Introduction
Although major depressive disorder (MDD) can be successfully treated with psychotherapy, more than half of all patients do not respond to treatment (Cuijpers et al., Reference Cuijpers, Miguel, Harrer, Plessen, Ciharova, Ebert and Karyotaki2023). Moreover, relapse after successful treatment is common. Response rates vary from 37% posttreatment to 48% at 13–24 months follow-up (Cuijpers et al., Reference Cuijpers, Karyotaki, Ciharova, Miguel, Noma and Furukawa2021), and up to 50% of the patients diagnosed with MDD relapse after receiving successful psychotherapy (Ali et al., Reference Beck, Steer and Brown2017; Steinert, Hofmann, Kruse, & Leichsenring, Reference Steinert, Hofmann, Kruse and Leichsenring2014; Vittengl, Clark, Dunn, & Jarrett, Reference Vittengl, Clark, Dunn and Jarrett2007). Response rates seem comparable for psychotherapy and pharmacotherapy (Cuijpers et al., Reference Cuijpers, Noma, Karyotaki, Vinkers, Cipriani and Furukawa2020), while relapse rates have reported to be lower in psychotherapy compared to pharmacotherapy or control conditions (Bockting, Hollon, Jarrett, Kuyken, & Dobson, Reference Bockting, Hollon, Jarrett, Kuyken and Dobson2015; Cuijpers et al., Reference Cuijpers, Hollon, Van Straten, Bockting, Berking and Andersson2013a). Finding ways to improve the success of psychotherapy is needed to optimize outcomes in the treatment of MDD.
One way to improve outcomes might be to enhance the frequency of the psychotherapy sessions. A meta-analysis and large naturalistic study have linked enhanced session frequency with better psychotherapy outcomes (Cuijpers, Huibers, Daniel Ebert, Koole, & Andersson, Reference Cuijpers, Huibers, Daniel Ebert, Koole and Andersson2013b; Erekson, Lambert, & Eggett, Reference Erekson, Lambert and Eggett2015) and it was recently shown in a randomized trial that enhancing the session frequency from once weekly to twice weekly sessions in cognitive behavioral therapy (CBT) and interpersonal psychotherapy (IPT) for MDD leads to less drop-out and a quicker and larger decrease in depressive symptoms posttreatment (Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020). While studies in patients with anxiety report equal or better follow-up outcomes for higher v. lower frequency sessions (Bohni, Spindler, Arendt, Hougaard, & Rosenberg, Reference Bohni, Spindler, Arendt, Hougaard and Rosenberg2009; Chambless, Reference Chambless1990; Herbert, Rheingold, Gaudiano, & Myers, Reference Herbert, Rheingold, Gaudiano and Myers2004), the long-term effects of session frequency in MDD are unclear.
The present study investigated the long-term effects of once weekly v. twice weekly sessions of CBT and IPT for depression. The primary hypothesis was that twice weekly sessions lead to greater reduction of depressive symptoms and secondary outcomes in the follow-up phase of treatment (i.e. from 6 months up to 24 months after start of treatment). In addition, we expected rates of reliable change, remission, response and relapse to be superior in the patients who received the twice weekly session frequency. Because studies that compared the long-term effects of different psychotherapies are scarce and mostly focused on the long-term effects of CBT (Bockting et al., Reference Bockting, Hollon, Jarrett, Kuyken and Dobson2015; Cuijpers et al., Reference Cuijpers, Karyotaki, Ciharova, Miguel, Noma and Furukawa2021), we will additionally compare the long-term effects of CBT v. IPT. Based on a recent RCT that showed comparable effects of CBT v. IPT in the long run (Lemmens et al., Reference Lemmens, Van Bronswijk, Peeters, Arntz, Hollon and Huibers2019), we did not expect significant differences in depressive symptoms during the 12–24 months follow-up period nor differences in reliable change, remission, response or relapse rates between the treatment modalities.
