The rate of behavioural and psychiatric disorders in children with epilepsy is estimated to be double that of the normal childhood population. 1 This may be a conservative estimate, as the Office for National Statistics reports that more than a third of children with neurological problems have mental health problems. 2 In children with epilepsy, attention problems and internalising problems are thought to be more frequent than externalising problems. Reference Austin and Caplan3
A recent survey highlighted high levels of unmet mental health needs in children with epilepsy. Reference Smith, Siddarth, Zima, Sankar, Mitchell and Gowrinathan4 Children with epilepsy have complex, often coexisting health needs whose treatment requires a holistic, multidisciplinary approach. The Scottish Intercollegiate Guidelines Network (SIGN) emphasise the importance of ‘close liaison with education, social work and the voluntary sector’ and state that ‘children with academic or behavioural difficulties should have appropriate educational and/or psychological assessment and intervention’. 1 Paediatric neurologists are more likely than other paediatricians to refer children to the child and adolescent mental health service (CAMHS), but describe resistance from child psychiatrists and other mental health professionals to assessment and treatment of these patients. The SIGN guidelines make recommendations for good practice in managing mental health needs of children with epilepsy, which read alongside with the Scottish Framework for CAMHS. 1,5
The West of Scotland Neurosciences Service at Yorkhill has a range of disciplines including paediatric neurology, neuropsychology, specialist nurses and a teacher. Hospital-based liaison CAMHS comprises paediatric psychology, neuropsychology and the liaison team (including consultant psychiatrists, specialist nurses and a clinical psychologist). Early intervention and treatment of less complex mental health problems are managed by paediatric psychologists. Neuropsychology provides specialist assessments and interventions, embedded within neurosciences, yet part of liaison CAMHS. The liaison team aims to advise on community CAMHS referral where appropriate and to provide services to children with complex and severe psychiatric disorders who require hospital-based multidisciplinary CAMHS input, for example where epilepsy and mental health treatments require close collaboration between CAMHS and neurosciences. A recent audit has shown that an epilepsy diagnosis is associated with prolonged input from the liaison team. Reference Cordeiro, Morton and McWilliam6
There are approximately 3500 children with epilepsy in Scotland, 7 about half of whom live in the West of Scotland. Thus, the catchment population may contain around 600 children with epilepsy and mental disorder. Community CAMHS may provide services for some of these and a subgroup with more complex needs will be referred to the liaison team.
Method
Liaison team members reviewed their case-loads and identified all current patients with epilepsy and psychiatric disorders as of 10 ctober 2007 (n=22). Psychiatric and medical case notes of these patients were systematically reviewed to determine service involvement.
Results
Most patients were referred to the liaison team from neurosciences; one each came from CAMHS and cardiology. Mean patient age was 12 years (range 6–19). Two-thirds of the patients were boys. The median duration of liaison CAMHS involvement was 18 months (range 2–58). Thirteen of these children were in mainstream education, eight attended special schools and one attended nursery school. Fifteen were from two-parent families and six from single-parent families (a further two families separated since referral); one was cared for by a relative. Eight children had a family history of psychiatric disorder.
Diagnoses
Epilepsy diagnoses included partial (simple and complex), focal and myoclonic epilepsy, startle seizures and polymorphous epilepsy. Underlying aetiology included cortical malformation, mesiotemporal sclerosis, limbic encephalitis, multiple haemangiomas, leukaemia and Angelman syndrome. Half of the patients had two or more coexisting psychiatric diagnoses (Fig. 1).
Interventions and interfaces
Figure 2 shows the range of interventions used, and indicates the interfaces between the liaison team and other teams and agencies that were identified in the review of case records.
Joint consultation
Most patients received joint clinic appointments and were seen by a neurologist and a psychiatrist working together. In many cases there was repeated joint review. Joint consultation with neuropsychology was also frequent and most patients had had neuropsychological assessment.
Therapeutic interventions
Fourteen patients received some individual therapy (including brief interventions and psychoeducation); for seven, this was provided by the liaison team. Paediatric psychologists and a community-based CAMHS worker conducted sessions in four cases. Other individual treatments were jointly conducted with other CAMHS staff. Family work was frequent, with seven family interventions by the liaison team and the remainder by community CAMHS. Drug treatment decisions were often shared during joint clinics with neurologists. Seven patients received psychotropic medication. In four cases, psychotropic medication was being reserved until the behaviour-modifying effects of anti-epileptic drugs had been addressed. Two patients had attention-deficit hyperactivity disorder, one of whom was treated with dexamphetamine. The other (a new referral) was being considered for neurostimulant treatment. Three patients were treated with risperidone for behavioural disorder with neurodisability and three received melatonin for sleep disturbance.
