Intimate partner violence (IPV) – defined as physical, psychological, or sexual violence inflicted by a current or former intimate partner – is a pervasive social concern affecting over one third of all women in the United States (World Health Organization, 2013). Estimates suggest that of the millions of children and adolescents in the U.S. who live in a home where IPV has occurred, 80% or more are direct eyewitnesses to violent events (Finkelhor et al., Reference Finkelhor, Turner, Shattuck and Hamby2013; Graham-Bermann et al., Reference Graham-Bermann, Lynch, Banyard, DeVoe and Halabu2007). The deleterious consequences of IPV exposure for youths’ mental health, social development, physical health, and academic performance are well documented (Bender et al., Reference Bender, McKinney, Schmidt-Sane, Cage, Holmes, Berg, Salley, Bodell, Miller and Voith2022; Cage et al., Reference Cage, Kobulsky, McKinney, Holmes, Berg, Bender and Kemmerer2021; Holmes et al., Reference Holmes, Berg, Bender, Evans, Kobulsky, Davis and King2022; Vu et al., Reference Vu, Jouriles, McDonald and Rosenfield2016), and evolutionary theories suggest that IPV exposure may prompt adaptation processes that are functional in the context of IPV, but that engender liabilities that are shared across other life domains. That is, IPV exposure – like other forms of early adversity (McLaughlin et al., Reference McLaughlin, Colich, Rodman and Weissman2020) – may initiate alterations in processes that are critical for child and adolescent development “across the board,” including their psychological, academic, and social adjustment.
Seminal work examining processes that explain links between youths’ IPV exposure and life outcomes has emphasized changes that occur at the level of the individual, or within the children and adolescents themselves, such as alterations in bioregulatory stress response systems (Berg et al., Reference Berg, Evans, Powers, Moore, Steigerwald, Bender, Holmes, Yaffe and Connell2022) or shifts in social information processing and learning mechanisms (McLaughlin et al., Reference McLaughlin, Colich, Rodman and Weissman2020). This body of literature has illuminated a host of potential intervention targets for IPV-exposed youth, and yet, there remain opportunities to understand the reach of IPV’s effects to include environments outside of developing individuals themselves. A core assumption of bioecological theory (Bronfenbrenner & Morris, Reference Bronfenbrenner, Morris, Damon and Lerner1998) is that children and adolescents develop within nested environments at increasing proximity to the individual, in which transactions among environments interact to shape one’s development (Bronfenbrenner & Evans, Reference Bronfenbrenner and Evans2000). IPV exposure is a form of adversity that inherently implicates disruption in other environments that are key for youths’ adaptive adjustment, including the functioning of primary caregivers. Notable research has identified bidirectional processes through which IPV-exposed mothers’ functioning influences their children’s mental health (Galano et al., Reference Galano, Grogan-Kaylor, Stein, Clark and Graham-Bermann2020; Wadji et al., Reference Wadji, Ketcha Wanda, Wicky, Morina and Martin-Soelch2022); however, links among IPV, caregiver functioning, and transdiagnostic risk processes in children and adolescents have been underexplored. To this end, the present study compared co-occurring trajectories of caregiver depressive symptoms and child/adolescent effortful control (EC) – a competency that has been identified as a transdiagnostic risk mechanism for various forms of psychopathology (Lynch et al., Reference Lynch, Sunderland, Newton and Chapman2021; Santens et al., Reference Santens, Claes, Dierckx and Dom2020) and is associated with a broad range of adaptive life outcomes including academic performance, interpersonal functioning, and reduced risk for psychopathology (Hankin et al., Reference Hankin, Davis, Snyder, Young, Glynn and Sandman2017; Shields et al., Reference Shields, Reardon, Brandes and Tackett2019; Snyder et al., Reference Snyder, Gulley, Bijttebier, Hartman, Oldehinkel, Mezulis, Young and Hankin2015) – between children and adolescents who have been exposed to IPV (IPV+) and children and adolescents who have not (IPV−).
Effortful control
EC is an aspect of temperament that comprises one’s conscientiousness, attention to detail, inhibitory control, and ability to activate nondominant responses (Rothbart & Bates, Reference Rothbart, Bates, Eisenberg, Damon and Lerner2006). EC is an individual-difference characteristic that exhibits both stability and change over time, as individuals’ EC can be influenced by life experiences (Inzlicht et al., Reference Inzlicht, Werner, Briskin and Roberts2021). Evolutionary theories indicate that self-regulatory abilities like EC develop in ways that are meant to enhance context-specific evolutionary fitness (Cabeza de Baca & Ellis, Reference Cabeza de Baca and Ellis2017; Del Giudice et al., Reference Del Giudice, Ellis and Shirtcliff2011). Therefore, children who are raised in under conditions that are considered high in extrinsic morbidity–mortality and with high levels of unpredictability – such as IPV – may develop EC strategies that favor short-term over long-term gains. In these environments, the use of “slow” life history strategies (i.e., those that employ high levels of EC) may undermine evolutionary fitness because youth mature into environments with relatively shorter life expectancy and less predictable access to resources (B. J. Ellis et al., Reference Ellis, Figueredo, Brumbach and Schlomer2009). Instead, adaptive development in the context of IPV exposure often includes strategies that would be characterized as low EC because such approaches (e.g., a present orientation as opposed to a future orientation) are hypothesized to promote reproduction before longer-term investments in parenting and health-promoting behaviors, which are more consistent with lower extrinsic morbidity-mortality and less predictable environments. Low EC, adaptive in the context of IPV exposure, may be viewed as maladaptive across time and/or when environmental circumstances change.
The literature on EC in children and adolescents experiencing adversity provides general support for the theory that adaptation in harsh and unpredictable circumstances involves low EC strategies. Harshness both within the home and in the community is associated with lower levels of EC by age 3 (Warren & Barnett, Reference Warren and Barnett2020). Higher levels of early childhood unpredictability are linked prospectively to low measured future orientation in adolescence and young adulthood (Hartman et al., Reference Hartman, Sung, Simpson, Schlomer and Belsky2018). Atherton et al. (Reference Atherton, Lawson and Robins2020) found that during late childhood and across adolescence, the developmental trajectory of EC is generally u-shaped (i.e., EC decreases between ages 10 and 14, then increases into late adolescence/early adulthood). Importantly, this trajectory was moderated by experiences of adversity, including violence exposure and discrimination, which exacerbated the decrease in EC during late childhood/early adolescence (Atherton et al., Reference Atherton, Lawson and Robins2020). However, because prior work in the field has examined the combined effects of various forms of harshness and unpredictability (e.g., parent–child aggression, IPV exposure, community violence) on children’s and adolescents’ EC development, further investigation of particular specific influence of IPV is needed. Intervention and advocacy for families affected by IPV can be enhanced by knowledge on IPV’s particular effects on youths’ development, especially during late childhood and early adolescence, when less is known about the specific ways that IPV may influence EC.
