Introduction
The two most prevalent disorders of childhood development are ASD and ADHD (American Psychiatric Association, 2013). These neurodevelopmental disorders result in atypical brain development and thus developmental trajectories. ASD impacts up to 4% of Australian children (May et al., Reference May, Brignell and Williams2020) and is associated with impaired social communication and repetitive, restricted and stereotyped behaviours (American Psychiatric Association, 2013). ADHD affects around 5–7% of children and symptoms include developmentally inappropriate levels of inattention and/or hyperactive and impulsive behaviours (Thomas et al., Reference Thomas, Sanders, Doust, Beller and Glasziou2015). Both ASD and ADHD have strong genetic causes with high heritability rates of up to 90% in ASD (American Psychiatric Association, 2013; Tick et al., Reference Tick, Bolton, Happé, Rutter and Rijsdijk2016) and 80% in ADHD (Larsson et al., Reference Larsson, Chang, D'Onofrio and Lichtenstein2014). ASD and ADHD also co-occur at high rates, with around 40–70% of children with ASD also having ADHD (Jensen & Steinhausen, Reference Jensen and Steinhausen2015; Salazar et al., Reference Salazar, Baird, Chandler, Tseng, O’sullivan, Howlin, Pickles and Simonoff2015). Conversely, around a third of children with ADHD also have ASD (Grzadzinski et al., Reference Grzadzinski, Dick, Lord and Bishop2016). Shared genetic aetiology is implicated in ASD and ADHD, and between these neurodevelopmental disorders and other mental health conditions including depression and schizophrenia (Gudmundsson et al., Reference Gudmundsson, Walters, Ingason, Johansson, Zayats, Athanasiu, Sonderby, Gustafsson, Nawaz, Jonsson, Jonsson, Knappskog, Ingvarsdottir, Davidsdottir, Djurovic, Knudsen, Askeland, Haraldsdottir, Baldursson and Stefansson2019; Lee et al., Reference Lee, Ripke, Neale, Faraone, Purcell, Perlis, Mowry, Thapar, Goddard, Witte, Absher, Agartz, Akil, Amin, Andreassen, Anjorin, Anney, Anttila, Arking and Wray2013).
Children with ASD and ADHD have more emotional and behavioural problems (EBPs) than children without these conditions (Giovagnoli et al., Reference Giovagnoli, Postorino, Fatta, Sanges, De Peppo, Vassena, Rose, Vicari and Mazzone2015). Both disorders are characterised by high levels of comorbid psychopathology (Simonoff et al., Reference Simonoff, Jones, Baird, Pickles, Happé and Charman2013; Van Steensel et al., Reference Van Steensel, Bögels and de Bruin2013). Few studies have contrasted children with ASD with comorbid ADHD (ASD + ADHD), compared to children with ASD or ADHD alone. This is likely due to the diagnostic restriction preventing their comorbid diagnosis in the DSM-IV-TR, which was removed in the DSM-5 in 2013 (American Psychiatric Association, 2000, 2013). While there are some inconsistent findings, limited research to date suggests children with ASD + ADHD have more behaviour and emotional problems than children with ASD or ADHD alone (Gargaro et al., Reference Gargaro, May, Tonge, Sheppard, Bradshaw and Rinehart2014). Furthermore, children with ASD + ADHD show more adaptive functioning impairments than children with ADHD and appear to have additive effects from each condition in areas of executive functioning (Ashwood et al., Reference Ashwood, Tye, Azadi, Cartwright, Asherson and Bolton2015; Tye et al., Reference Tye, Asherson, Ashwood, Azadi, Bolton and McLoughlin2014).
Over childhood and adolescence, research suggests a reduction in core symptoms of ASD/ADHD but there may be an increase in other psychiatric problems (Larsson et al., Reference Larsson, Larsson and Lichtenstein2004; Yoshimasu et al., Reference Yoshimasu, Barbaresi, Colligan, Voigt, Killian, Weaver and Katusic2012). Research suggests that the symptoms of ASD either remain stable (Simonoff et al., Reference Simonoff, Kent, Stringer, Lord, Briskman, Lukito, Pickles, Charman and Baird2020) or reduce over adolescence (Gray et al., Reference Gray, Keating, Taffe, Brereton, Einfeld and Tonge2012). Similarly, symptoms of ADHD may reduce during adolescence (Larsson et al., Reference Larsson, Larsson and Lichtenstein2004). There are few studies exploring EBPs over time using longitudinal designs with these groups, with some contradictory findings. For example, a study of ASD with only two time points suggest EBPs may decrease from 12 to 16 years (Simonoff et al., Reference Simonoff, Jones, Baird, Pickles, Happé and Charman2013), while others suggest there is an increase in anxiety and depression symptoms from 13 years onward (Gotham et al., Reference Gotham, Brunwasser and Lord2015). One study exploring children with ASD from 4 to 13 years showed pro-social behaviour on the SDQ increased and peaked at around 12 years, similar to children with no diagnosis, however the total SDQ and other subscales were not reported (Russell et al., Reference Russell, Golding, Norwich, Emond, Ford and Steer2012). Another study identified subgroups of increasing, decreasing or persistent emotional and behavioural problems in adolescents with ADHD (Zendarski et al., Reference Zendarski, Mensah, Hiscock and Sciberras2021). Generally, children with ADHD have been found to have more EBPs on the SDQ when younger (aged 6–10 years) compared to when older (11–18 years) but using a cross sectional design (Becker et al., Reference Becker, Steinhausen, Baldursson, Dalsgaard, Lorenzo, Ralston, Döpfner and Rothenberger2006).
Not surprisingly, parents of children with ASD/ADHD also experience higher rates of psychopathology and psychological distress than the general population of parents (Karst & Van Hecke, Reference Karst and Van Hecke2012; Tarabek, Reference Tarabek2011; Theule et al., Reference Theule, Wiener, Tannock and Jenkins2013; Van Steijn et al., Reference Van Steijn, Oerlemans, Van Aken, Buitelaar and Rommelse2014; Wesseldijk et al., Reference Wesseldijk, Dieleman, van Steensel, Bartels, Hudziak, Lindauer, Bögels and Middeldorp2018). This may relate to numerous factors including difficulty parenting children who have high levels of EBPs; plus parents may have underlying biological vulnerabilities to mental health conditions given the genetic aetiology of ASD/ADHD (Van Steijn et al., Reference Van Steijn, Oerlemans, Van Aken, Buitelaar and Rommelse2014). Parental stress and depression is higher parents of children with ASD and ADHD than in parents of children with other psychopathology such as anxiety disorders or other developmental disorders (Singer, Reference Singer2006; Telman et al., Reference Telman, van Steensel, Maric and Bögels2017). Parent stress has been associated with behaviour problems, lower IQ and adaptive behaviour in children with ASD (Giovagnoli et al., Reference Giovagnoli, Postorino, Fatta, Sanges, De Peppo, Vassena, Rose, Vicari and Mazzone2015). In ADHD child conduct problems are associated with more parent stress (Theule et al., Reference Theule, Wiener, Tannock and Jenkins2013).
