presume causality, but only an association. Second, the DS survey in the 2015–2017 KNHANES was conducted as part of a 24-h food recall, not as a long-term DS questionnaire. Therefore, there is a possibility that the prevalence of DS use might be underestimated. Notwithstanding these limitations, the results of this study offer guidance to health care providers on the extent of data gathering and counselling needed regarding DS use. Our study used the latest nationwide data to outline the current state of DS use for the Korean paediatric population of all ages. Moreover, we included various covariates, including BMI, socio-economic status, lifestyle factors, infantile feeding patterns, that are potentially related to DS use.
Conclusion
In conclusion, over 20 % of the Korean paediatric population take DS, and pro/prebiotics and multivitamin/mineral supplements were the most commonly used DS. Younger age, lower BMI status, low birth weight, use of nutrition facts labels and regular breakfast intake were associated with DS use in this study. Since DS use in children with sufficient nutrition can lead to nutritional imbalances or adverse health outcomes, health care providers need to guide caregivers to provide appropriate DS that meets the children’s nutritional needs.
Acknowledgements
Acknowledgements: We would like to thank the Korean Ministry of Health and Welfare for providing raw data from the fourth Korea National Health and Nutrition Survey. Financial support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: S.H.K. and M.J.P. were responsible for the conception and design of the study. S.H.K. performed data analysis, and all authors had a role in the interpretation of the data. J.H.J. drafted the manuscript, and M.Y.S., S.H.K. and M.J.P. revised and commented on the draft. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving study participants were approved by the Institutional Review Board (IRB) of the Korea Centers for Disease Control and Prevention (IRB no. 2013-07CON-03-4c, 2013-12EXP-03-5C). Written informed consent was obtained from all subjects.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980020003419