Caregiver depression
One likely factor that may influence children’s and adolescents’ EC in the context of IPV, and one that can be targeted by intervention, is the mental health of their caregivers, especially their levels of depression. Caregivers’ depressive symptoms, specifically, are robustly associated with experiences of IPV (Bacchus et al., Reference Bacchus, Ranganathan, Watts and Devries2018) as well as children’s and adolescents’ EC abilities (Bates et al., Reference Bates, Salsberry, Justice, Dynia, Logan, Gugiu and Purtell2020; Goodman & Gotlib, Reference Goodman and Gotlib1999). Mounting evidence suggests that links between caregiver depressive symptoms and children’s and adolescents’ EC may be transactional (i.e., parental depression is linked to lower EC in youth, which in turn exacerbates parental depression) (Choe et al., Reference Choe, Olson and Sameroff2014).
Children and adolescents with low EC may require more support from their caregivers to effectively regulate their emotions (Morris et al., Reference Morris, Criss, Silk and Houltberg2017), and depressive symptoms interfere with caregivers’ ability to meet their children’s regulatory needs (Goodman et al., Reference Goodman, Simon, Shamblaw and Kim2020; Lovejoy et al., Reference Lovejoy, Graczyk, O’Hare and Neuman2000). When their emotions are unregulated, youth with low EC may then respond in ways that further exacerbate caregivers’ depressive symptoms, leading to greater disengagement from the child and higher levels of negative emotionality in the parent (Choe et al., Reference Choe, Olson and Sameroff2014). As these transactional relations between CD and EC unfold over time, cascading effects can influence other developmental processes, especially in the context of IPV (Clark et al., Reference Clark, Grogan-Kaylor, Galano, Stein and Graham-Bermann2022). Importantly, prior work with families experiencing IPV has demonstrated that CD is one of the caregiver-level factors most strongly linked to parenting behaviors, and to child and adolescent outcomes (i.e., above and beyond other forms of caregiver psychopathology) (Galano et al., Reference Galano, Stein, Clark, Grogan-Kaylor and Graham-Bermann2022; Grogan-Kaylor et al., Reference Grogan-Kaylor, Stein, Galano and Graham-Bermann2019; Stein et al., Reference Stein, Prakken, Grogan-Kaylor, Galano, Clark and Graham-Bermann2022).
CD has a marked influence on key developmental processes across childhood and adolescence, and that the impact of CD on these processes is moderated by contextual factors including violence exposure (Burkhouse & Kujawa, Reference Burkhouse and Kujawa2022; Suor et al., Reference Suor, Granros, Calentino, Luan Phan and Burkhouse2021). Furthermore, adaptive intimate partner relationships have been found to buffer the influence of mothers’ depressive symptoms on their young children’s EC (Goldstein et al., Reference Goldstein, Borelli and Shai2022). Indeed, a confluence of research across multiple levels of analysis suggests that the factors that influence EC development depend on the context in which the child or adolescent is developing, where factors associated with low EC become more salient in higher-risk contexts (e.g., contexts with greater levels of family conflict, cumulative risk, violence exposure) (S. Kim & Kochanska, Reference Kim and Kochanska2021; Rioux et al., Reference Rioux, Castellanos-Ryan, Parent and Séguin2016; Sun et al., Reference Sun, Measelle and Ablow2021; Waxman et al., Reference Waxman, Lieshout and Schmidt2014). This may be especially true when contextual factors contribute to the deployment of “fast” life history strategies, including low measured EC, which may be adaptive in response to one salient developmental threat (e.g., IPV) and then exacerbate – and be exacerbated by – others (e.g., CD). This process is consistent with what life history theories would predict, because although cascading transactions between low EC and high CD in the context of IPV may appear maladaptive at the level of the individual (e.g., by contributing to higher levels of stress, more difficulties with daily living), low EC would still be adaptive in terms of evolutionary fitness, as the unpredictability and morbidity-mortality factors within this environment would prompt the prioritization of reproduction over investment in longer-term health-promoting and parenting behaviors.
Developmentally, studying potential transactional influences between CD and EC across the transition from childhood into adolescence may be particularly important. Because self-regulation is especially consequential during late childhood into early adolescence (Hollenstein & Lougheed, Reference Hollenstein and Lougheed2013; Sawyer et al., Reference Sawyer, Afifi, Bearinger, Blakemore, Dick, Ezeh and Patton2012), an exploration of the factors that influence EC development during this period of transition merits attention. Furthermore, adolescence is a time when sensitivity to social context becomes distinctly apparent (Guyer, Reference Guyer2020; Schriber & Guyer, Reference Schriber and Guyer2016), suggesting that adolescents’ EC development may be especially sensitive to social–environmental conditions (including CD).
The present study
This study was designed to evaluate the hypothesized moderating influence of IPV exposure on the associations between caregiver depressive symptoms (CD) and EC in children and adolescents, as well as potential transactional relationships among these factors during middle childhood/early adolescence. In a sample of children and adolescents ages 7–17 assessed longitudinally across 3 years, this study leveraged multigroup latent change score (LCS) modeling (McArdle & Hamagami, Reference McArdle, Hamagami, Collins and Sayer2001) to examine: (1) baseline covariance between CD and EC; (2) whether changes in EC were associated with baseline levels of CD, and vice versa; (3) whether changes in CD and EC were associated with one another; and (4) whether and how these processes differed between children and adolescents who had witnessed IPV and those who had not (IPV+ and IPV− participants, respectively). LCS modeling was chosen to evaluate not only average change in EC and CD over time in our sample, but also to examine whether there were differences in change score variance (i.e., individual differences around slopes and intercepts) based on IPV exposure status, as well as proportional change (i.e., whether and how prior levels of EC/CD influenced EC/CD change over time). We hypothesized that CD and EC would have significant, negative associations both cross-sectionally and across time, and that these associations would be stronger for IPV+ relative to IPV− participants.