There has been less exploration of the impact of having a child with both ASD + ADHD relative to those with ASD or ADHD alone. Van Steijn et al. (Reference Van Steijn, Oerlemans, Van Aken, Buitelaar and Rommelse2014) found parents of children with ASD or ASD + ADHD reported more depressive symptoms than parents of children with ADHD alone. In contrast, another study reported more stress relating to attachment and depression in parents of children with ADHD than ASD or ASD + ADHD, although those with ASD + ADHD showed a unique profile (Miranda et al., Reference Miranda, Tárraga, Fernández, Colomer and Pastor2015). These are the only two studies the authors are aware of that have explored parent mental health between these three groups.
Taken together, there are increased levels of psychological distress in parents, and EBPs in children with either ASD or ADHD, which appears further exacerbated in ASD + ADHD. To date little is known about these trajectories over time and their bidirectional influence. Child development is dynamic process where children influence their environment and the environment influences child development (Sameroff & Mackenzie, Reference Sameroff and Mackenzie2003; Sameroff, Reference Sameroff1975). Exploring only child or parent characteristics alone, without consideration of their broader interaction can result in misleading conclusions (Sameroff & Mackenzie, Reference Sameroff and Mackenzie2003). Transactional models propose that parent emotional distress can result in child EBPs and conversely, child EBPs can result in parental psychological distress. Thus the process of developmental psychopathology in children is influenced by parents and vice versa (Sameroff & Mackenzie, Reference Sameroff and Mackenzie2003). Emerging research shows support for this model in both typically developing children and in one study for children with developmental delays, specifically borderline to extremely low cognitive functioning (Neece et al., Reference Neece, Green and Baker2012). However, there are a lack of empirical studies exploring this transactional model due to the need for large longitudinal studies which are costly and take considerable time.
Thus, very few studies have explored these bidirectional relationships between parent and child emotional functioning in children with ASD or ADHD using longitudinal designs, and those that have generally use only a few time points. One study of children with ASD assessed at age 9 months, 3 years and 5 years, found maternal psychological distress, but not early child behaviour problems, predicted later child behaviour problems (Totsika et al., Reference Totsika, Hastings, Emerson, Lancaster, Berridge and Vagenas2013). They suggested the bidirectional influence was therefore not present in children with ASD. In ADHD, studies have focused on parent-child relationships rather than parental psychological distress (Lifford et al., Reference Lifford, Harold and Thapar2008, Reference Lifford, Harold and Thapar2009). To the authors knowledge, there have been no longitudinal studies exploring ASD and ADHD compared with ASD + ADHD, to understand a transactional model of mental health problems between parents and children. Such an exploration would provide important information regarding peak times of need for mental health intervention for parents and children and may indicate the priority for each. They would also seek to either validate or question whether transactional models of parent/child emotional health apply to children with neurodevelopmental disorders.
The Longitudinal Study of Australian Children (LSAC) recruited two population-representative cohorts of Australian children and has followed them from age 0 to 14 years in the Birth cohort, and from age 4 to 18 years in the Kinder cohort. Data has been collected every 2 years from 2003/04, with parents in the Birth cohort reporting if their child has ASD from age 6 and ADHD from age 4. This study will explore the Birth cohort given it has tracked parent mental health since children were babies (age under one year), thus exploring children from age 0 to 14 years. LSAC offers a unique opportunity to explore transactional models of child development in children with ASD and ADHD due to the longitudinal design. It provides a range of family, parent and child demographic measures and child characteristics including child temperament, cognitive and language ability, all factors which can influence both child and parent emotional health.
The aims of this study were to understand (a) whether there were differences in mother psychological distress and child EBPs between children with ASD, ADHD, ASD + ADHD and those without these disorders, (b) how mother and child mental health changed over time from child age 0 to 14 years in each group, and (c) whether there was a bidirectional relationship between early mother psychological distress and later child EBPs and vice versa, in mothers of children with combined ASD, ADHD, and ASD + ADHD.
Hypotheses were as follows. Firstly, it was predicted that mothers of children with ASD, ADHD, and ASD + ADHD would have significantly higher psychological distress than mothers of children without these conditions. As past studies suggest an additive effect of having ASD + ADHD, it was expected that mothers of children with ASD + ADHD would have more psychological distress than those with ASD or ADHD alone. Secondly it was expected that children with ASD, ADHD, and ASD + ADHD would have more EBPs over time than children without these disorders, with children with ASD + ADHD having the highest levels. It was expected that child EBPs would peak at around 10–12 years of age, but no hypotheses were made about mother psychological distress over time in these groups given a lack of prior research. Finally, a bidirectional relationship was hypothesised which would support the transactional model of child development, such that early mother psychological distress would influence later child EBPs, and vice versa, and this would be present in the combined group of children with ASD and or ADHD, and in children without.
Method
Study design
A secondary data analysis of already collected data from LSAC, a longitudinal Australian population representative cohort study, was conducted.
Participants
LSAC employs a cross-sequential design following two Australian population based cohorts of children. At the first wave children were aged 0–1 years (Birth cohort; n = 5107; born 2004) and 4–5 years (Kinder cohort; n = 4983; born 2000) during 2003/2004, and have been assessed every 2 years (Sanson et al., Reference Sanson, Nicholson, Ungerer, Zubrick, Wilson, Ainley, Berthelsen, Bittman, Broom, Harrison and Sawyer2002). At wave 8 in 2018 there were N = 3,127 responding in the Birth cohort (age 14–15 years) which will be the focus of this study.
The broader LSAC study was approved by the Australian Institute of Family Studies Ethics Committee. Parents/caregivers provided written informed consent. This current study is a secondary analysis of general release Wave 8 LSAC data. Approval for the current study was granted by the National Centre for Longitudinal Data and the Charles Sturt University Human Ethics Committee.
Measures
Mother-reported ASD and ADHD status
At each wave occurring every 2 years, during the study interviews primary caregiver were asked: ‘Does your child have any of these ongoing conditions?’. Parents could respond yes or no regarding whether their child had ‘Autism, Aspergers, or other autism spectrum’ from age 6 to 14 years, and ‘Attention Deficit Hyperactivity Disorder/Attention Deficit Disorder’ from age 4 to 14 years. Diagnosis was not verified by study researchers. In the current study, a parent report of their child having these diagnoses at any age was used to indicate ASD, ADHD, or ASD + ADHD if parents indicated yes to both questions at any age. Parents also reported on the age ASD was first diagnosed. This question was not asked of ADHD and instead age of first diagnosis was calculated based on child’s age at the first wave that parents indicated their child had ADHD.