Methods
Trial design and participants
Data come from a multicentre trial using a 2 × 2 factorial design testing the effects of session frequency in CBT v. IPT in patients with MDD (Bruijniks et al., Reference Bruijniks, Bosmans, Peeters, Hollon, van Oppen, van den Boogaard and Huibers2015). The presented results will be based on this sample. Patients were recruited in nine different mental health centres. Inclusion criteria were a primary diagnosis of MDD according to the Diagnostic and Statistical Manual of Mental Disorders fourth or fith edition (DSM-IV/DSM-5)) (including chronic depression or DSM-5 persistent depressive disorder), a pre-treatment score of ⩾20 on the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996), age > 18, sufficient knowledge of the Dutch language and having access to internet facilities. Patients were excluded if they had started an antidepressant medication (ADM) or changed ADM dose in the past 3 months, who showed acute suicide risk or a diagnosis of drug or alcohol dependence or a cluster A or B personality disorder as indicated by the DSM-IV or DSM-5, or who received more than five sessions of CBT or IPT in the past year were excluded. After signing informed consent, patients were randomly assigned to one of the four conditions: 16 sessions of CBT twice a week, 16 weekly sessions of CBT, 16 sessions of IPT twice a week and 16 weekly sessions of IPT. In each condition, the 16th session was followed by four biweekly sessions. Treatment manuals were used for both interventions and both treatments consisted of a minimum of 12 and maximum of 20 45-min face-to-face sessions, depending on individual patient progress. CBT was based on the manual by Beck and colleagues (Beck, Rush, Shaw, & Emery, Reference Beck, Rush, Shaw and Emery1979) and IPT was based on the manual by Klerman and colleagues (Klerman, Weissman, Rounsaville, & Chevron, Reference Klerman, Weissman, Rounsaville and Chevron1984). Adherence to CBT was rated with the Collaborative Study Psychotherapy Rating Scale-Version 6 (Hill, O'Grady, & Elkin, Reference Hill, O'Grady and Elkin1992) and was significantly more evident in CBT than in IPT, while adherence to IPT was more present in IPT than in CBT (Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020). Therapy competence varied from poor-to-good for both treatments. Results showed that a frequency of twice weekly sessions led to less drop-out (n = 16 v. n = 32) and faster and better decrease of depressive symptoms (effect size d = 0.55; hazard ratio (HR) = 1.48) compared to the weekly sessions posttreatment (i.e. up to 6 months after start of treatment; Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020). The trial was registered with the Netherlands Trial Register (registration number NTR4856). Further details about the study design, posttreatment outcomes and quality of treatments have been described elsewhere (Bruijniks et al., Reference Bruijniks, Bosmans, Peeters, Hollon, van Oppen, van den Boogaard and Huibers2015, Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020, Reference Bruijniks, DeRubeis, Lemmens, Peeters, Cuijpers and Huibers2021). All procedures were approved by the Medical Ethical Committee of VU Medical Centre Amsterdam (registration number 2014.337).
Primary outcomes
The presence of depressive symptoms during the follow-up period was measured with the BDI-II (Beck et al., Reference Ali, Rhodes, Moreea, McMillan, GilbodyS., Leach and Delgadillo1996) and the Longitudinal Interval Follow-up Evaluation (LIFE; Keller, Reference Keller1987). The BDI-II is a 21-item self-report instrument assessing depressive symptoms over the past 2 weeks. A score of 0–13 indicated minimal depression, 14–19 indicated mild depression, 20–28 indicated moderate depression and 29–63 indicated severe depression. The BDI-II was completed online posttreatment at 6, 9, 12 and 24 months after starting treatment. The LIFE interview is a semi-structured interview that assesses episodes and symptoms of depression retrospectively and took place after the 24-month assessment to obtain a clinically rated measure of depression during the period between 12 and 24 months after start of treatment. The LIFE interview was conducted (unblinded) by phone by S. B. or clinical psychology graduate students supervised by S. B. and has shown to be reliable and valid for characterizing the course of depression for up to a year (Warshaw, Dyck, Allsworth, Stout, & Keller, Reference Warshaw, Dyck, Allsworth, Stout and Keller2001). Good internal consistency (Cronbachs' alpha between 0.73 and 0.95), test–retest reliability (between 0.73 and 0.96) and validity of the BDI-II have been previously reported (Beck et al., Reference Ali, Rhodes, Moreea, McMillan, GilbodyS., Leach and Delgadillo1996; Beck, Steer, & Garbin, Reference Beck, Steer and Garbin1988; Wang & Gorenstein, Reference Wang and Gorenstein2013).
Secondary outcomes
Secondary outcomes included a single item rating of ‘current mood’ (0, ‘worst mood ever’ to 100, ‘best mood ever’); two single items rating happiness, ‘general life happiness’ and ‘happiness today’ (1, ‘completely unhappy’ to 7, ‘completely happy’); the general health perception domain of the RAND 36-Item Health Survey (RAND-36; Van Der Zee & Sanderman, Reference Van Der Zee and Sanderman1993) and the Remission of Depression Questionnaire (RDQ; Zimmerman et al., Reference Zimmerman, Martinez, Attiullah, Friedman, Toba and Boerescu2014). At posttreatment, there were significant differences between session frequencies in current mood, happiness in general and happiness today over time and non-significant trends toward significance on the RAND-36 in favor of twice weekly sessions of either modality and trends toward significance on the RDQ positive health in favor of twice weekly sessions and IPT in particular (Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020). The RDQ and RAND-36 have shown good psychometric properties (RDQ, Cronbach's alpha = 0.97, test–retest reliability = 0.85; RAND-36, Cronbach's alpha = 0.71–0.92, test–retest reliability = 0.40–0.75; Van Der Zee & Sanderman, Reference Van Der Zee and Sanderman1993; Zimmerman et al., Reference Zimmerman, Martinez, Attiullah, Friedman, Toba and Boerescu2014). Secondary outcomes were completed online at 6, 9, 12 and 24 months after start of treatment. We additionally reported received psychological health care after end of the study treatment, which was coded as yes in case patients reported this in the LIFE interview or in the Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiCP; Hakkaart-van Roijen, Tan, & Bouwmans, Reference Hakkaart-van Roijen, Tan and Bouwmans2011).
Statistical analyses
First, study adherence on all outcome measures was described. Differences in attrition between session frequencies and treatment modalities at months 9, 12 and 24 were tested with a χ2 test. Differences in baseline characteristics (baseline BDI-II, age, gender, recurrence of depression, active employment, reported duration of symptoms) between patients with and without missing data on one of the follow-up moments or the LIFE were tested using χ2 tests (dichotomous variables) or t tests (continuous variables).
