CLINICIAN'S CAPSULE
What is known about the topic?
Prehospital point of care ultrasound (POCUS) has been widely used in European and Scandinavian countries where it changes patient management.
What did this study ask?
What is the current POCUS use among Canadian aeromedical service (AMS) providers?
What did this study find?
POCUS in AMS is available in Prairie Provinces. The Maritimes and the Yukon report plans to introduce it within the next year.
Why does this study matter to clinicians?
This study informs clinicians of the current AMS POCUS use and may aid in the development of prehospital training curricula.
INTRODUCTION
Point of care ultrasound (POCUS) is quickly becoming the standard of care in emergency medicine.Reference Olszynski, Kim, Chenkin and Rang1 Ultrasound generated images have been shown to aid in physical examination, diagnosis, and triage of patients in the field.Reference Nelson, Melnick and Li2 There is growing evidence that prehospital POCUS may change patient management, expedite diagnostic and therapeutic care and decrease time to definitive management.Reference Botker, Jacobsen, Rudolph and Knudsen3–Reference O'Dochartaigh, Douma, Alexiu, Shell and MacKenzie5 Aeromedical services providers may use POCUS both in and out of aircraft. In-flight POCUS assessments by paramedics have been shown to have high rates of correlation (positive predictive value and negative predictive value) when compared with in-hospital imaging and operating room reports.Reference Yates and Baylous6,Reference Press, Miller and Hassan7 Aeromedical services in several European and Scandinavian countries have been using POCUS for many years.Reference Nelson and Chason8 Although a recent Danish systematic review did not gather enough evidence to show improved patient outcomes, it concluded that POCUS is feasible and changes management in trauma, cardiac arrest, and patients with breathing difficulty.Reference Botker, Jacobsen, Rudolph and Knudsen3 A 2018 German cohort study showed prehospital ultrasound changed management in 49.5% of patients, 33% of which were transport related changes.Reference Scharonow and Weilbach9
A 2014 survey of North American emergency medical services (EMS) directors (ground EMS and aeromedical services) showed that only 4.1% of ground EMS and 3.7% of aeromedical services used POCUS while 21% of directors were considering it.Reference Taylor, McLaughlin, McRae, Lang and Anton10 Canada faces unique and significant patient transport and diagnostic challenges due to its landscape and population density heterogeneity. POCUS in the hands of aeromedical services providers could conceivably be beneficial to Canadian patients, especially in remote geographic locations. Current Canadian data on POCUS adoption and use among aeromedical services providers are lacking. The purpose of this study was to describe current ultrasound use among Canadian aeromedical service providers.
METHODS
This is a cross-sectional observational study using an online survey. The survey was developed using the FluidSurveysTM (San Francisco) and distributed by means of email to all directors of government-funded (fully or partially) aeromedical services bases in Canada (Appendix 1). For the purposes of this study, aeromedical services was defined as a service providing prehospital in-flight medical care and patient transport, by means of both rotary and fixed-wing aircraft. Respondents completed the survey between March 9, 2018, to April 26, 2018. To meet inclusion criteria, the survey was to be completed by medical base directors of Canadian government-funded aeromedical services. Privately funded services were excluded from this study. The study (BEH 18-07) was assessed by the University of Saskatchewan Research Ethics Board and met the requirements for exemption of full review. Surveys were sent to directors of all known aeromedical services throughout Canada. The survey included questions regarding demographic information, POCUS availability, and barriers to its use (Appendix 1). Directors currently using ultrasound were asked additional questions regarding details of POCUS use, training of crews, and quality control. Individual base directors were not identified by name; however, the location of each base was recorded. Data were analyzed using descriptive statistics (means and medians), and between group differences were analyzed by chi-squared analysis.
RESULTS
Fourteen of 17 (82.3% response rate) directors completed the survey. As some directors were responsible for multiple bases, data were obtained for 41 of the 46 (89.1%) government-funded bases. Data from bases in Yellowknife (Northwest Territories), Inuvik (Northwest Territories), Cambridge Bay (Nunavut), Winnipeg (Lifeflight Manitoba), and Quebec were unavailable. Thirteen of 41 of the represented Canadian bases (7/14 responding directors) currently have access to POCUS onboard their aircraft, largely due to rotor wing aeromedical services. Ontario and Newfoundland and Labrador as well as Alberta Health Services Air Ambulance reported they do not have POCUS available and are not currently planning on introducing it. Bases in the Maritime region (New Brunswick, Nova Scotia/Prince Edward Island), the Yukon Territory, and Saskatchewan Air Ambulance (4/41 bases) are not currently using POCUS, but report they intend to implement it within the next year, increasing usage to 41.5% of responding Canadian bases. Twelve bases (29.2%) use exclusively fixed-wing aircraft, and six bases (14.6%) use exclusively rotary aircraft. British Columbia is currently the only province using POCUS on fixed-wing aircraft. (See Table 1 “Demographics and reported POCUS use” for each response.) Bases with rotary aircraft are significantly more likely to have POCUS (χ(2) = 11.79; p = 0.003).