Child mental health
Emotional and behavioural problems (EBPs) were assessed by the parent and teacher-reported SDQ (Goodman, Reference Goodman2001). The SDQ is a 25 item questionnaire with five subscales, each containing five items: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems and prosocial behaviour. Satisfactory reliability and validity has been demonstrated (Goodman, Reference Goodman2001). The total score was used in the current study and is the sum of all subscales except prosocial behaviour, and ranges from 0 to 40. Raw scores were used. Higher scores indicate more EBPs. The SDQ was collected from ages 4 to 14 years of age.
Parent psychological distress
This was assessed using the K6 psychological distress self-report scale (Kessler et al., Reference Kessler, Barker, Colpe, Epstein, Gfroerer, Hiripi, Howes, Normand, Manderscheid, Walters and Zaslavsky2003). This 6-item questionnaire uses a 5-point Likert scale ranging from ‘none of the time’, to ‘all the time’. The questions draw from depressive and anxiety symptomology. A total score was calculated from the six questions with higher scores indicating more psychological distress. Scores from child age 0 to 14 years were used.
Demographic variables
Demographic information included neighbourhood socioeconomic disadvantage which was measured using the Socio-Economic Indexes for Areas Disadvantage Index (SEIFA) which corresponds to the family’s postcode. Number of siblings in the family, geographic remoteness (dichotomised to very remote/remote or non-remote), whether English was the primary language spoken at home, primary caregiver education level, whether a family had one or two parents, and indigenous status were also recorded and used as covariates in analyses. These variables were included given their potential differences between children with ASD and or ADHD compared to those without, as found in prior studies (Canals et al., Reference Canals, Morales-Hidalgo, Jané and Domènech2018; Rai et al., Reference Rai, Lewis, Lundberg, Araya, Svensson, Dalman, Carpenter and Magnusson2012).
Child factors
The child’s language level was assessed by the short version of the Peabody Picture Vocabulary Test third edition (PPVT-III) (Dunn & Dunn, Reference Dunn and Dunn1997) at age 4, 6, and 8 years. The Matrix Reasoning subtest from the Wechsler Intelligence Scale for Children IV (WISC-IV) at 6, 8, and 10 years was used as a brief measure of child cognitive functioning and assesses non-verbal intelligence. Data from the youngest wave (age 4 PPVT and age 6 matrix reasoning) were used as covariates in analyses. Child temperament was assessed at ages 0 and 2 years using the shortened 12-item version of the Short Temperament Scale for Children (Prior et al., Reference Prior, Sanson, Smart and Oberklaid2000). This measures three dimensions of child temperament with four items per dimension: persistence (capacity to see tasks through to completion), reactivity (intensity and volatility of child), and introversion (reaction to new people and situations). Parents rated their child for each item on a six-point Likert scale (from 1 = almost never, to 6 = almost always). Temperament was combined into one variable by summing each of the three dimensions for entry into models, which provides an overall score as to indicate whether the child has an ‘easy’ or ‘difficult’ temperament.
Procedure
LSAC trained interviewers conducted face to face interviews with the primary caregiver at their home. Direct assessments of children and administration of parent surveys were also conducted at each LSAC wave. The primary caregiver was usually the mother and was consistent across the waves, except in a minority of cases (1.5%) which were excluded from analyses. Thus, maternal psychological distress was explored.
Statistical analysis
Survey methods were used where appropriate to ensure equal probability of participant selection into the sample, account for non-response and sample attrition and also the multi-stage, clustered sampling design (Soloff et al., Reference Soloff, Lawrence, Misson, Johnstone and Slater2006). Weights from the most recent wave 8 were used. These weights account for both geographic representation, to make the sample more similar to the Australian population, and to account for any loss to follow-up to make the sample more similar to the original participants. To remove the impact of missing data mean imputation by group was used for missing data at different waves.
Summary statistics described differences in demographic and clinical variables for the four groups (ASD, ADHD ASD + ADHD, no developmental diagnosis). Group differences were explored using Chi Square tests for categorical data, and linear regression for grouped data, with post hoc tests used if omnibus tests were significant. All analyses were conducted in Stata Version 15.0.
Aims 1 and 2
Generalised Estimating Equations were used to explore group differences and differences in trajectories for parent psychological distress and child EBPs grouped by children with ASD, ADHD, ASD + ADHD and those with no developmental diagnoses. Demographic and child factors indicated above were controlled for in these analyses. To assess group differences at each timepoint 95% confidence intervals were used. This analysis compares groups on parent psychological distress and child EBPs as well as differences in these slopes over time.
Aim 3
SEM using the STATA SEM command was used in a cross lagged linear model using maximum likelihood estimation. This was an exploratory analysis to understand whether the theorised bidirectional relationship between parent psychological distress and child EBPs was supported in children with or without ASD/ADHD. Covariance between pairs of variables (parent psychological distress and child EBPs) at the same timepoint were used. The model estimated the cross lagged paths between the mother and child. Parent psychological distress (K6) from child ages 0 to 14, child temperament at age 0 and 2 years and child EBPs measured using the SDQ from child age 4 to 14 were used. Two cross lagged models were run. The first for children without ASD/ADHD (n = 4,624) and the second for the combined group of children with ASD and/or ADHD (n = 409). Children with ASD and/or ADHD were combined into one group to ensure an adequate sample size for this analysis given the seven time points explored. Socio-economic status at the final wave was controlled for in analyses by calculating its effect on child EBP and parent psychological distress at age 14. Model fit was measured using the RMSEA, Based on past recommendations values less than .06 indicated good fit, values between .05 to .10 acceptable fit and values >.10 indicated poor fit (Browne & Cudeck, Reference Browne and Cudeck1992; MacCallum et al., Reference MacCallum, Browne and Sugawara1996).
Results
Demographic characteristics by group
The adjusted proportion of children with ASD only was 3.94%, ADHD only was 4.08%, and with ASD and ADHD was 2.31%. Of the children with ASD, the adjusted proportion of these who also had ADHD was 35.7%; and of children with ADHD the adjusted proportion of these with ASD was 36.5%. The adjusted mean age of diagnosis of ASD in children with ASD only was 6.7 years [95% CI 6.0–7.4] and in children with ASD + ADHD was 6.0 years [95% CI 5.0–6.9]. Age of diagnosis for ADHD only was 9.1 years [95% CI 8.4–9.8] and in children with ASD + ADHD 8.1 [95% CI 7.3–9.0].
Demographic and child characteristics for ASD only, ADHD only, ASD + ADHD and those without these diagnoses were compared using age 0 data, and age 4 data for child factors not collected at age 0, see Table 1. Children without these diagnoses and with ASD only were significantly older than children with ADHD + ADHD at baseline. Children without these diagnoses had higher SEIFA than children with ASD + ADHD. Children with ASD or ADHD only had higher proportions of English as the main language spoken at home than children without these diagnoses. Families of children with ASD only had fewer children in the home than families of children without these diagnoses or with ADHD. Children with ASD + ADHD were more likely to come from single parent families than children without these diagnoses. Children with diagnoses were more likely to be male than children without these diagnoses. Children with ADHD were less likely to be male than children with ASD. There were no group differences in geographical remoteness, proportion of Indigenous children, proportion of primary caregivers not completing high school, and child temperament relating to introversion and persistence.