Second, similar to the analyses that were conducted to investigate the effects of session frequency on posttreatment scores (Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020), multilevel regression analyses with maximum likelihood estimation were run to investigate the long-term effect of session frequency on depression (BDI-II scores) at follow-up. Intervention was represented by two dichotomous variables: CBT v. IPT and once weekly v. twice weekly sessions. The model adjusted for baseline values by adding BDI-II baseline as a covariate in the model. The initial basic model was a two-level model with repeated measurements (level 1) nested within patients (level 2) with two two-way interactions testing the difference in change of BDI-II scores over time in days for the different session frequencies (time × frequency) and treatments (time × treatment). To avoid collinearity between the variables representing time, time in days was centred using the median time. Quadratic and cubic functions with respect to time were tested to see if they led to a better model fit. Subsequently, the addition of random levels on therapist and treatment centre were tested, followed by a test of random slopes for time on all fitted random levels. Fit of different (co)variance structures for both the random effects and residuals errors within the lowest level (repeated measurements) were compared. To explore whether the effect of session frequency was different for CBT v. IPT, a model with a three-way interaction (frequency × treatment × time) was fitted. Analyses were intention to treat, and significance levels were set at p < 0.05. Missing data were not imputed. To investigate the effects of session frequency up to the different follow-up points, models were fitted separately up to 9-, 12- and 24-month follow-up, with each model including all data collected up to the follow-up point (for example, the model up to month 12 would also include the data at follow-up point month 9). The same method was used to investigate effects on the secondary outcomes. Effect sizes from session 1 to month 24 (Cohen's d) for the primary outcomes were computed: (estimated session 1 mean − estimated mean at time i)/estimated s.d. at session 1).
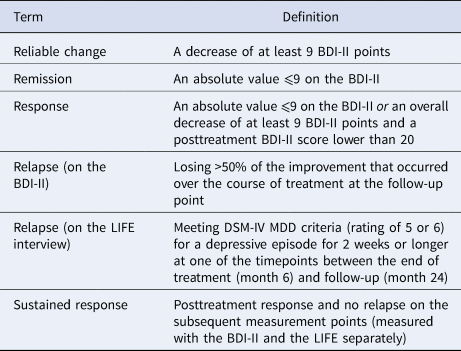
Third, rates of reliable change, remission, response and relapse were calculated. As in our outcome paper (Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020), reliable change was defined as a decrease of at least nine BDI-II points from session 1 to the follow-up, and remission as an absolute value ⩽9 on the BDI-II. In regard to relapse and following the criteria of earlier studies (DeRubeis et al., Reference DeRubeis, Zajecka, Shelton, Amsterdam, Fawcett, Xu and Hollon2019; Hollon et al., Reference Hollon, DeRubeis, Shelton, Amsterdam, Salomon, O'Reardon and Gallop2005; Jarrett, Minhajuddin, Gershenfeld, Friedman, & Thase, Reference Jarrett, Minhajuddin, Gershenfeld, Friedman and Thase2013; Lemmens et al., Reference Lemmens, Van Bronswijk, Peeters, Arntz, Hollon and Huibers2019), response was defined as a posttreatment BDI-II score ⩽9 or an overall change of at least nine BDI-II points from session 1 to the follow-up moment and a posttreatment BDI-II score lower than 20. This definition of response was chosen to be able to identify patients who show reliable change but still have a high end-of-treatment BDI-II. Relapse was defined as losing >50% of the improvement on the BDI-II that occurred over the course of treatment from session 1 to posttreatment at the follow-up point or as meeting full DSM-IV criteria for MDD (rating of 5 or 6) on the LIFE interview for 2 weeks or longer between the end of treatment (month 6) and follow-up (month 24). Sustained response was defined as meeting the criteria for response at posttreatment and no relapse at the subsequent time points and was plotted separately for the BDI-II and LIFE. An overview of all definitions can also be found in Table 1. Differences between session frequencies and treatment modalities were given by odds ratios and tested with χ2 tests. Cox regressions were used to test for differences in the time of sustained response (in days) for weekly v. twice weekly sessions, including treatment modality and the BDI-II baseline score as covariates (censoring was coded as 0, no response posttreatment or relapse as 1, days of sustained response was indicated at months 6, 9, 12 or month 24 for both the LIFE and the BDI-II).
Table 1. Overview of definitions
Fourth, two sensitivity analyses were conducted. Following the posttreatment outcome paper, sensitivity analyses tested whether the total number of sessions, the presence of a comorbid anxiety disorder or the use of antidepressants were covariates that influenced the main results at 24-month follow-up. Second, two χ2 tests tested whether having received posttreatment psychological health care after the study treatment (yes/no) differed between the different session frequencies and treatments.