Method
Participants
Participants (N = 365) were children and adolescents (44.1% boys, 55.6% girls, 0.3% did not report gender identity) in the 3rd, 6th, and 9th grades recruited from schools in Denver, Colorado and surrounding communities as a part of the Gene–Environment Mood (GEM) Study (Hankin et al., Reference Hankin, Young, Abela, Smolen, Jenness, Gulley, Technow, Gottlieb, Cohen and Oppenheimer2015). Eligibility criteria included English language fluency and absence of intellectual disability, autism spectrum disorder, and psychotic disorder. Participants ranged in age from 7 to 17 at baseline (M = 12.04, SD = 2.32); children in the 3rd grade cohort ranged in age from 7.25 to 10.50 (M = 9.20, SD = 0.48), the age range for the 6th grade cohort was 10.92–13.92 (M = 12.10, SD = 0.53), and the 9th grade cohort ranged in age from 13.58 to 16.67 (M = 14.91, SD = 0.51). At Time 2, children and adolescents’ average age was 13.62 (SD = 2.29); the youngest child in the sample was 9.51 years old and the oldest adolescent was 17.53 years old. At Time 3, participants’ ages ranged from 10.69 to 19.12 (M = 15.08, SD = 2.31). Median household income was US$75,000 (M = US$90,991.11, SD = US$89,527.98), and the majority (86.8%) of participants’ caregivers reported at least some college education. At baseline, 72.5% of children and adolescents identified as white, 7.7% reported a multiracial identity, 6.6% identified as African American or Black, 3.6% identified as Asian/Pacific Islander, 1.4% identified as American Indian/Alaska Native, and 8.2% endorsed “Other” as their racial identity. Approximately 16.8% identified as Hispanic/Latino. Demographic characteristics of the children and adolescents in the sample are summarized in Table 1.
Table 1. Sample demographics, study variable means (standard deviations), and correlations

Note. *p < .05, **p < .01, ***p < .001. IPV = intimate partner violence. IPV+ = participants exposed to IPV. IPV− = participants with no history of IPV exposure. API = Asian/Pacific Islander. AI/AN = American Indian/Alaska Native. CD = caregiver depression. EC = effortful control. All pairwise comparisons of EC and CD between IPV+ and IPV− groups were significant, ps < .001.
All caregivers who participated in the study identified as women, and most (96.1%) were the biological or adoptive mother of the child/adolescent participant. The remaining 3.9% of caregivers were the child/adolescent’s aunt or grandmother. At baseline, 64.5% of caregivers identified as white, 1% reported a multi-racial identity, 16.5% identified as African American or Black, 15.5% identified as Asian/Pacific Islander, 0.3% identified as American Indian/Alaska Native, and 2.2% endorsed “Other” as their racial identity. Approximately 8.9% identified as Hispanic/Latino. Eighty percent of caregivers were married (or cohabiting in a marriage-like relationship), 5.1% were single, 10.1% were divorced, 2.5% were separated, and 2.2% were widowed. Caregivers ranged in age from 29 to 63 years (M = 43.38, SD = 5.94).
Procedure
Upon receiving informed consent from caregivers and assent from children and adolescents, participants completed three assessments over 3 years: one at baseline (Time 1), another 18 months later (Time 2), and a third 36 months after baseline (Time 3). Participants and caregivers received monetary compensation for participating in the study. All materials and procedures were approved by the University Institutional Review Board.
Measures
Intimate partner violence (IPV) exposure
Children and adolescents’ exposure to IPV was assessed using their responses to the Youth Life Stress Interview (YLSI) (Rudolph & Flynn, Reference Rudolph and Flynn2007). The YLSI is a semi-structured interview that includes questions about chronic and episodic stressors in several life domains, and has advantages over self-report measures of IPV because it ensures that IPV is clearly defined for participants and provides opportunities for youth to report violence in caregiver relationships that may be missed using alternative methods (Follingstad & Bush, Reference Follingstad and Bush2014; Lam et al., Reference Lam, Fals-Stewart and Kelley2009). In this study, trained interviewers asked participants increasingly specific questions about children’s and adolescents’ life experiences across family, school, and community contexts. IPV exposure was determined based on responses to the family stress and violence exposure modules of the YLSI. Within the family stress module, participants described their family structure and relationships, and specific questions were asked about relationships between parents/parent-figures and their intimate partners (e.g., “How often do they fight? What are their fights like?”). The violence exposure module asked participants about their experiences with physical as well as psychological violence (e.g., “Have you seen someone get hurt or threatened?”). Participants also specifically reported any lifetime exposure to “serious marital conflict.” Responses to the YLSI were reviewed by an independent team and coded 1 for any lifetime exposure to either chronic or episodic IPV and 0 where no IPV exposure was indicated. Final IPV scores were determined based on consensus agreement. Example responses consistent with IPV exposure included witnessing or overhearing physical violence, witnessing or overhearing verbal abuse with fears for family members’ safety, as well as coercive or spiteful actions meant to exert power or control in the intimate relationship (e.g., “father ran off with kids and didn’t tell mom”). Children and adolescents who endorsed having ever witnessed IPV in the home comprised the IPV+ group (45.3%), and all other participants were in the IPV− group (54.7%). The proportion of participants in the IPV+ group in this study is slightly greater than the 30–40% estimates of youth IPV exposure prior to age 17 (Finkelhor et al., Reference Finkelhor, Turner, Shattuck and Hamby2013; Hamby et al., Reference Hamby, Finkelhor, Turner and Ormrod2011), which was expected because the semi-structured interviewing method likely captured forms of IPV that may have been missed on questionnaire measures. Indeed, prior work has supported the reliability and validity of the YLSI to evaluate chronic and acute life stressors across childhood and adolescence (Rudolph & Flynn, Reference Rudolph and Flynn2007; Rudolph, Reference Rudolph2008).
Caregiver depressive symptoms (CD)
Caregivers’ responses to the Beck Depression Inventory-II (BDI) (Beck et al., Reference Beck, Steer and Brown1996) were used to measure CD. The BDI includes 21 items, each assessing a symptom of depression on a 4-point scale ranging from 0 to 3, with higher ratings indicating greater depression symptom severity. The BDI is a well-established measure of depression in clinical and community samples of adults, with strong reliability and validity (Wang & Gorenstein, Reference Wang and Gorenstein2013). Internal consistency of the BDI in the present study was strong across time points (Cronbach’s α = 0.90 Time 1, 0.93 Time 2, 0.93 Time 3).