Table 1. Differences in demographic and child factors between the groups
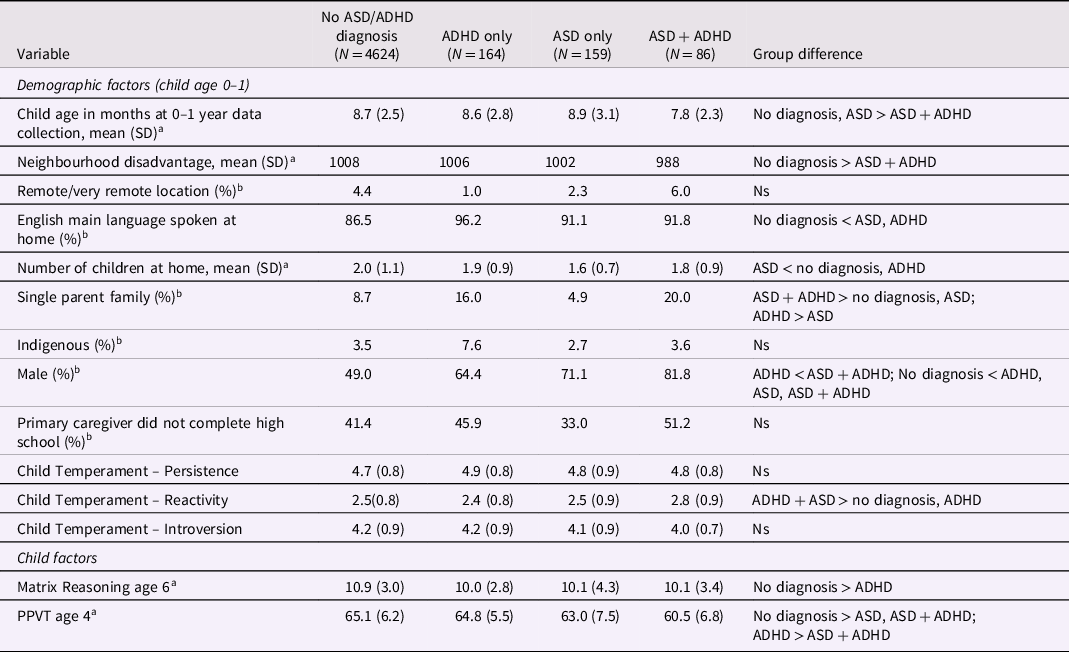
Note. All statistics are weighted and adjusted for LSAC sample design; PPVT = Peabody Picture Vocabulary test; Ns = not significant; ADHD = attention deficit hyperactivity disorder; ASD = Autism Spectrum Disorder; SD = standard deviation. aregression analysis used for statistical comparison; b χ 2 used for statistical comparison.
Child emotional and behavioural trajectories by group
Figure 1A shows child SDQ total scores over time by group with predicted slopes and Figure 1B shows child SDQ total scores over time with 95% confidence intervals. Results of the generalised estimating equation indicated significant differences between groups, over time and differences in slopes. Children without diagnoses had lower SDQ total scores over all ages than children with ASD (B = 4.95 [95% CI 4.17, 5.74], z = 12.39, p < .001), ADHD (B = 3.12 [95% CI 2.54, 3.80], z = 9.92, p < .001) or ADHD + ASD (B = 5.73 [95% CI 5.52, 6.96], z = 9.24, p < .001). Children with ADHD had lower SDQ scores also over all ages than children with ADHD + ASD. Children with ADHD + ASD had higher SDQ scores than children with ASD at age 6, 8, 12 and 14.
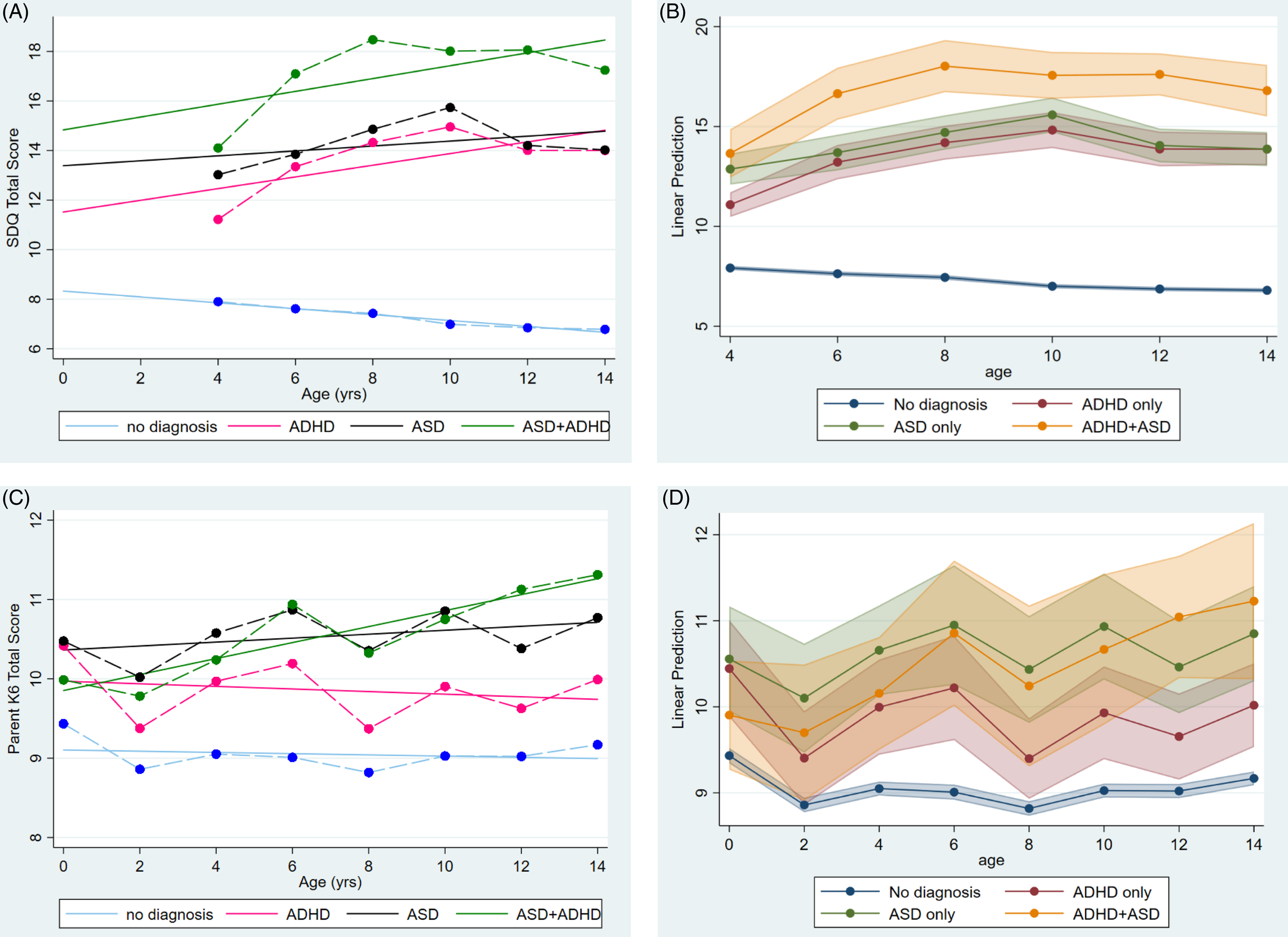
Figure 1. (A) Child emotional and behavioural problems (SDQ total score) from age 4 to 14 with slopes; (B) Child emotional and behaviour problems from age 4 to 14 with 95% CIs; (C) Mother psychological distress(K6) from child age 0 to 14 with slopes; (D) mother psychological distress from age 0 to 14 years with 95% CIs.
