Nutrition is an important and modifiable determinant of non-communicable chronic diseases. Cumulative epidemiological evidence shows that a diet rich in fibre is associated with decreased risk of CVD, certain types of cancer and type 2 diabetes, as well as better weight management and glucose control(Reference Lindstrom, Peltonen, Eriksson, Louheranta, Fogelholm, Uusitupa and Tuomilehto1–Reference Bhargava4). In pregnancy, during which excessive weight gain is currently common(Reference Nucci, Schmidt, Duncan, Fuchs, Fleck and Santos Britto5), additional benefits are a lower risk of pre-eclampsia(Reference Frederick, Williams, Dashow, Kestin, Zhang and Leisenring6, Reference Qiu, Coughlin, Frederick, Sorensen and Williams7), abnormal glucose tolerance(Reference Tovar, Must, Bermudez, Hyatt and Chasan-Taber8) and constipation(Reference Jewell and Young9, Reference Anderson and Whichelow10). A recent study also suggests an attenuation of pregnancy-associated dyslipidaemia by dietary fibre(Reference Qiu, Coughlin, Frederick, Sorensen and Williams7).
Healthy eating habits of mothers also have importance beyond their own health because pregnancy is a critical period in the life of the newborn(Reference Barker11). Additionally, mothers provide a role model for the eating patterns of the whole family(Reference Symon and Wrieden12) and the mother’s decisions about food are often made for the entire family. Since pregnancy represents a window for educating women about the benefits of healthy diet and lifestyle(Reference Olson13), health professionals and in particular dietitians could use this period to encourage women to make lasting changes in their habits in order to improve not only pregnancy outcomes but also to reduce future chronic disease.
In Brazil, the Ministry of Health publication Nutritional Guidelines for Brazilians (2006) presents nutritional recommendations aiming to maintain healthy nutritional habits and prevent chronic diseases in adults(14). This guide recommends a daily consumption of at least 25 g of dietary fibre, 3 servings of fruit and 3 servings of vegetables. During pregnancy, the recommendation for fibre intake, consistent with US recommendations, increases to 28 g daily(15).
Several studies in Brazil(Reference Barros, Pereira, Gama and Leal16–Reference Azevedo and Sampaio18) and other countries(Reference Olson13, Reference Giddens, Krug, Tsang, Guo, Miodovnik and Prada19–Reference Irles Rocamora, Iglesias Bravo, Aviles, Bernal, de Valle Galindo, Moriones, Maetzu and Mingo24) describe the nutritional intake of pregnant women. Many of them studied specific populations (e.g. overweight and teenage women). To our knowledge, none of these studies evaluated dietary fibre intake during pregnancy in Brazil, a nation with a culinary culture considered to be based on fibre-rich foods, especially beans and fruits. Fruits and vegetables are important markers of a healthy diet for their high content of fibre, which contributes to satiety and displacement of higher energy-dense foods. Whole-grain foods are a privileged source of fibre for their phytochemical and antioxidant content compared with refined grains. Fibre intake from whole grains has been inversely associated with chronic disease and mortality(Reference Jacobs, Meyer, Kushi and Folsom3, Reference Jacobs, Pereira, Meyer and Kushi25).
The aim of the present study was to assess, both quantitatively and qualitatively, the dietary fibre intake and factors associated with this intake in pregnant women receiving prenatal care in general practices in southern Brazil.
Method
Design and setting
ECCAGE – the Study of Food Intake and Eating Behaviour in Pregnancy – is a cohort study carried out in ten general public practices in Porto Alegre and eight general public practices in Bento Gonçalves, two cities in Rio Grande do Sul. Results presented herein pertain to the baseline data of ECCAGE. The study was approved by the ethics committee of the Federal University of Rio Grande do Sul and the committee responsible for the general practices in both cities. Written informed consent was obtained prior to all interviews.
Subjects
From June 2006 to April 2007, a total of 780 consecutive pregnant women between their 16th and 36th gestational weeks, receiving prenatal care in selected general practices covered by the study, were invited to participate during a routine prenatal care consultation. From these women, fifty-nine (7·5 %) refused to participate and nine (1·1 %) interrupted the interview prior to completion, resulting in a total of 712 pregnant women interviewed. Interviews were conducted before or after the clinical consultation; the principal reason given for refusal was lack of time to participate.