Effortful control (EC)
Participants’ EC was measured using responses to the 16 EC items (Activation Control, Attention, and Inhibitory Control subscales) of the Early Adolescent Temperament Questionnaire-Revised (EATQ-R) (L. K. Ellis & Rothbart, Reference Ellis and Rothbart2001). EATQ-R items are rated on a scale from 1 (almost always untrue) to 5 (almost always true), where higher scores indicate higher levels of EC. Example items include: “If I have a hard assignment to do, I get started right away” (Activation Control), “It is easy for me to really concentrate on homework problems” (Attention), and, “When someone tells me to stop doing something, it is easy for me to stop” (Inhibitory Control). The Effortful Control superfactor of the EATQ-R is supported by factor analytic studies (Snyder et al., Reference Snyder, Gulley, Bijttebier, Hartman, Oldehinkel, Mezulis, Young and Hankin2015), and the psychometric properties of the instrument are strong across childhood and adolescence (Muris & Meesters, Reference Muris and Meesters2009). The internal consistency of the EC items on the EATQ-R in the present study was: Cronbach’s α = 0.77 Time 1, 0.83 Time 2, 0.83 Time 3.
Covariates
To address the confounding effects of developmental age and non-IPV traumatic experiences on the processes under investigation in this study, both variables were included as covariates in the LCS model.
Non-IPV trauma experiences
Because IPV often co-occurs with other significant life stressors that may alter EC development and/or influence caregivers’ depressive symptoms (Chan et al., Reference Chan, Chen and Chen2021), participants’ experiences of other forms of trauma were evaluated using the Posttraumatic Stress Disorder (PTSD) module of the Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions (ADIS-IV; Silverman & Albano, Reference Silverman and Albano1996). Both parents and children/adolescents completed the ADIS-IV, which comprehensively evaluates anxiety disorder symptoms consistent with diagnoses in the 4th Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association (APA), 1994). The PTSD module probes for experiences of trauma meeting DSM-IV Criterion A for PTSD (i.e., witnessing or experiencing actual or threatened death or serious injury). Participants’ responses to Criterion A PTSD probes were coded for experiences of significant trauma, such that participants who reported experiences of trauma received a score of 1, unless the only reported event was IPV, in which case they received a score of 0. Participants who reported no trauma also received scores of 0 (i.e., significant trauma other than IPV = 1, no reported trauma or only reported event was IPV = 0). Example responses denoting significant trauma included a sibling’s suicide attempt, having been sexually assaulted by a peer, and having witnessed a shooting. Overall, 40 participants (11.0%) scored 1 on this measure, and 325 (89.0%) scored 0. Among participants who scored 0, 160 (49.2%) had not experienced IPV and 165 (50.8%) had. Of the participants who scored 1, 17.5% also endorsed experiences of IPV.
Analytic strategy
A multigroup LCS model (Klopack & Wickrama, Reference Klopack and Wickrama2020; McArdle & Hamagami, Reference McArdle, Hamagami, Collins and Sayer2001) was specified that included the following latent parameters for both CD and EC: a latent intercept, a latent linear slope factor, and a latent proportional change factor (i.e., change since the previous measurement occasion beyond that accounted for by the latent slope factor). Latent factors for CD were estimated using caregivers’ responses to the BDI, and latent factors for EC were estimated using participants’ responses to the EC items of the EATQ-R.
To evaluate baseline covariance between CD and EC, paths were parameterized between latent intercept scores on both variables. Paths between latent intercepts and latent slopes on each factor indicated whether change on one factor was influenced by baseline levels of the other. Paths between latent slope factors for EC and CD revealed whether and how changes in CD influenced changes in EC (and vice versa; see Figure 1). Moderation by IPV exposure was examined using Chi-square tests comparing a constrained model (where parameters were set to be equal between groups) to the freely estimated multigroup model, with a statistically significant result indicating that relationships between CD and EC differed between IPV+ and IPV− participants.
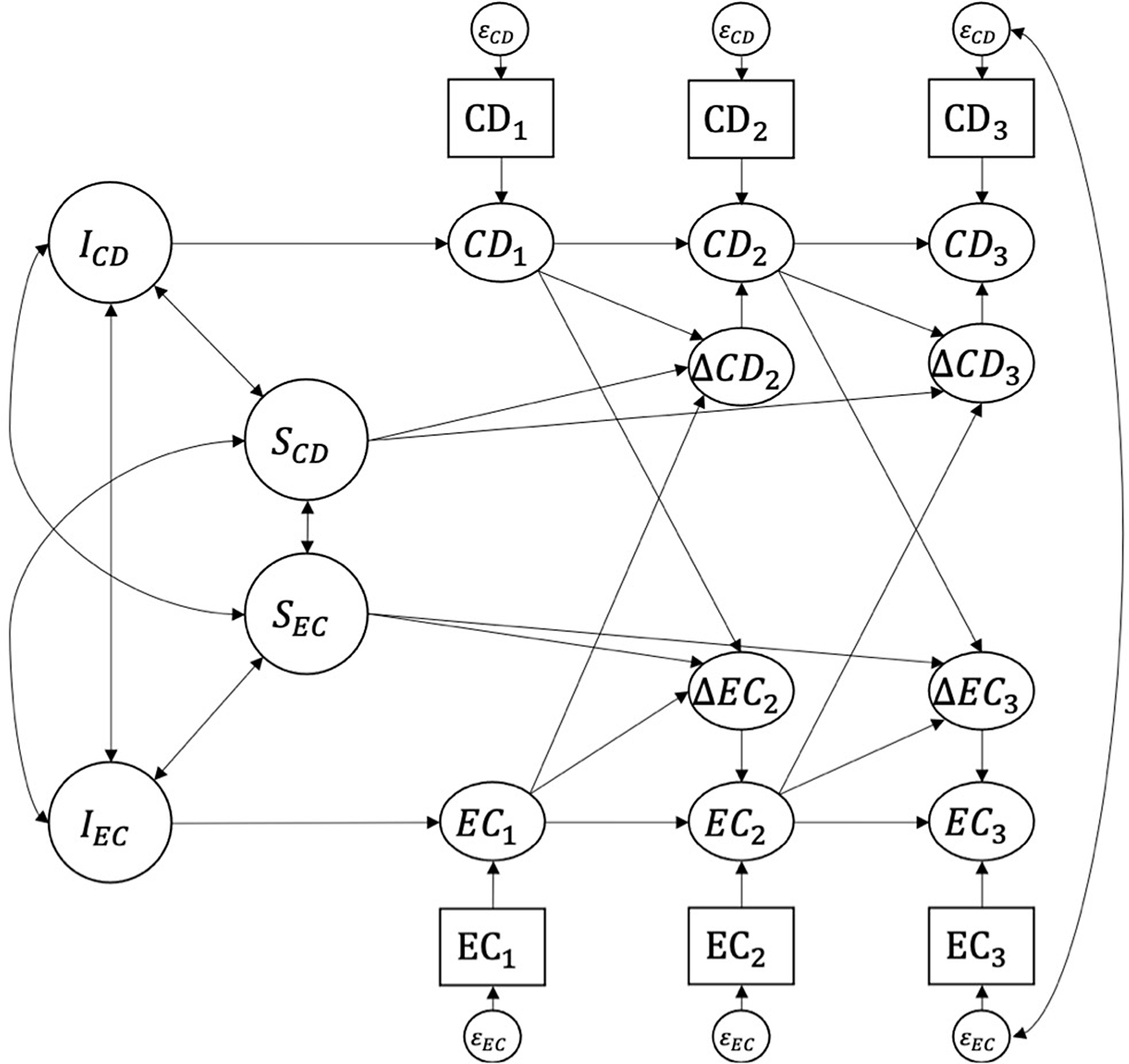
Figure 1. Latent change score (LCS) model of associations between caregiver depressive symptoms (CD) and youth effortful control (EC) across three measurement occasions. I = intercept. S = slope.