Results
Study adherence
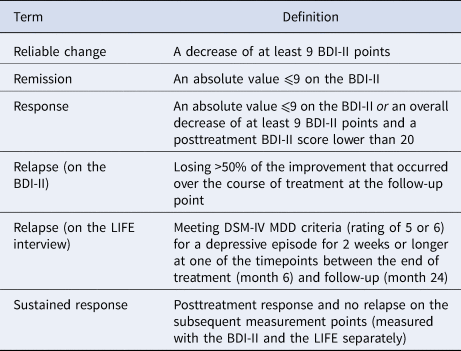
BDI-II data from 61 (30.5%), 60 (30%) and 75 (37.5%) participants were missing at months 9, 12 and 24, respectively. There were no significant differences in missing data between session frequency conditions or treatment modalities (p > 0.05 on all time points). LIFE interviews were conducted for 96 (48% of the) patients (n = 49 in the once weekly condition, n = 47 in the twice weekly condition; χ2 = 0.68, p = 0.79). Missing data were due to participants who did not want to participate anymore or could not be reached during the follow-up period. Patients with and without missing data on one of the follow-up measurements (months 9, 12 and 24) or the LIFE interview did not differ in age, gender, baseline BDI-II, recurrent depression, active employment or self-reported duration of symptoms, except that patients with missing LIFE interviews had a higher BDI-II baseline score compared to patients with whom the LIFE interview was conducted (M = 36.13, s.d. = 10.05; M = 33.17, s.d. = 9.68; t (198) = 2.11, p = 0.036). Observed means [95% confidene interval (CI)] on all outcome measures at each time point for each condition are given in Table 2.
Table 2. Observed means (standard deviations) and N on all outcome measures at each time point for each condition
Note. CBT, cognitive behavioral therapy; IPT, interpersonal psychotherapy; RAND-36, RAND 36-Item Health Survey; BDI-II, Beck Depression Inventory-II; RDQ, Remission of Depression Questionnaire. Note that for the RDQ a lower score indicates better functioning in the respective subscale.
Long-term effects of session frequency on the primary and secondary outcomes
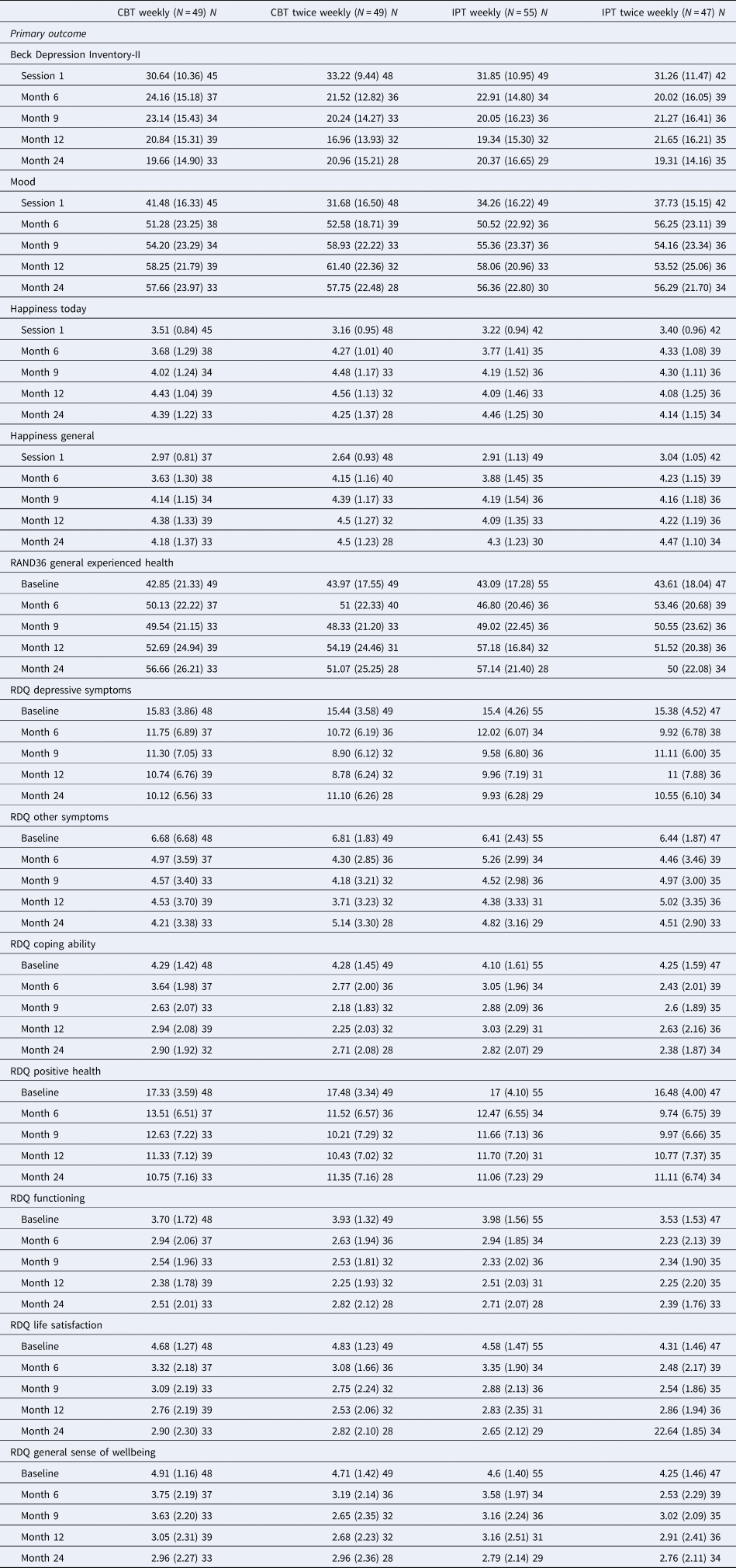