For the present analysis, 105 (14·7 %) women were excluded because their reported daily energy intake fell outside the usually accepted pregnancy range of 3347 kJ (800 kcal) to 20 083 kJ (4800 kcal), based on the Institute of Medicine (IOM)(Reference Trumbo, Schlicker, Yates and Poos26) recommendations, as applied in previous studies(Reference George, Hanss-Nuss, Milani and Freeland-Graves22, Reference Watts, Rockett, Baer, Leppert and Colditz27). Additionally, twenty-nine subjects (4·7 %) were excluded for reporting a daily intake of fruit and vegetables greater than 16 servings(Reference Mai, Flood, Peters, Lacey, Schairer and Schatzkin28), leaving 578 pregnant women for analysis.
Data collection
Interviews were conducted by trained interviewers. Weight and height were measured according to a standardized protocol and nutritional categories classified according to the IOM criteria(29). Data on sociodemographic variables were collected through a standardized questionnaire, with questions about age, marital status, years in school, family income, health-related behaviours such as tobacco and alcoholic beverage use during pregnancy, nutritional status before pregnancy according to self-reported BMI(29), receipt of nutritional guidance, and number of meals consumed daily.
Data on food intake were collected through an 88-item FFQ, derived from a previously validated questionnaire(Reference Sichieri and Everhart30) and validated for this population(Reference Giacomello, Schmidt, Nunes, Duncan, Soares, Manzolli and Camey31). Pearson correlation coefficients obtained in the validation study of the FFQ against a 24 h food recall were 0·27 for energy and 0·42 for fibre intake. The questionnaire provided standard servings of each food item to assess the amount consumed during pregnancy. The subjects reported the number of servings and frequency of intake for each food item listed. This frequency was categorized as >3 times daily, 2 or 3 times daily, once daily, 5 or 6 times weekly, 2 to 4 times weekly, once weekly, 1 to 3 times monthly, and never or hardly ever.
Analysis of food consumption data
The estimated consumption of energy, fibre and servings of fruit and vegetables reported in the questionnaire was calculated as:
For these calculations, the following weights were assigned for the frequency of food consumption categories: ‘>3 times daily’ = 3; ‘2 or 3 times daily’ = 2; ‘once daily’ = 1; ‘5 or 6 times weekly’ = 0·79; ‘2 to 4 times weekly’ = 0·43; ‘once weekly’ = 0·14; ‘1 to 3 times monthly’ = 0·07; and ‘never/hardly ever’ = 0.
A nutrient database for different foods was constructed using two main Brazilian references(Reference Philippi32, 33) and, when not listed, we used the information provided in food labels. Total dietary fibre in these references was determined using the Association of Analytical Communities (AOAC) methods(Reference Cho, Devries and Prosky34, Reference Li and Cardozo35).
Assessment of recommended food intake
To evaluate the fibre intake of the subjects, the Adequate Intake for fibre intake in pregnancy as defined by the US Food and Nutrition Board, i.e. 28 g/d, was used(15). To compare daily intake of fruit and vegetable servings with those currently recommended in Brazil, the servings listed in the questionnaire were converted to equivalents of the standard servings of the Nutritional Guidelines for Brazilians: at least 3 servings of fruit – 1 serving equals 130 g of a food item in the group and contains 293 kJ (70 kcal), fruit juices not included; and 3 servings of vegetables – 1 serving equals 60 g of a food item in the group and contains 63 kJ (15 kcal) daily(14). Consistent with most guidelines, the Brazilian recommendation is that cereal intake should be primarily whole-grain cereal(14). Therefore, a qualitative analysis of the fibre intake was performed to identify the percentage contribution of fibre from different food groups compared with the total fibre intake. The sources of dietary fibre were divided into cereals (refined and whole-grain), fruit, vegetables and legumes.
Statistical analysis
The percentage of pregnant women not meeting the recommendation was calculated. These and other descriptive analyses as well as those based on contingency tables were performed using the SPSS statistical software package version 13·0 (SPSS Inc., Chicago, IL, USA). The results are presented as means and standard deviations. The association between not meeting the recommended fibre intake and various factors was estimated adjusting for potential confounders with Poisson regression analysis using the STATA statistical software package version 9·0 (StataCorp, College Station, TX, USA). Variables with P values lower than 0·2 in bivariate analyses were entered in multivariable modelling. Statistical significance was established at the two-sided 0·05 level.