As articulated by Kievit et al. (Reference Kievit, Brandmaier, Ziegler, van Harmelen, de Mooij, Moutoussis, Goodyer, Bullmore, Jones, Fonagy, Lindenberger and Dolan2018), LCS models offer several advantages to examining developmental change over time relative to, for example, latent growth curve models. In addition to providing information on average rates of change over time (i.e., latent slope factors and LCSs between time points), LCS models estimate change score variance, which in our model captures the extent to which the rates of change in CD and EC differ between participants. Furthermore, autoregressive parameters estimate proportional change, or the extent to which change is dependent on scores at the previous time point – for example, in our model, the extent to which change in participants’ EC scores between Time 1 and Time 2 depends on their Time 1 EC. Multigroup LCS models provide all of the benefits of LCS models while also testing for differences in parameter estimates between groups; here, we tested whether IPV exposure moderated the relationships between caregiver depression and EC across 3 years.
To determine the unique moderating effects of IPV on relations between CD and EC over time, participants’ non-IPV traumatic experiences were included as covariates in the multigroup LCS model. Participants’ age was also included as a covariate to account for developmental differences in EC abilities.
Finally, we tested a model that included a cohabitation status covariate, which indicated whether caregivers’ intimate partners resided in the participant’s home (1 = yes, 0 = no). This analysis was run to explore whether the chronicity of participants’ IPV exposure may have influenced relations among CD and EC in this sample, as children and adolescents cohabitating with caregivers’ partners were likely exposed to more frequent IPV than participants whose caregivers had partners residing elsewhere.
Missing data
Over three quarters of participants (76.4%; n = 279) were retained across the 3 years of the study, and 81.6% (n = 298) were retained through Time 2. Data were complete on all variables of interest for all participants who were retained at each time point, with the exception of four missing CD scores at Time 2 (1.3% missing) and five missing EC scores at Time 3 (1.8% missing). Examination of missing data patterns and an omnibus test supported the missing at random (MAR) assumption (Little’s MCAR test X 2 (48, N = 365) = 62.37, p = .080).
Multigroup LCS model analyses were conducted using Mplus Version 8 (Muthén & Muthén, Reference Muthén and Muthén2017) with full information maximum likelihood estimation to account for missing data. Goodness of fit was evaluated according to Hu and Bentler’s (Reference Hu and Bentler1999) criteria (i.e., TLI and CFI above .95; SRMR lower than .08; RMSEA below .06) across multiple indices. Rather than relying on any single measure of model fit, convergence across fit indices was prioritized (Barrett, Reference Barrett2007).
Results
Summary data
Means, standard deviations, and correlations among study variables across time points are reported in Table 1. There was notable variability in individual trajectories of CD and EC (see Tables 1 and 2). Mean-level trends showed that participants who had been exposed to IPV had lower EC scores than participants in the IPV− group, and caregivers in the IPV+ group also indicated higher levels of depression relative to IPV− caregivers. Overall average levels of CD in both groups were low (IPV+ M = 6.16, SD = 6.36; IPV− M = 4.33; SD = 5.13); however, CD scores were as high as 50, indicating severe levels of depression in some families.
Table 2. Multigroup latent change score model results
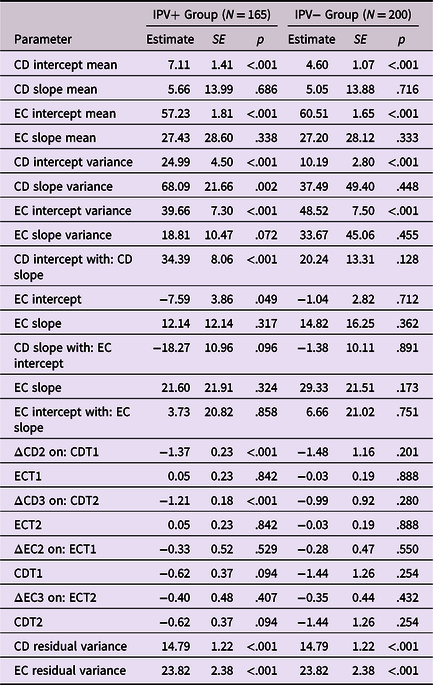
Note. IPV = intimate partner violence. IPV+ = participants exposed to IPV. IPV− = participants with no history of IPV exposure. CD = caregiver depression symptoms. EC = effortful control. Participants’ age and non-IPV trauma experiences were included as covariates in the latent change score model.