The peak of EBPs was at age 4 years in children without diagnoses and the slope was decreasing. In children with ASD + ADHD the peak was at age 8 with an increasing slope. The peak was later, at age 10, in children with ASD or ADHD, with both showing an increasing slope of EBPs.
Mother psychological distress trajectories by group
Figure 1C shows mother psychological distress scores over time by group and slopes, and Figure 1D shows the 95% confidence intervals. Overall, mothers of children without diagnoses had lower levels of psychological distress than mothers of children with ASD (B = 1.12 [95% CI 0.50, 1.74], z = 3.56, p < .001) or ADHD (B = 1.01 [95% CI 0.44, 1.55], z = 3.48, p = .001) but not ASD + ADHD (B = 0.47 [95% CI − 0.17, 1.11], z = 1.44, p = .150) although there were differences at particular ages. There was no difference in psychological distress at child age 0 for mothers of children with ASD + ADHD and children without diagnoses. Mothers of children with ASD and ADHD only had higher levels of psychological distress when their children were aged 0, than parents of children with ASD + ADHD and parents of children without diagnoses. At child age 2, mothers of children with ASD only had higher psychological distress than all other mothers. From age 4 years old, mothers of children with ASD, ADHD and ASD + ADHD had higher psychological distress than mothers of children with no diagnoses. At age 12, parents of children with ASD + ADHD had higher levels of psychological distress than mothers of children with ADHD only. Otherwise, mothers of children with ASD, ADHD, and ADHD + ASD had similar levels of psychological distress. The mother psychological distress in children without diagnoses and ADHD followed a declining trajectory; compared with an increasing trajectories of mother psychological distress in children with ASD (with or without ADHD).
The peak of psychological distress was at child age 0 for mothers of children without diagnoses and ADHD only, age 14 in mothers of children with ASD + ADHD, and age 6 in ASD only.
Exploration of bi-directional relationship between mother psychological distress and child emotional and behavioural problems
Figure 2 show the cross lagged fitted models of the bidirectional relationship between mother psychological distress and child EBPs for children with ASD/ADHD (Figure 2B) and those without (Figure 2A). Results are presented as standardised correlation coefficients with statistically significant associations indicated. The fit of the model was acceptable with RMSEA being under 0.10 for children without (RMSEA = .08) and children with ASD/ADHD (RMSEA = .09). Although, CFI and TLI were below levels usually indicating good fit (children without CFI = 0.86, TLI = 0.80; children with ASD/ADHD CFI = 0.84, TLI = 0.78),it is noted that arbitrary cut-offs have been criticised, particularly for continuous variables as used in the current study (Xia & Yang, Reference Xia and Yang2019). There were significant paths between mother psychological distress from child age 0 to 14 in children with and without ASD/ADHD. Child temperament showed a significant path from 0 to 2 years in children without diagnoses but not for children with ASD/ADHD. For child EBPs there were significant associations from the first measurement at child age 4 until 14 years in children with and without ASD/ADHD.
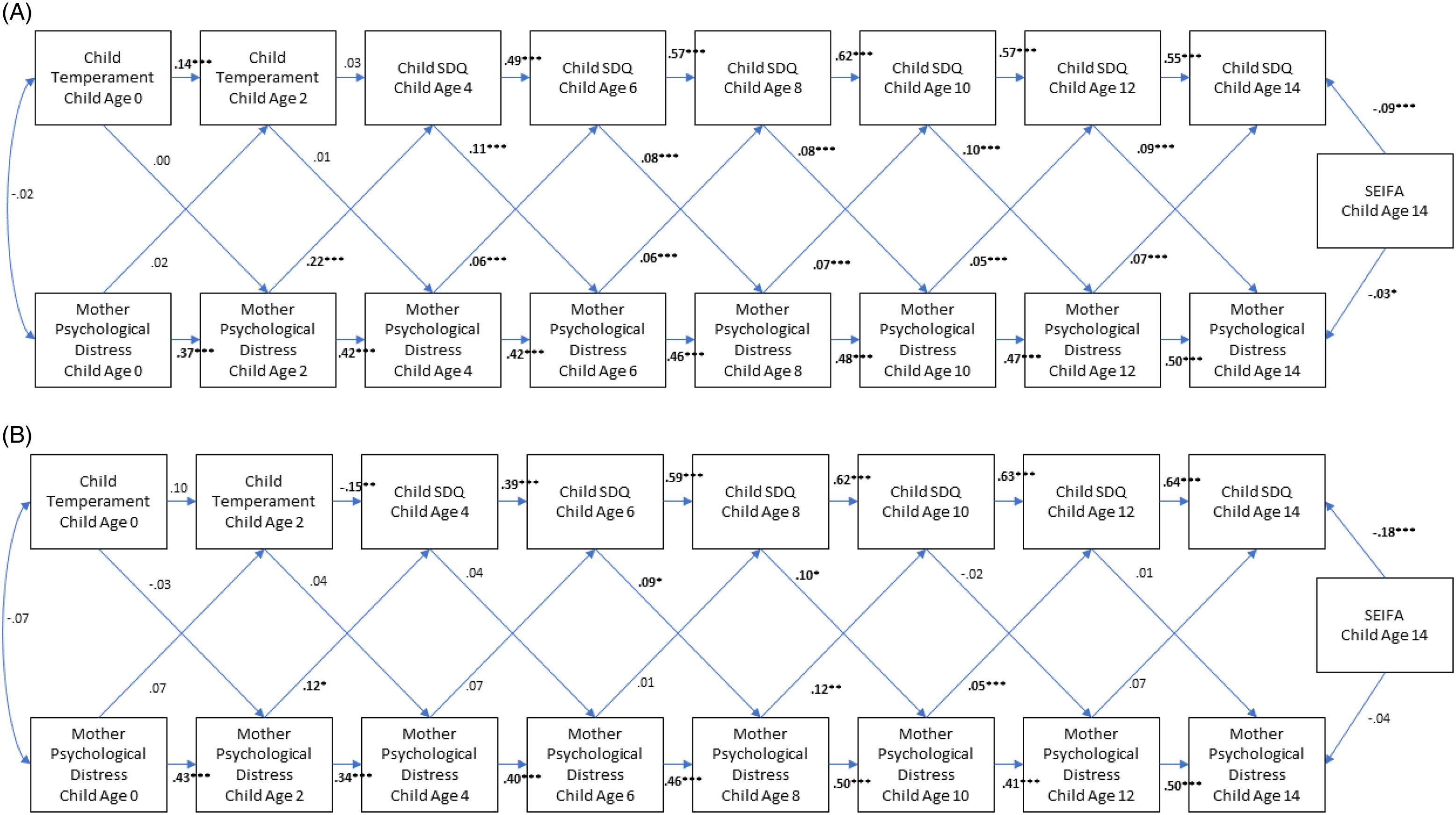
Figure 2. (A) Bidirectional cross lagged model of mother psychological distress and child EPBs in children without ASD/ADHD; (B) Bidirectional cross lagged model of mother psychological distress and child EPBs in children with ASD/ADHD. Note. SDQ = Strengths and Difficulties Questionnaire Total score; EBPs = Emotional and Behavioural Problems. ***p < .001; **p < .01; *p < .05.