Twice weekly sessions showed a significant advantage over weekly sessions on the BDI-II up through month 9 (3.17 points on the BDI-II, between group difference in effect size d = 0.42, p = 0.009), but that advantage was no longer significant at month 12 (0.72 points on the BDI-II, between group difference in effect size d = 0.09, p = 0.06) or month 24 (1.46 points on the BDI-II, between group difference in effect size d = 0.15, p = 0.90); estimated means for weekly v. twice weekly sessions at session 1 and at month 24: 31.51 (95% CI 29.11–33.92) to 20.26 (95% CI 16.06–24.46) for once weekly CBT; 31.38 (95% CI 28.99–33.76) to 18.66 (95% CI 14.32–22.99) for twice weekly CBT; 32.83 (95% CI 30.48–35.18) to 21.74 (95% CI 17.48–26.00) for once weekly IPT and 32.69 (95% CI 30.29–35.10) to 20.14 (95% CI 15.95–24.33) for twice weekly IPT. There was no effect of session frequency in CBT v. IPT over time (i.e. session frequency × treatment × time interaction) in one of the models. Regarding the secondary outcomes, there was a significant difference between session frequencies over time (from baseline up to month 24) in favor of the weekly sessions for happiness today (estimated mean difference at month 24, 0.28 points on happiness today; effect size d = 0.34, p = 0.002). Estimated means (95% CI) on all outcome measures at each time point for each condition of the 24-month model are given in online Supplementary Data Supplement S1. The mixed regression model on the BDI-II (without and without the three-way interaction) and happiness today scores up to month 24 can be found in online Supplementary Data Supplement S2. Figure 1 depicts change in estimated BDI-II means between conditions over time.
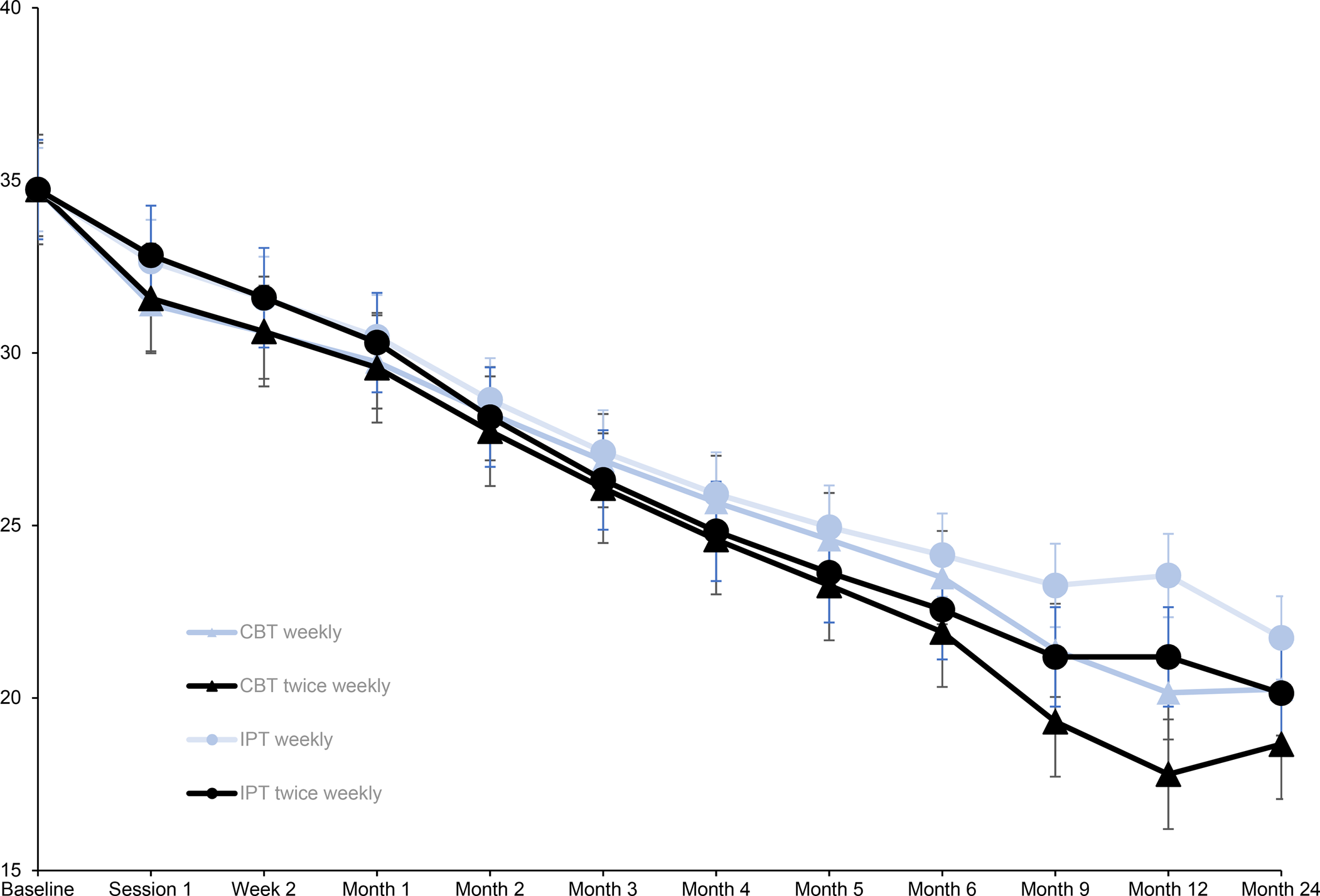
Figure 1. Estimated means on the BDI-II per condition over time. Note that for illustrative purposes, the y-axis starts at BDI-II = 15. Note that BDI-II scores at baseline present the observed mean BDI-II score for all conditions at baseline. The x-axis presents the moment of measurement: baseline, before session 1, and 2 weeks and 1–24 months after the first session. Error bars present the estimated standard error (except for the baseline values that show the observed standard errors). CBT, cognitive behavioral therapy; IPT, interpersonal psychotherapy.