Moderation by IPV
Growth models were specified to compare change processes in EC and CD over time between IPV+ and IPV− groups, accounting for non-IPV traumatic experiences and participant age. A multigroup LCS model that included a proportional change factor provided a better fit for the data than a model that included only a constant change factor, Δχ 2 (4) = 17.91, p = .001.Footnote 1 This significantly improved model fit supports the use of LCS modeling as the analytic approach. Additionally, comparison of model fit between LCS models with freely estimated versus constrained parameters shows that IPV exposure significantly moderated relationships between CD and EC over time: Δχ 2 (14) = 27.18, p = .018.Footnote 2
As shown in Table 2, model-estimated baseline levels of CD were lower in the IPV− group relative to the IPV+ group, and caregivers in the IPV+ group reported greater increases in depression over the 3 years of the study than IPV− caregivers. In contrast, model-estimated baseline EC was lower in the IPV+ than the IPV− group. Rates of change in EC were similar across groups. Significant individual differences in the intercept for both EC and CD factors were found in both groups, whereas the random effects for CD slope were only significant for the IPV+ group. The variance of the EC slope factor was not significant in either the IPV+ or the IPV− group.
Associations between EC and CD also differed between groups. Specifically, EC and CD were linked for children and adolescents who had been exposed to IPV, although there were no significant associations between changes in EC and CD in the IPV− group. In the IPV+ group, children and adolescents with higher levels of EC at baseline had caregivers who reported lower concurrent levels of depression. Higher baseline levels of CD were associated with greater increases in CD over time. Proportional change in CD between time points was also significant, indicating an attenuation of the rate of change in CD symptoms between assessments for caregivers in the IPV+ group (i.e., although the general rate of change in CD across time was higher for the IPV+ group relative to the IPV− group, the growth in CD slowed between measurement occasions). Full model results are provided in Table 2 and Figure 2.
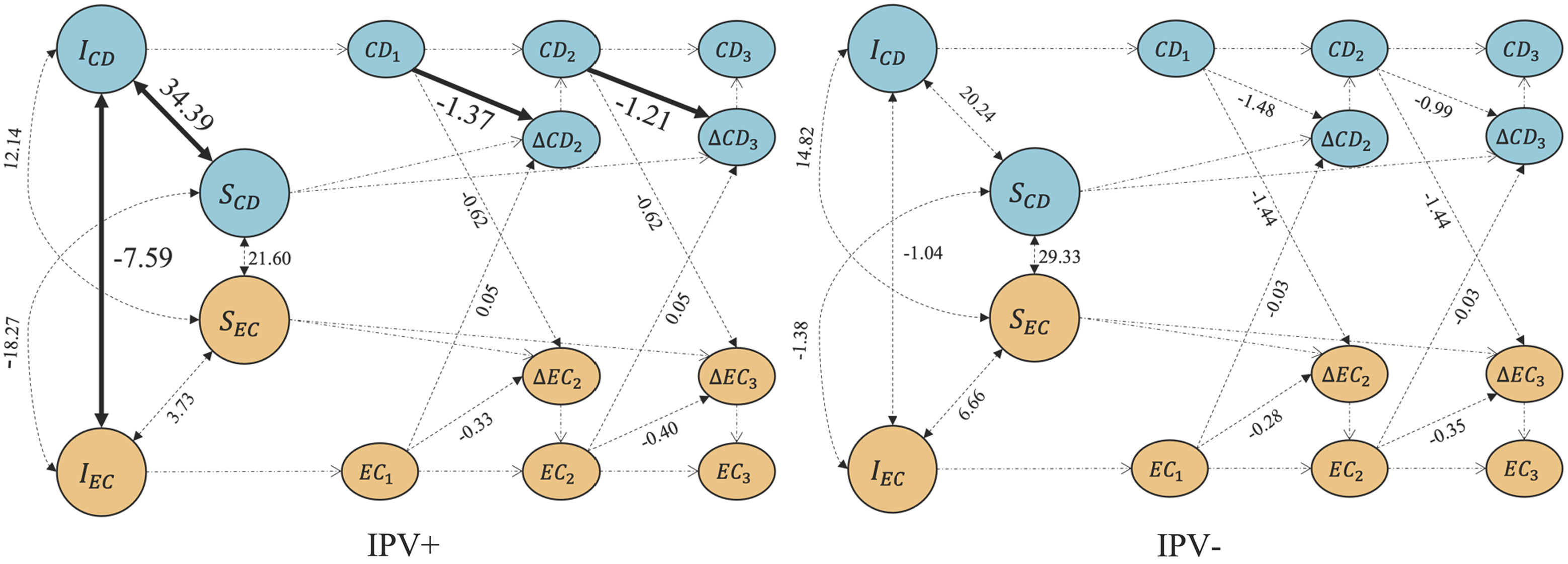
Figure 2. Unstandardized parameter estimates for latent change score models comparing associations between caregiver depressive symptoms (CD) and effortful control (EC) across three measurement occasions for participants exposed (IPV+) and not exposed (IPV−) to intimate partner violence. I = intercept. S = slope.
To test the sensitivity of the multigroup LCS model, we also tested a model that included an additional covariate denoting whether caregivers’ intimate partners resided in the participants’ home (i.e., cohabitation status; 1 = yes, 0 = no). The LCS model including the cohabitation status covariate revealed largely the same pattern of results as those reported above, with one notable exception. Whereas baseline CD and EC were significantly associated for IPV+ participants in the primary model (without the cohabitation status covariate), when cohabitation status was included, this association was no longer significant. This difference in findings may indicate that the chronicity of IPV exposure affects the links between CD and EC, as children and adolescents who live in the same home as the partner of their caregiver are likely exposed to more frequent IPV than those living homes where the partner of their caregiver lives elsewhere. Full model results including all covariates are reported in Supplemental Table 1.
Discussion
Until recently, examination of children’s and adolescents’ adjustment following exposure to IPV has largely been limited either to factors within the individual (e.g., stress response systems, fear learning) or within the environment (e.g., parenting, caregiver mental health). Little attention has been given to interactions between individual-level self-regulation processes and family-level influences that may have transdiagnostic implications for IPV-exposed children and adolescents, despite strong evidence for such links in other developmental contexts (see, for example, Bronfenbrenner & Evans, Reference Bronfenbrenner and Evans2000; Cicchetti & Rogosch, Reference Cicchetti and Rogosch2002). The purpose of this study was to compare trajectories of children’s and adolescents’ EC and caregivers’ depressive symptoms (CD) between families reporting a history of IPV (IPV+) and those with no reported IPV history (IPV−) during a key developmental transition in middle childhood and early adolescence. Bioecological systems theory (Bronfenbrenner & Morris, Reference Bronfenbrenner, Morris, Damon and Lerner1998) posits that transactions between individual-level factors and family-level environments, situated within larger community and sociohistorical contexts, are critical to shaping development across time. Findings support this perspective and show that relationships between CD and EC in children and adolescents depend on exposure to IPV. As we discuss in more detail next, these results highlight targetable avenues for intervention to support EC development in children and adolescents, which may have downstream benefits to improve well-being and mental health given the role of EC as a transdiagnostic process associated with risk for psychopathology (Lynch et al., Reference Lynch, Sunderland, Newton and Chapman2021).