Regarding cross lagged effects, for children without ASD/ADHD bidirectional relationships were consistently present from child age 4 until 14 years. Mother psychological distress predicted child EBPs 2 years later and vice versa consistently throughout this period. Mother psychological distress at age 2 also predicted child SDQ score at age 4; but child temperament at 2 years did not predict mother psychological distress at age 4.
Cross lagged effects were far fewer in children with ASD/ADHD. Mother psychological distress predicted child EBPs 2 years later only at child age 2, 8 and 10 years. Child EBPs predicted mother psychological distress at child ages 6 and 8 only. Eight years of age was the only time when there was bidirectional prediction between mother and child emotional health for 2 years later.
Discussion
There are few studies exploring the longitudinal emotional and behavioural impacts to children and their parent from having ASD, ADHD or both over time. This study aimed to understand trajectories of child EBPs and mother psychological distress in children with ASD only, ADHD only, and ASD + ADHD. It also sought to understand whether there was a bidirectional relationship between mother psychological distress and child EBPs as predicted by transactional models of child development. As expected, children with ASD and/or ADHD diagnoses had higher emotional and behavioural problems than children without these diagnoses, and their mothers had higher levels of psychological distress across some time points, but with differing trajectories.
Compared to children with ASD or ADHD alone, children with ASD + ADHD had more emotional and behavioural problems from age 6 to 14 and an earlier peak at age 8 compared to age 10 in the other groups. Children with ASD + ADHD had a younger age of ASD diagnosis than children with ASD alone. Their mothers showed increasing psychological distress over time, similar to mothers of children with ASD, whereas mothers of children with ADHD tended to have reducing psychological distress over time. These findings are consistent with children with the combined disorder having more severe symptoms exhibited earlier in development.
The bidirectional relationship between mother and child mental health, where early parent psychological distress predicted later child EBPs and early child EBPs predicted later mother psychological distress, was less pronounced in the combined group of children with ASD/ADHD. This suggests different mechanisms may be occurring for children with ASD/ADHD in the development of EBPs and the transactional model of mother-child emotional health may be less applicable for children with neurodevelopmental disorders.
Mother psychological distress
Over time mothers of children with ASD, ADHD and ASD + ADHD had significantly higher psychological distress than mothers of children without these diagnoses, specifically from age 4 years. At child age 0 mothers of children without these diagnosis and mothers of children with later diagnoses of ADHD had similar levels of psychological distress, which was below that of mothers of children with ASD, with or without ADHD. At age 2, mothers of children later diagnosed with ADHD or ASD + ADHD had similar levels of psychological distress to mothers of children with no diagnoses. Mothers of children with ASD at all ages had higher psychological distress than mothers of children with without these diagnoses. These findings from child age 4 years mirror extensive prior research showing higher parental mental health issues in parents of children with ASD and/or ADHD relative to parents without children with these diagnoses (Karst & Van Hecke, Reference Karst and Van Hecke2012; Tarabek, Reference Tarabek2011; Theule et al., Reference Theule, Wiener, Tannock and Jenkins2013; Van Steijn et al., Reference Van Steijn, Oerlemans, Van Aken, Buitelaar and Rommelse2014; Wesseldijk et al., Reference Wesseldijk, Dieleman, van Steensel, Bartels, Hudziak, Lindauer, Bögels and Middeldorp2018).
We also predicted mothers of children with ASD + ADHD would have more psychological distress than those with ASD or ADHD alone due to the additive effects of having the symptoms and subsequent functional impact of both disorders. This hypothesis was partially supported. While the psychological distress of mothers with ASD + ADHD showed the steepest increasing slope and highest levels at child age 12 and 14 years, there was no statistical difference with mothers of children with ASD or ADHD (except at age 12). However, mothers of children with ASD (with or without ADHD) had higher psychological distress, although not statistically significant, than mothers of children with ADHD at all ages from 2 years. The wide confidence intervals due to the smaller sample size in ASD + ADHD may have contributed to a lack of statistical differences being found. These findings are generally consistent with Van Steijn et al. (Reference Van Steijn, Oerlemans, Van Aken, Buitelaar and Rommelse2014) who found higher levels of stress in parents of children with ASD + ADHD and parent depression in those with ASD and ASD + ADHD, than ADHD alone.
These findings show that mothers of children with ASD (with or without ADHD) already had higher psychological distress in the first year of their children’s life; well before their children were formally diagnosed with ASD. This is consistent with past research showing more psychiatric disorders, including depression, in parents of children with ASD (Daniels et al., Reference Daniels, Forssen, Hultman, Cnattingius, Savitz, Feychting and Sparen2008). However, we cannot exclude the possibility that in the first year of life the babies who were later diagnosed with ASD were more challenging to parents. Challenges could have included increased irritability, feeding and sleep problems. This is partially supported by parents of children with ASD + ADHD in the current study reporting higher levels of child reactivity in their infants at age 0 than children with no diagnoses, or ADHD. Children with ASD only had similar levels of reactivity to children with ASD + ADHD. Otherwise, there were no differences in child temperament relating to persistence and introversion at this age.