Long-term effects of CBT v. IPT on the primary and secondary outcomes
There were no significant differences in change over time on the BDI-II between CBT and IPT up to month 9 or month 12, but treatment modalities differed significantly over time up to month 24 in favor of CBT (0.16 points on the BDI-II; effect size d = 0.04, p = 0.018). There was a significant difference between treatment modalities over time (from baseline up to month 24) in favor of CBT on the general sense of wellbeing subscale of the RDQ (0.59 points on the RDQ general sense of wellbeing subscale; difference in effect size d = 0.21, p = 0.032).
Reliable change and remission rates
Reliable change and remission rates are presented in online Supplementary Data Supplement S3. At month 24, 15 (45.5%) (CBT) and 14 (56%) (IPT) patients showed reliable change in the weekly conditions, whereas 17 (60.7%) (CBT) and 21 (65.6%) (IPT) patients showed reliable change in the twice weekly conditions (once weekly v. twice weekly: χ2 = 2.13, p = 0.14, odds ratio: 1.72). At month 24, 11 (33.3%) (CBT) and 11 (37.9%) (IPT) patients showed remission in the weekly conditions, whereas 7 (25%) (CBT) and 10 (28.6%) (IPT) patients showed remission in the twice weekly conditions (once weekly v. twice weekly: χ2 = 1.05, p = 0.30, odds ratio: 0.67). There were no significant differences between treatment modalities.
Relapse
Information on response was missing for 53 patients (26.5%). Fifty-six patients (38.1% of the available data, n = 147) showed response to treatment. Response did not differ significantly between session frequencies or treatment modalities (χ2 = 1.89, p = 0.17, odds ratio: 1.60; χ2 = 0.16, p = 0.68, odds ratio: 1.14, respectively). Of the 56 patients who responded to treatment, 6 (11.8% of n = 51), 5 (10% of n = 50) and 11 (24.4% of n = 45) patients reported relapse according to the BDI-II at months 9, 12 and 24, respectively. Relapse according to the BDI-II did not differ significantly between session frequencies or treatment modalities. Of the 56 patients who responded to treatment, 35 patients completed the LIFE of which 14 patients (40%) relapsed in the follow-up period up to month 24. Relapse on the LIFE did not differ significantly between session frequencies or treatment modalities. Relapse rates on the BDI-II and LIFE are presented in online Supplementary Data Supplement S4.
Sustained response
In the model that investigated time until relapse on the BDI-II, there was no significant difference between session frequencies or treatment modalities in time to relapse (HR = 0.86, 95% CI 0.71–1.04, p = 0.14 and HR = 0.92, 95% CI 0.76–1.12, p = 0.44, respectively). There was also no significant difference between session frequencies or treatment modalities in time to relapse on the LIFE (HR = 0.88, 95% CI 0.73–1.08, p = 0.24 and HR = 0.96, 95% CI 0.78–1.17, p = 0.69, respectively). Sustained response on the BDI-II is presented in Fig. 2. Sustained response on the LIFE is presented in online Supplementary Data Supplement S5.