Specifically, caregivers in the IPV+ group reported higher levels of depression as well as greater overall increases in depressive symptoms across the 3-year follow-up with repeated measures, relative to the IPV− group. Further, it was only among the IPV+ group that higher levels of CD were significantly associated with lower EC among children and adolescents. Taken together, along with significantly lower levels of EC in IPV+ relative to IPV− participants over time, these results suggest that among children experiencing IPV, caregiver depressive symptoms may have promoted the use of “fast” life history strategies (i.e., low EC; present as opposed to future orientation) that were maintained over the 3-year follow-up across the transition into adolescence. As the rates of change in EC over time were similar between IPV+ and IPV− participants, consistent with prior work showing relatively high stability of individual differences in EC but that violence exposure may moderate EC trajectories (Atherton et al., Reference Atherton, Lawson and Robins2020; Tiberio et al., Reference Tiberio, Capaldi, Kerr, Bertrand, Pears and Owen2016), the longitudinal findings from this study reveal that children and adolescents with lower EC from the IPV+ group did not “catch up” to the higher EC levels of their IPV− peers.
There are several potential reasons why higher levels of CD were associated with lower EC only among participants who experienced IPV. First, CD likely affects the use and implementation of adaptive and effective parenting practices in the context of IPV. Among families with IPV exposure, maternal depressive symptoms are associated with increased use of parenting behaviors that are consistent with lower levels of EC in children and adolescents (Grogan-Kaylor et al., Reference Grogan-Kaylor, Galano, Stein, Clark and Graham-Bermann2020; Stein et al., Reference Stein, Hunter, Graham-Bermann, Galano, Clark and Grogan-Kaylor2020; Valiente et al., Reference Valiente, Lemery-Chalfant and Reiser2007; Warren & Barnett, Reference Warren and Barnett2020). Specifically, among IPV-exposed parents, those with higher reported levels of depression are more likely to endorse the use of corporal punishment (e.g., spanking, slapping, or hitting with objects) to discipline their children (Grogan-Kaylor et al., Reference Grogan-Kaylor, Galano, Stein, Clark and Graham-Bermann2020), and are also less accepting of their children’s negative emotions (Stein et al., Reference Stein, Hunter, Graham-Bermann, Galano, Clark and Grogan-Kaylor2020). Parental harshness, including the use of corporal punishment practices and lower acceptance of children’s negative emotions, are strongly linked to lower levels of EC in children and adolescents (Valiente et al., Reference Valiente, Lemery-Chalfant and Reiser2007; Warren & Barnett, Reference Warren and Barnett2020). Although CD is known to affect parenting regardless of context (Goodman et al., Reference Goodman, Simon, Shamblaw and Kim2020), our findings are consistent with prior research suggesting that these effects can be exacerbated or attenuated by the quality of the family environment (Goldstein et al., Reference Goldstein, Borelli and Shai2022; S. Kim & Kochanska, Reference Kim and Kochanska2021; Suor et al., Reference Suor, Granros, Calentino, Luan Phan and Burkhouse2021; Waxman et al., Reference Waxman, Lieshout and Schmidt2014). Taken together, parenting factors may account for the associations between CD and children’s and adolescents’ EC among IPV+ families in this study.
Second, children’s emotional processing may also partly explain associations between CD and EC among offspring exposed to IPV. Children exposed to adversity have greater difficulty disengaging from negative emotional content, and these attentional biases mediate associations between childhood adversity and alterations in self-regulation (McLaughlin & Lambert, Reference McLaughlin and Lambert2017). Children and adolescents with histories of violence exposure are faster to notice and take longer to look away from angry, sad, and threatening faces (Mastorakos & Scott, Reference Mastorakos and Scott2019; Shackman & Pollak, Reference Shackman and Pollak2014), which is associated with lower parent-reported emotion regulation skills (Bender et al., Reference Bender, McKinney, Schmidt-Sane, Cage, Holmes, Berg, Salley, Bodell, Miller and Voith2022; Miller-Graff & Scheid, Reference Miller-Graff and Scheid2021). This line of work suggests that children and adolescents who experience IPV have heightened sensitivity to CD, likely because careful attunement to caregivers’ functioning is associated with greater evolutionary fitness, especially in harsh and unpredictable circumstances (Cabeza de Baca & Ellis, Reference Cabeza de Baca and Ellis2017). While potentially adaptive in the short-term in the context of IPV, children who adjust to caregivers’ heightened depression in the form of lower EC may have longer-term challenges – particularly as their EC abilities do not appear to “recover” over time, as evidenced by findings from the present study.
Strengths, limitations, and future directions
Innovative in its scope and approach, this study has several strengths. In particular, the use of LCS as a sophisticated data analytic technique is highly appropriate to rigorously examine this study’s key questions, including those previously unanswered about differences in EC and CD trajectories between IPV+ and IPV− families. The use of LCS modeling allowed for examination of the variance of growth factors associated with CD and EC between groups. Importantly, for example, LCS revealed individual differences in slope factors for EC and CD only for the IPV+ group. Such significant variance among those exposed to IPV may indicate differential susceptibility in the multiple influences that can contribute to EC development and caregivers’ depression over time. Use of LCS as an advanced, appropriate data analytic approach permitted discovery of such significant variance in slopes for EC and CD trajectories only among the IPV+ group, and this novel finding opens new avenues for future research to explain the substantial individual differences in transdiagnostic risk processes, such as EC.
Furthermore, this study employed a multi-informant, multimethod design in which caregivers reported their own depressive symptoms, EC was measured via self-report, IPV exposure status was determined based on a semi-structured interview, and non-IPV trauma experiences were evaluated using reports from multiple informants on participants’ exposure to traumatic events. Analyses that rely on a single method and/or informant typically result in effect sizes that are inflated by shared aspects of measurement (Owens et al., Reference Owens, Potter, Hyatt, Albaugh, Thompson, Jernigan, Yuan, Hahn, Allgaier and Garavan2021). By reducing sources of shared variance between measured constructs, our findings may capture a more accurate representation of the relations among IPV exposure, EC, and CD.