We made no hypotheses about the peak of mother psychological distress over time in these groups given a lack of prior research. For children without diagnoses, mother psychological distress was greatest at child age 0. For parents of children with ASD + ADHD mother psychological distress increased over time, with the most recent age of 14 having the highest level of distress. For ASD only there were peaks at 6 and 10 years; with another peak at age 14 years. Notably in ASD the mean age of diagnosis was 6 years and ADHD only, 9 years. Obtaining a diagnosis could potentially relate to these peaks given past literature about the significant stress for many parents during this process (Bonis, Reference Bonis2016). For children with ASD (with or without ADHD) mother psychological distress increased over time. For children with no diagnoses or ADHD, the trajectory of mother psychological distress was either flat or slightly decreasing. The increase in mother psychological distress at age 14 for children with ASD (with or without ADHD) could be due to various factors. We speculate these may include navigating the transition to high school and the second wave of executive dysfunction that occurs with the onset of puberty in ASD (Cadman et al., Reference Cadman, Eklund, Howley, Hayward, Clarke, Findon, Xenitidis, Murphy, Asherson and Glaser2012; Nuske et al., Reference Nuske, McGhee Hassrick, Bronstein, Hauptman, Aponte, Levato, Stahmer, Mandell, Mundy, Kasari and Smith2019; Ozonoff & McEvoy, Reference Ozonoff and McEvoy1994). Exploring the ongoing trajectory of parent psychological distress as children continue through adolescence and into early adulthood will be important future research to understand whether age 14 will be a peak time for psychological distress for parents or whether there will be a continuing upward trajectory.
Child emotional and behavioural problems
It was hypothesised that children with ASD, ADHD and ASD + ADHD would have higher emotional and behavioural problems over time than children without these disorders, with children with ASD + ADHD having the highest levels. Overall children with ASD and or ADHD had higher EBPs at all ages than children without these diagnoses, with these levels of EBPs present for many children well before they were diagnosed. That children with ASD + ADHD had higher levels of EBPs was supported from age 6 to 14 years and suggests that the combination of ASD + ADHD does result in a cumulative effect. This is consistent with past studies showing children with ASD + ADHD have more behaviour problems than children with ASD or ADHD alone (Gargaro et al., Reference Gargaro, May, Tonge, Sheppard, Bradshaw and Rinehart2014).
It was expected that child emotional and behavioural problems would peak at around 10–12 years of age based on the two prior cross-sectional and longitudinal studies (Becker et al., Reference Becker, Steinhausen, Baldursson, Dalsgaard, Lorenzo, Ralston, Döpfner and Rothenberger2006; Russell et al., Reference Russell, Golding, Norwich, Emond, Ford and Steer2012). This finding was partially supported. For children without these diagnoses, there was a gradual linear decline in emotional and behavioural problems from age 4 to 14 years. In contrast the clinical groups showed an inverted U profile, with a peak in child behavioural problems at age 8 years in ASD + ADHD, and a slightly later peak at 10 years in children with ASD or ADHD alone. Given the lack of longitudinal studies in this area these findings are novel and need replication in other cohorts.
Bidirectional relationship between mother psychological distress and child emotional/behavioural problems
Finally, a bidirectional relationship was hypothesised, such that mother psychological distress would influence later child EPBs, and vice versa. Findings from the current study indicate a different relationship in children with and without ASD/ADHD. There were consistent bidirectional relationships from age 4 to 14 in children without these diagnoses, such that child EBPs and parent distress predicted the other 2 years later, consistently until age 14. Thus, in children without ASD/ADHD the bidirectional relationship between mother distress and child EBPs supported the transactional model of child and parent emotional problems (Sameroff & Mackenzie, Reference Sameroff and Mackenzie2003; Sameroff, Reference Sameroff1975).
In contrast, in children with ASD/ADHD a bidirectional relationship was only present at child age 8 with cross lagged effects predicting outcomes at child age 10 years. Only two prior studies have explored this bidirectional relationship in children with developmental disorders. One suggested that the bidirectional relationships was not present in children with ASD based on assessments at age 9 months, 3 years and 5 years (Totsika et al., Reference Totsika, Hastings, Emerson, Lancaster, Berridge and Vagenas2013). Our findings are consistent with this. They found mother psychological distress at 3 years predicted child EBPs at age 5. We found mother psychological stress at 2 years predicted child EBPs at 4 years consistent with their finding but with a 1-year age difference. The other study combined children with borderline or extremely low cognitive functioning assessed at 3–9 years with children with normal cognitive functioning into the one cross lagged model. Intellectual ability was not correlated with time one variables, hence the authors concluded the relationship was similar regardless of cognitive functioning (Neece et al., Reference Neece, Green and Baker2012). They found that mother’s stress at child age 3 and 4 and 6 and 7 years predicted child EBPs one year later; and child EBPs at age 4, 6 and 7 years predicted mother stress one year later. Child age 7 was the only time there was a bidirectional relationship between mother stress and child EBPs both predicting the other at child age 8 years. The only time a concurrent bidirectional relationship was found in children with ASD/ADHD in the present study was at child age 8 predicting levels at child age 10. It appears that in children with ASD/ADHD that bidirectional relationships are fewer and occur later, primarily between the ages of 6 and 10 years. These findings have significant clinical implications given the average age for diagnoses in our study, ASD (6 years) and ADHD (9.1 years). Additional support is warranted for parents and children at these times to attempt to minimise any bidirectional impacts.
That bidirectional effects are not present earlier in children with ASD/ADHD may be due to several factors. For example, the ‘wear and tear’ model might apply where exposure is needed over a long time to accumulate any effects. This may be salient given the peak of parent psychological distress was at age 14 compared with parent/child peaks of EBPs at age 8–10 years. While multiple factors may account for this mismatched peak, the wear and tear model could explain this accumulation of psychological distress in mothers versus the inverted U shape of child EBPs. Also, mother’s psychological distress and child EBPs were already elevated early in life for children with ASD/ADHD. It may have resulted in ceiling type effects such that child EBPs would not further influence increases in mother psychological distress, and vice versa.
Overall, it is perhaps not surprising that evidence for a bidirectional relationship was weaker in children with ASD/ADHD. ASD and ADHD are neurodevelopmental disorders caused mostly by biological rather than social factors. The heritability of ASD and ADHD disorders is around 80 to 90% based on twin studies and genetic factors explain most of the risk for ASD/ADHD (Larsson et al., Reference Larsson, Chang, D'Onofrio and Lichtenstein2014; Sandin et al., Reference Sandin, Lichtenstein, Kuja-Halkola, Hultman, Larsson and Reichenberg2017). As such, the transactional model where parent emotional distress can result in child EBPs may be limited when mostly biological causes of child EBPs are present. This also applies to parents such that their own genetic and biological factors could be causing psychological distress, given more mental health problems identified in parents of children with ASD/ADHD before having children. While the current model went beyond exploring child factors to understand psychopathology, and included parent psychological distress, the model did not capture other factors relating to the social context of the child and parent other than socioeconomic-status. It is likely that complex factors are at play, suggesting that transactional models of child development may be different for children with neurodevelopmental disorders.