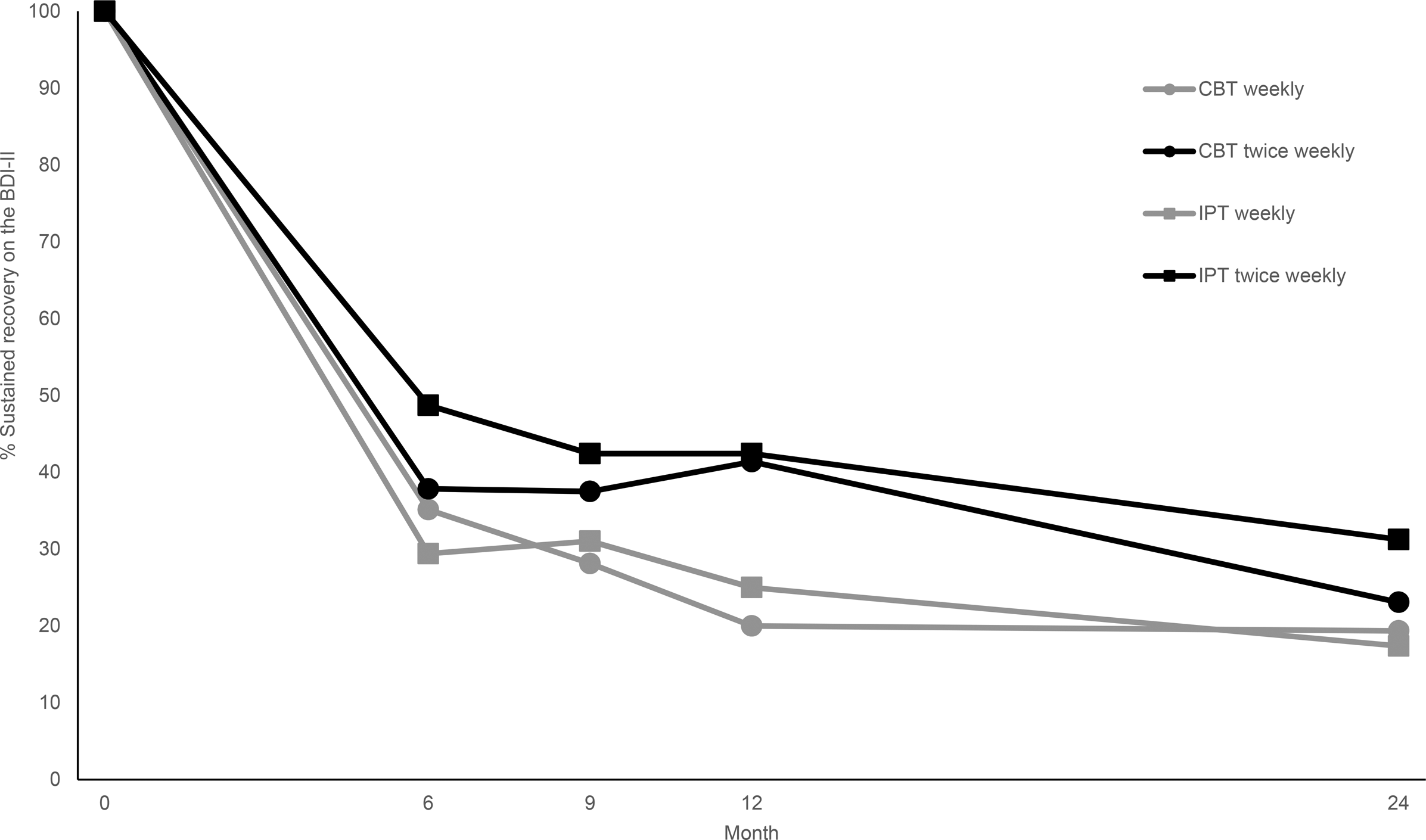
Figure 2. BDI-II, Beck Depression Inventory-II (BDI-II); CBT, cognitive behavioral therapy; IPT, interpersonal psychotherapy. Note that sustained response was defined as posttreatment response and no relapse on the subsequent measurement points (months 9, 12 and 24 follow-up). The percentage at month 6 presents the percentage of responsers, the percentages at month 9, 12 and 24 the percentage of individuals who showed response and no relapse up to the respective time point. Available data was n = 147, n = 126 and n = 125 for these time points respectively.
Sensitivity analyses
The total number of sessions, the presence of a comorbid anxiety disorder or the use of antidepressants were not significant covariates and did not influence the results. There was no difference between session frequencies of treatment modalities in having received mental health treatment after the study treatment (46.7% in the once weekly condition v. 53.1% in the twice weekly condition; χ2 = 0.51, p = 0.47; 51.6% in CBT v. 48.4% in IPT; χ2 = 0.13, p = 0.72).
Discussion
There were no significant differences in decrease of depressive symptoms between once weekly v. twice weekly sessions of CBT and IPT for depression at long-term follow-up 24 months after the start of treatment, indicating that the advantage observed for the higher session frequency at posttreatment dissipated over time. However, depression severity decreased after psychotherapy ended in all conditions, and these effects were most pronounced in the CBT twice weekly group. Although sustained response seemed to hold up longer in patients who received the higher session frequency, these differences dissipated over time and were not significant when tested up to month 24. A comparison between CBT and IPT showed a significant difference in the decrease of depressive symptoms over time in favor of CBT, but the difference in effect size at month 24 was clinically small. About 40% of the patients responded to treatment, of which 20–40% (depending on the definition of relapse) experienced relapse during the follow-up period. There were no significant differences between session frequencies or treatment modalities in reliable change, response, remission or relapse.