Table 1. Demographics and reported POCUS use
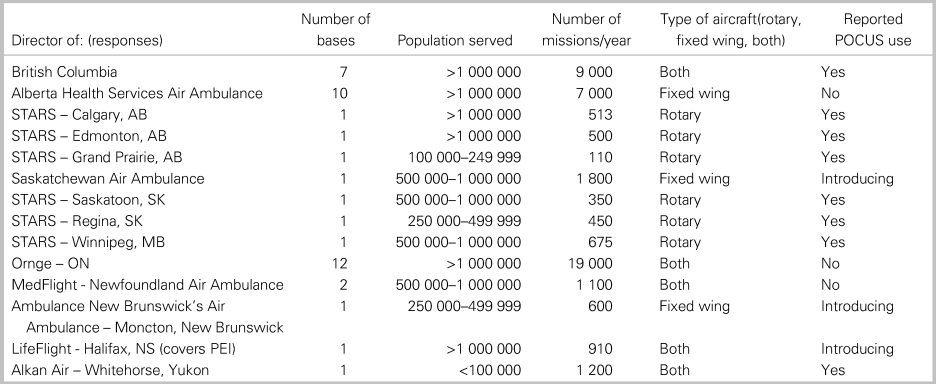
AB = Alberta; MB = Manitoba; NS = Nova Scotia; ON = Ontario; PEI = Prince Edward Island; SK = Saskatchewan.
Barriers to POCUS use
The most commonly quoted barrier to POCUS use (by nearly all directors) was cost of training and maintenance of competence. Cost of ultrasound machines was more commonly identified as a barrier by directors not using POCUS (not significant, Appendix 2).
POCUS application
POCUS use was reported by 7/14 responding directors (13/41 bases). Five of seven directors using POCUS reported obtaining scans on <25% of missions. POCUS use by aeromedical services personnel occurs at the referring hospital (71.4%) and/or in flight (50%). Assessment of abdominal free fluid, pneumothorax, and pericardial effusion in suspected tamponade are performed at all locations using POCUS, primarily by paramedics. Other commonly performed scans were for pulseless electrical activity/cardiac standstill, and abdominal aortic aneurysm (Appendix 2). All directors reported that scans were documented, most frequently in patient's chart with quality control measures in place (Appendix 2). All directors using POCUS believe it has a positive role on patient care in the emergency department and believe aeromedical services POCUS should become common practice (7/7).
DISCUSSION
Unlike Europe and Scandinavia where aeromedical services POCUS is common practice, only 31% of the represented Canadian aeromedical services bases reported POCUS use, predominantly on rotary aircraft. There is a geographical distribution with respect to its availability revealing a large geographical area of the country without plans to introduce POCUS in the near future. As POCUS is more commonly used on rotary aircraft, there may be a difference in the utility of it between mission types (transport v. scene calls). Aeromedical services providers dispatched to scene calls fly directly to the acutely ill patient, often with very limited information. It is possible that several POCUS applications are of more utility during these scene calls as compared to standard inter-facility transport; however, our study did not explore these differences, with further research required. Currently, there are no specifically defined prehospital/aeromedical POCUS training standards in Canada. Of interest, lack of such guidelines was not identified as a major barrier to POCUS use among aeromedical services base directors.
Strengths and limitations
This is the first Canadian study describing the current climate in POCUS use within aeromedical services. There are several limitations to this study. Each survey response came from a medical director of an aeromedical services base(s); however, some were accountable for many bases. And as such, it is possible we did not capture all POCUS use within Canadian aeromedical services. Despite multiple attempts, we were unable to obtain data from Quebec, Manitoba LifeFlight, and the NWT/Nunavut. There is heterogeneity within our data possibly leading to selection bias. Furthermore, the survey design left directors not currently using POCUS without access to some of the survey questions (including quality assurance measures and training specifics).
CONCLUSIONS
Prehospital POCUS is used by aeromedical services in British Columbia and on rotary aircraft in the Prairie Provinces. There are plans by local providers to further extend its use to the Maritimes and the Yukon Territory within the next year. Cost of training remains the most significant barrier to POCUS use regardless of whether or not POCUS is already available. Although all directors currently using POCUS find it valuable, further research will help inform the role of aeromedical services POCUS on patient outcomes.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.451.
Acknowledgements
The authors thank Shell Ryan for reviewing and contributing to the survey, and the University of Saskatchewan Social Sciences Research Laboratories for data analysis and report generation.
Financial support
This research received funding from the Department Head Discretionary Research Fund to cover cost of statistical analysis.
Competing Interests
None declared.