At the same time, study limitations offer opportunities for future research to build and improve upon the current work. First, the sample’s demographic and geographic diversity may limit generalizability of findings to communities with differences in access to resources. Availability of accessible healthcare, education, and mental health resources varies widely across communities in the United States, all of which contribute to disparities in IPV, EC, and depression (Clark et al., Reference Clark, Galano, Grogan-Kaylor, Montalvo-Liendo and Graham-Bermann2016; M. Kim, Reference Kim2014; Sturge-Apple et al., Reference Sturge-Apple, Davies, Cicchetti, Hentges and Coe2017). Future work can evaluate the strength and robustness of these relationships across diverse samples. Second, although these results lend credence to evolutionary theories of EC development, the present study did not provide direct evidence that IPV+ participants’ use of “fast” life history strategies was more adaptive, as evolutionary theories would suggest. Further research is needed to establish whether and how the use of “fast” life history strategies in the context of IPV may be advantageous to developing youth in these environments. Such work could explore associations between youths’ measured EC and behaviors more closely linked to evolutionary fitness (e.g., risk-taking, sexual activity), and compare these processes between IPV+ and IPV− families.
Prior work examining trajectories of EC development across childhood and adolescence has revealed a u-shaped pattern, suggesting decreases in EC in late childhood/early adolescence and increases in later adolescence/early adulthood (Atherton et al., Reference Atherton, Lawson and Robins2020). Taken with findings from the present study, it is possible that the effects of IPV exposure on co-occurring EC and CD trajectories may be moderated by youths’ age. Further research in this area should account for developmental differences is EC strategies when examining the relations among caregivers’ depressive symptoms, EC, and youths’ IPV exposure. Such work would do well to include larger sample sizes with more measurement occasions to increase statistical power. The novelty of LCS as an analytic approach means that empirical guidelines for its statistical power have not yet been developed (Kievit et al., Reference Kievit, Brandmaier, Ziegler, van Harmelen, de Mooij, Moutoussis, Goodyer, Bullmore, Jones, Fonagy, Lindenberger and Dolan2018). Klopack and Wickrama (Reference Klopack and Wickrama2020) caution that statistical power may be increasingly limited as LCS models become more complex, noting that, aside from larger sample sizes (i.e., N > 200) and more (i.e., > 2) time points, information on elements of study design that affect statistical power using LCS modeling is limited. Indeed, it is possible that the lack of longitudinal associations between CD and EC in this study may have been attributable, in part, to insufficient statistical power to detect such associations in this sample.
Despite this possible limitation, findings from the present study lend support to the notion that relations among CD and EC are moderated by IPV experiences, and that concurrent CD and EC are more strongly related in the context of IPV exposure. However, there are several potential ways to interpret the null result for longitudinal associations between CD and EC. It is possible that limitations in study design constrained our ability to detect true associations between CD and EC over time. Alternatively, it may be that there was insufficient variation in caregivers’ levels of depression to capture meaningful associations between EC and CD over time. Although CD scores ranged from minimal to severe levels of depression across time points, most CD scores fell within the minimal range. Finally, it is possible that CD, rather than causing longitudinal change in EC, is better considered as a contextual factor that may have implications for youths’ EC depending on other influences (e.g., parenting behaviors, availability of other social support, etc.). Future, well-powered research in this area could compare models treating CD as a causal or contextual factor to better elucidate the processes associated with youths’ EC development.
Finally, the measurement of IPV as present or absent did not allow for the determination of whether and how the degree of IPV experiences may influence the processes under investigation. It is possible that different forms of IPV contribute to CD and EC in unique ways, as prior work has indicated that psychological, as opposed to physical or sexual violence, has stronger associations with revictimization and chronicity of violence experiences (Stein et al., Reference Stein, Grogan-Kaylor, Galano, Clark and Graham-Bermann2019). Future work using continuous measures of IPV – and that distinguishes between IPV subtypes – may further elucidate pathways through which IPV experiences alter caregiver and youth functioning. Findings from the present study could inform intervention science examining outcomes associated with families’ participation in interventions for IPV-exposed families, as some research has indicated that interventions tailored to families who recently experienced IPV can reduce the incidence of IPV itself (Clark et al., Reference Clark, Grogan-Kaylor, Galano, Stein, Montalvo-Liendo and Graham-Bermann2018; McCabe et al., Reference McCabe, Gonzalez-Guarda, Peragallo and Mitrani2016; Miller et al., Reference Miller, Howell and Graham-Bermann2014), can decrease symptoms of depression in caregivers (Arroyo et al., Reference Arroyo, Lundahl, Butters, Vanderloo and Wood2017; Stein et al., Reference Stein, Grogan-Kaylor, Galano, Clark and Graham-Bermann2021), and can improve symptoms of externalizing psychopathology that are associated with self-regulation and EC in children and adolescents (Clark et al., Reference Clark, Galano, Grogan-Kaylor, Stein and Graham-Bermann2021; Jouriles et al., Reference Jouriles, McDonald, Rosenfield, Stephens, Corbitt-Shindler and Miller2009).
Conclusions
This study used multigroup LCS modeling to compare change in EC and caregiver depressive symptoms across 3 years during middle childhood and early adolescence between IPV+ and IPV− participants (i.e., those who had and had not witnessed IPV, respectively). By showing overall mean-level vulnerabilities (i.e., higher levels of caregiver depressive symptoms and lower EC scores) for the IPV+ group, and associations linking caregiver depressive symptoms and EC only for participants who witnessed IPV, this study contributes to the literature on adaptation processes in the context of IPV. Findings from this study also suggest that interventions designed to reduce IPV and improve caregivers’ depressive symptoms following experiences of IPV are likely to have favorable effects on children’s and adolescents’ EC, which may also have a protective influence on transdiagnostic psychopathology outcomes in the longer term.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423000615
Acknowledgements
The authors thank the families who participated in this project. We also thank the dedicated research team at the Gene–Environment Mood study.
Funding statement
This research was supported by grants from the National Institutes of Health R01MH077195 awarded to BLH.
Competing interests
None.