Community-based services
Community CAMHS were frequently involved in the care of liaison team patients, with specialist learning disability CAMHS involved in two cases. The liaison team directly contacted schools in 10 cases and educational psychology input was noted in 13. Social work services were involved in half of the cases, with input in eight of the nine cases known to the team for the longest period. In two cases, referral to social work did not result in their involvement. Two patients were on the child protection register. Half the patients had one or more multi-agency case conferences to discuss their needs.
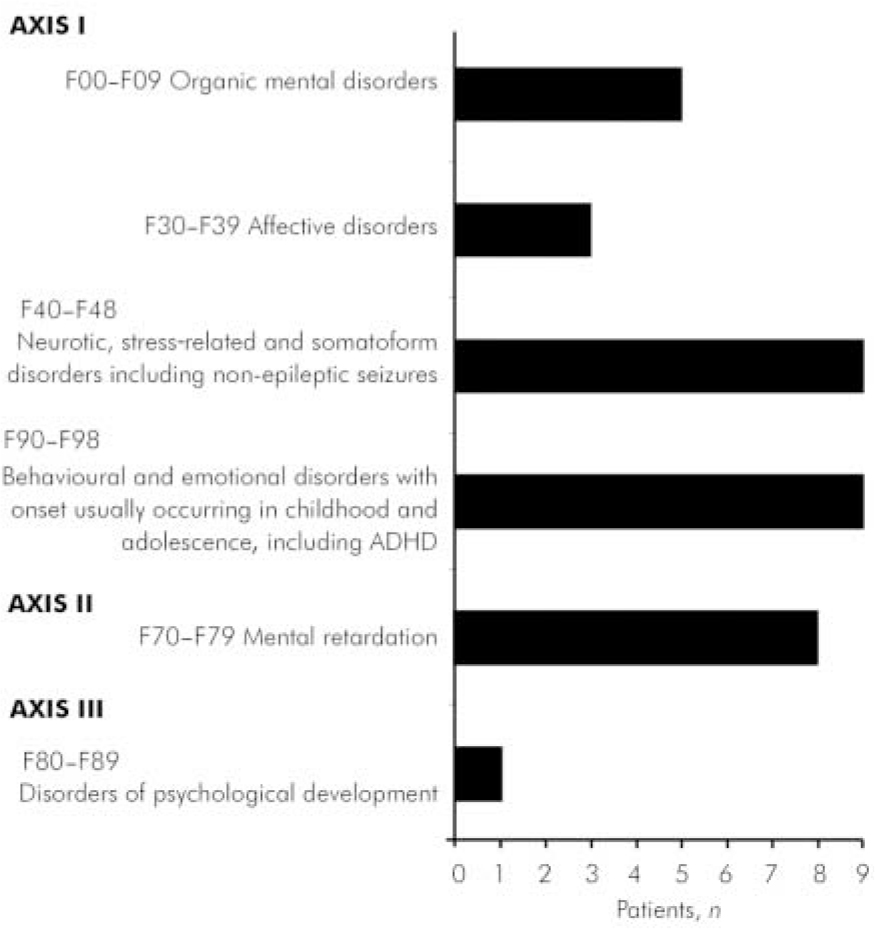
Fig. 1. Psychiatric diagnoses (ICD–10, multi-axial version). ADHD, attention-deficit hyperactivity disorder.