To our knowledge, this was the first randomized trial investigating the long-term effects of session frequency in a depressed sample. Response to treatment was low compared to previous studies, who used the same definitions of response, and reported response rates up to 50–60% (Lemmens et al., Reference Lemmens, Van Bronswijk, Peeters, Arntz, Hollon and Huibers2019; Luty et al., Reference Luty, Carter, McKenzie, Alma, Frampton, Mulder and Joyce2007), but relapse rates were comparable to earlier studies, where about one-third of the responders relapsed during follow-up (Lemmens et al., Reference Lemmens, Van Bronswijk, Peeters, Arntz, Hollon and Huibers2019; Vittengl et al., Reference Vittengl, Clark, Dunn and Jarrett2007). Although our results indicated that, from baseline till 24-month follow-up, CBT may lead to more decrease in depressive symptoms compared to IPT, the difference in effect sizes was ignorable by month 24 and there were no differences between treatment modalities on response or relapse. This finding is in line with the two other studies that pointed to no differences in the long-term effects of CBT v. IPT for depression (Lemmens et al., Reference Lemmens, Van Bronswijk, Peeters, Arntz, Hollon and Huibers2019; Shea et al., Reference Shea, Elkin, Imber, Sotsky, Watkins, Collins and Parloff1992).
Future studies should investigate individual differences in the long-term effects of session frequency in depression and preferably in larger samples. Twice weekly sessions were not beneficial over the long run, but this conclusion might not hold for everyone. Using the same dataset, we recently showed that different individuals benefit from different session frequencies in the acute phase of treatment (Bruijniks, Van Bronswijk, et al., Reference Bruijniks, Meeter, Lemmens, Peeters, Cuijpers, Renner and Huibers2022). Using machine learning techniques, we identified patient characteristics that predicted who benefits from once weekly respectively twice weekly session frequencies at posttreatment in this specific sample. A future study should investigate whether similar predictions can be made for the long-term effects of session frequency and whether these identified patient characteristics can be generalized to other samples and clinical practice (Bruijniks, Van Bronswijk, et al., Reference Bruijniks, Van Bronswijk, Derubeis, Delgadillo, Cuijpers and Huibers2022; van Bronswijk et al., Reference van Bronswijk, DeRubeis, Lemmens, Peeters, Keefe, Cohen and Huibers2019). In addition, as the current sample consisted mostly of severely depressed patients, another possibility is that twice weekly sessions in combination with the current duration of treatment are not enough to induce long-term effects in patients who are severely depressed. Different severity levels may require different session frequencies and different therapy doses and it would be interesting to investigate whether higher session frequencies or doses would be more beneficial for more severely depressed samples.
Strengths of the present study were the external validity: patients were seen by a high number of different therapists in different treatment centres that showed a varying amount of therapy competence (Bruijniks et al., Reference Bruijniks, Lemmens, Hollon, Peeters, Cuijpers, Arntz and Huibers2020). A limitation of the present study was the large amount of missing data, especially for the LIFE interview. The sample who conducted the LIFE interview had somewhat higher BDI-II baseline scores compared to the samples whose LIFE interview was missing. This might explain the slightly elevated relapse rates on the LIFE compared to the relapse rates as computed on the BDI-II, but we controlled for the BDI-II baseline scores in the Cox regression. Other comparisons showed no important baseline differences between patients with or without missing data. The varying amount of therapy competence, although increasing external validity, can also be considered as a limitation: violations to the treatment protocol might compromise the effects of the change mechanisms that enhance the treatment effects in a higher session frequency (Bruijniks, Meeter, et al., 2022) leading to less power to find a differential effect between session frequencies over time. Moreover, CBT twice weekly seemed to do somewhat better over time compared to the other conditions and the absence of significance points to a lack of statistical power.
In summary, the benefits of a greater session frequency are apparent after psychotherapy has ended but dissipate over time. Response was quicker and higher in the short term, but these differences were not maintained over time: although further decreases on the BDI-II were most pronounced in CBT twice weekly and sustained response seemed to hold up longer in patients who received the higher session frequency, differences were not significant at 24-month follow-up. Implementation of a higher session frequency in clinical practice might be beneficial for reducing drop-out and for a greater response quicker in the acute-treatment phase but, on the basis of the present findings, does not seem to have an established advantage on symptom reduction in the long term.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291723002143
Acknowledgements
We acknowledge the contribution of participating patients and therapists at Altrecht, GGZ inGeest, GGZ Oost-Brabant, Pro Persona, PsyQ Amsterdam, PsyQ Den Haag, PsyQ Haarlem, PsyQ Leiden and Riagg Maastricht. Without their cooperation, the trial would have been impossible to conduct. Furthermore, we gratefully thank Danielle Tilburgs, Nicole Billingy, Kris Wijma, Sofie Jansen and Annie Hendriks for their assistance during the data collection.
Author contributions
S. D. H., J. B., F. P. M. L. P., P. V. O., P. C., A. A. and M. J. H. H. obtained funding for this study. All authors contributed to the design of the study. F. P. M. L. P., P. D., L. W., P. V. O., M. V. D. B. and J. S. were involved in the recruitment of patients, therapists and coordination of the treatments. S. J. E. B. coordinated the recruitment of patients and data collection. S. J. E. B. conducted the analyses. S. J. E. B., M. J. H. H., J. T., S. D. H. and A. A. were involved in the interpretation of the analyses. S. J. E. B. wrote the manuscript. Authors read, contributed to and approved the final manuscript.
Financial support
This study was funded by ZonMw and Stichting tot Steun VCVGZ. The funders were not involved in the study design; the collection, analysis and interpretation of data; the writing of the report or the decision to submit the article for publication.
Conflict of interest
None.
Data availability
Data will be available upon request.