Limitations and future research
There was no measure of ASD symptoms and diagnoses of ASD and ADHD were not validated by researchers or clinicians, and are solely based on parent report. We have explored some of these issues in our prior work (May et al., Reference May, Brignell and Williams2021) but also note that parent report of a diagnosis is usually accurate (Daniels et al., Reference Daniels, Rosenberg, Anderson, Law, Marvin and Law2012). Verifying diagnoses would be important future work, however, may not be feasible in these types of large longitudinal studies. If there was non-systematic under- or over-reporting of diagnosis of these conditions by parents, it would likely result in a tendency towards null-findings. It is also important to note that ADHD was only able to be dually diagnosed with autism from 2013 using the DSM-5 (American Psychiatric Association, 2000, 2013). This may have resulted in some children with ASD who had ADHD not being diagnosed with both disorders in the present study that commenced in 2004. Thus, it is possible that some of the children in the ASD only group also had ADHD. However, this would not have impacted on the bidirectional findings given the groups were combined for this analysis.
The SDQ used as a measure of child EBPs was only available from 4 years of age. We used child temperament at child age 0 and age 2 instead. The cross lagged model showed that child temperament at age 2 only predicted SDQ score at age 4 for the children with ASD/ADHD but not in children without these diagnoses, and so may have been measuring different constructs than child EPBs. However, given rapid changes in development from infancy to childhood there is not a measure that could be consistently used throughout this period to assess EBPs.
The bidirectional model fit was just at acceptable levels. As this was an exploratory study we aimed to understand whether a cross lagged model was present. Future research could explore other models which might show better fits, such as exploring four yearly rather than two yearly connections and including additional factors, such as parenting style, that could be a mediating factor between parent mental health and child EBPs. The measures explored here, parent mental health and child EBPs, have indirect effects on each other. Exploring the mechanisms by which parent anxiety/depression then impacts on their child resulting in EBPs and vice versa will be important. This could include parenting style and behaviours, including the ability to emotionally regulate. Exploring further environmental factors such as those relating to the school environment, family and social supports are also likely to be important factors in any transactional model. It also is also possible that intervention received by children with ASD/ADHD or their parents may have reduced any bidirectional influences. Empirically assessing these models using robust statistical techniques when so many factors are involved, in low prevalence developmental disorders, is a challenge for future research (Sameroff & Mackenzie, Reference Sameroff and Mackenzie2003).
The ASD/ADHD groups were combined to explore bidirectional relationships. It is important to note there may be group differences in how parental distress impacts on parenting behaviour. For example, a past study showed parental depression symptoms did not impact on parenting behaviours in parents of children with ASD, but they did for parents of children who were anxious (Ventola et al., Reference Ventola, Lei, Paisley, Lebowitz and Silverman2017). Exploring larger groups to enable exploration of ASD and ADHD separately will enable this type of relationship to be explored.
This study has numerous strengths. It utilised a population derived sample representative of the Australian general population of children with ASD/ADHD rather than clinically derived groups, which often have more severe symptoms and comorbidities which necessitated clinical attention. The longitudinal study is the only appropriate design to understand bidirectional relationships and this study utilised two yearly timepoints over 14 years of child development from the first year of life (Sameroff & Mackenzie, Reference Sameroff and Mackenzie2003). This study is the first to examine children with ASD/ADHD relative to ASD and ADHD only, over time and also systematically explore bidirectional relationships between parent and child emotional health. Thus, despite the noted limitations this study has provided important insights into the development of psychopathology and parent/child transactional models for children with ASD/ADHD.
Clinical implications
This longitudinal research has highlighted key times where EBPs may be particularly elevated in children with ASD/ADHD and these could be suitable times to plan intervention. The peak of EBPs is earlier for children with ASD + ADHD at around 8 years of age, compared with around 10 years of age for children with ASD or ADHD alone. Mothers of children with ASD + ADHD, ASD and ADHD alone are likely to experience peak psychological distress at around 6 years of age; with elevations for children with ASD when they start adolescence at around 12–14 years. For mothers of children with ADHD peaks are also present in the first year of their child’s life. For children with ASD/ADHD, mother’s psychological distress at child age 2, 8 and 10 has a significant later impact on their child’s EBPs. Child EBPs at age 6 and 8 has lagged effects on mother psychological distress.
Thus, 6 years of age is a critical time for parent mental health and child age 8–10 for child EBPs. Intervention for parents at this point may reduce exacerbation of later child behaviours problems. This links with age of diagnosis of ASD (6 years) highlights the importance of parent intervention programs which address both parent mental health and managing child EBPs at the time of diagnosis. Parent and child intervention programs addressing the management of both ASD and ADHD symptoms should also be considered given additive effects of increased child EBPs and high comorbidity, with at least a third of children with ASD having ADHD and vice versa.
For mothers of children with ADHD only, the average age of diagnosis means parents may not be identified as at risk of mental health problems by health professionals earlier in their child’s life. Mother mental health in children with ADHD only was lower than for mothers of children with ASD, but still elevated relative to children without diagnoses. Ensuring timely identification of ADHD in children is important given children with ADHD had significantly more EBPs from age 4 yet the average age of diagnosis was 9 years old. Focusing on child difficulties rather than diagnoses may result in the support sooner access to support. Increased awareness of health professionals, educators and the general public regarding ADHD is needed given the late average age of diagnosis despite high levels of emotional problems in mothers and their children from child age 4 years.
While there are many parenting behavioural skills programs for children with ASD/ADHD (Tarver et al., Reference Tarver, Palmer, Webb, Scott, Slonims, Simonoff and Charman2019) there are fewer programs targeting parent mental health (Da Paz & Wallander, Reference Da Paz and Wallander2017). Learning skills to better manage child behaviour results in reductions in stress in these programs. However, the high level of emotional distress already present in the child’s first year of life in parents of children with later diagnosed ASD/ADHD suggests that mental health issues are not only attributable to being a parent, and may require further intervention beyond parent training. It is particularly noteworthy that interventions that improve child EBPs may not result in later improvement in parent psychological health and vice versa for children with ASD/ADHD given the few bidirectional relationships found. Interventions for both the parent and the child will likely be necessary where there is evidence of efficacy.
Conclusion
This longitudinal research and approach to analyses has provided important new information about the timing and trajectories of parent psychological distress and child EBPs in children with ASD and ADHD. It has also presented novel findings in detailing the bidirectional relationships between mother mental health and child EBPs in children with ASD and ADHD over the first 14 years of child development. That bidirectional relationships were fewer in children with ASD/ADHD than in children without these diagnoses provides important insights into the transactional model of child development. Neurodevelopmental disorders may introduce factors related to underlying biological and other causes which reduce the strength of transactional models of child development between parent psychological distress and child EBPs.
Acknowledgements
This article uses confidential unit record files from the LSAC survey. The LSAC was initiated and funded by the Commonwealth Department of Families, Housing, Community Services and Indigenous Affairs and was managed by the Australian Institute of Family Studies. The findings and views reported in this article are those of the authors and should not be attributed to either the Commonwealth Department of Families, Housing, Community Services and Indigenous Affairs, or the Australian Institute of Family Studies.
Funding statement
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.