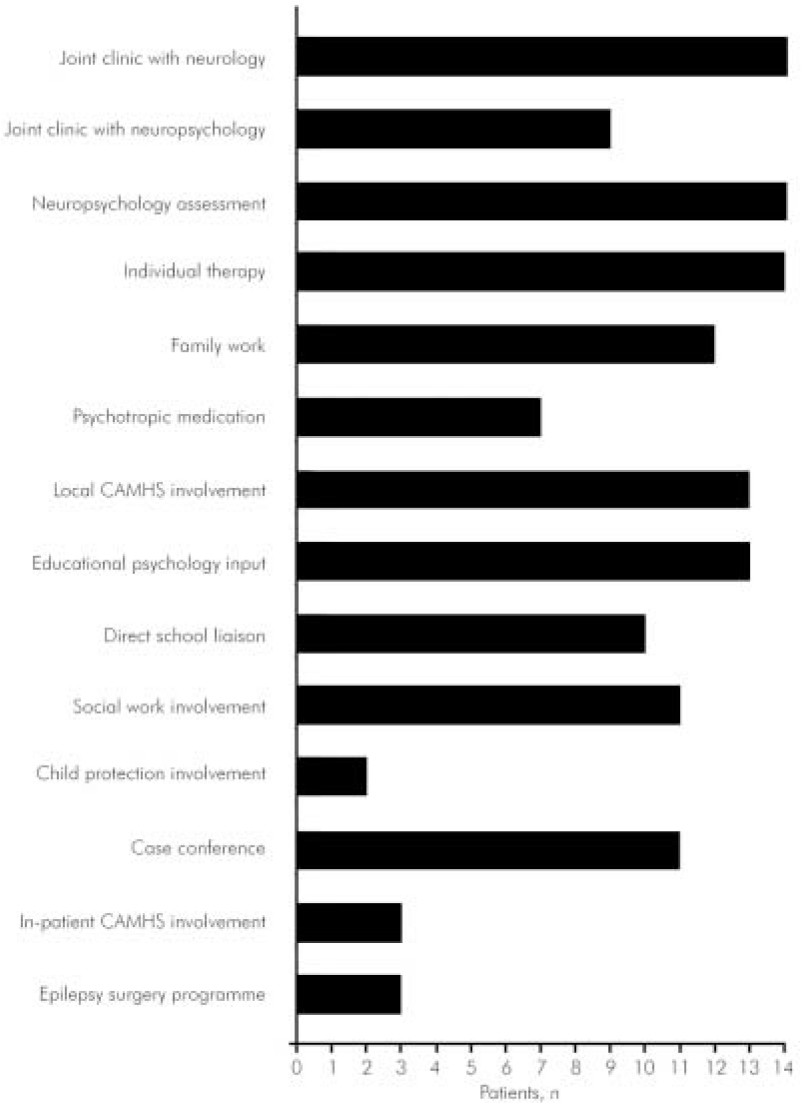
Fig. 2. Interventions and interfaces. CAMHS, child and adolescent mental health service.
Tier IV/tertiary care
Three patients had been admitted to a child psychiatry in-patient unit. One had an emergency admission with post-ictal behavioural changes. One was admitted for fuller assessment of a complex presentation. One attended the ward as a day patient in preparation for epilepsy surgery. Three patients were within the Great Ormond Street epilepsy surgery programme: one postoperative, one awaiting surgery and one patient being considered for surgery.
Discussion
Close CAMHS liaison with neurosciences is evidenced both by the route of referral and the frequency of joint clinics with neurology and neuropsychology. No clear pattern of neurological or psychiatric diagnosis appeared to be associated with referral to the liaison team. The SIGN guidelines recommend that all children with epilepsy should have their behavioural and academic progress reviewed on a regular basis by the epilepsy team. These recommendations appear to have been followed in cases referred to the liaison team. The SIGN guidelines also advise that if a child experiences cognitive or behavioural adverse effects from a specific anti-epileptic drug, then an alternative drug should be considered. It could not be determined how many patients suffered adverse effects from anti-epileptic drugs, but joint approaches facilitate review of such effects. Psychotropic medication was used in accordance with SIGN guidelines, which state that neurostimulants, risperidone and melatonin ‘should not be withheld when indicated in children with epilepsy and associated behavioural and psychiatric disorders’. 1
The Scottish Executive Framework for CAMHS states that ‘support and intervention is delivered as far as possible in the child's usual environment and within universal children's services’; 5 the linking of liaison activity to community-based service involvement reflects this approach. Psychological therapies were provided in a community setting when appropriate. However, frequent hospital attenders benefited from psychological input linked to other appointments and for children with complex clinical needs a combined input from liaison psychiatry and neurosciences was helpful. Some difficulties arose in obtaining social work involvement but it is not surprising that this agency's involvement featured with children with more extended input from the liaison team. Liaison with schools and educational psychology input was evident in a number of cases. Community CAMHS routinely link to education, and this input in some cases, as well as the neurosciences own teacher's involvement, reduced the need for direct school contact by the liaison team. Although community links are important, the involvement of other highly specialist services (in-patient child psychiatry and epilepsy surgery) reflects the specialist nature of referrals to the team.
Conclusions
The children reviewed constitute a small subset of a vulnerable group of neurology patients for whom the provision of a specialist liaison service offers an opportunity for better-quality care. Services were provided in line with policy guidelines. The liaison team offers continuity in the development of joint working with neurosciences colleagues in the hospital, while maintaining connections with community CAMHS provided alongside other children's services across the West of Scotland. Although this liaison model does not directly address the needs of the large number of children affected by epilepsy and mental disorder, it facilitates links between agencies to support the development of services for this group and can meet the needs of those with the most complex presentations.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.