Results
The mean (sd) energy intake was 11 615 (3724) kJ/d (2776 (890) kcal/d). Mean daily intake of total dietary fibre was 30·2 (13·4) g. A total of 290 (50·2 %) women did not meet the recommendation for fibre intake.
As seen in the crude analyses of Table 1, not achieving the recommended fibre intake was associated with alcoholic beverage consumption (P = 0·01); eating less frequently (P < 0·001); not receiving nutritional guidance (P = 0·02); and having a higher pre-gestational BMI (P = 0·04). The distribution of the variables of Table 1 was similar between those included and excluded from the sample (data not shown).
Table 1 Sociodemographic characteristics, lifestyle habits and nutritional counselling of 578 pregnant women attending general medical practices in southern Brazil, 2006–2007
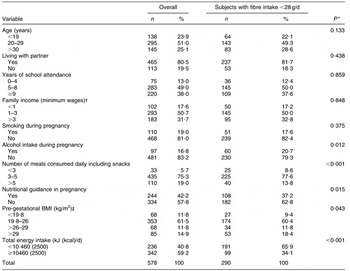
*Pearson χ 2 test comparing those who met v. did not meet recommendations.
†Minimum wage in Brazil in 2006 = US$ 175·00/month.
‡According to the Institute of Medicine(29); n 574 due to missing data on pre-gestational body weight.
Figure 1 illustrates the contribution of different food groups as sources of fibre. Most of the fibre intake came from the cereal group (10.5 g; 35 % of the total), but whole-grain consumption represented only 1 % of this group intake. Approximately one-third of dietary fibre was supplied by the fruit group (10 g; 34 %), followed by the legume group (6 g; 20 %) and the vegetable group (3.5 g; 11 %). Comparing the reported intake with the Nutritional Guidelines for Brazilians(14), we identified that 213 (37 %; 95 % CI 33, 41) pregnant women failed to meet the recommended fruit intake and 167 (29 %; 95 % CI 25, 33) failed to meet the recommended vegetable intake.
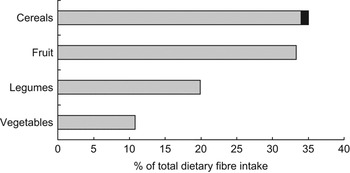
Fig. 1 Contribution of different food groups (█, whole-grain cereal) as sources of dietary fibre among 578 pregnant women attending general medical practices in southern Brazil, 2006–2007
Table 2 explores the magnitude of the associations between sociodemographic and behavioural independent variables and not meeting the recommended fibre intake. Crude prevalence ratios are shown for variables presenting a P value below 0·2. The multivariable model shows that the prevalence of not meeting the recommended fibre intake, adjusted for age, total energy intake, pre-gestational BMI and nutritional counselling, was 29 % higher in those consuming alcoholic beverages during pregnancy (P = 0·001); and, once adjusted for the same variables and alcohol consumption, 22 % higher in those not receiving nutritional guidance (P = 0·008).
Table 2 Factors associated with not meeting the recommended fibre intake in 578 pregnant women attending general medical practices in southern Brazil, 2006–2007
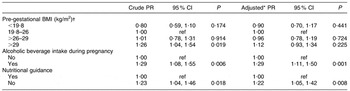
PR, prevalence ratio; ref, referent category.
*Through Poisson regression analysis adjusted for age, total energy intake and the other variables in the table.
†According to the Institute of Medicine(29); n 574 due to missing data on pre-gestational body weight.
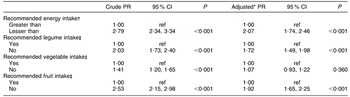
Table 3 explores the magnitude of similar associations with principal dietary factors. The adjusted prevalence ratio was 2·07 (95 % CI 1·74, 2·46) for women not meeting the recommended energy intake; 1·72 (95 % CI 1·49, 1·98) for women not meeting the recommended legume intake; and 1·92 (95 % CI 1·65, 2·25) for women not meeting the recommended fruit intake. In the multivariable model, after adjusting for all of these factors, meeting the recommended vegetable intake was no longer statistically significant.
Table 3 Dietary factors associated with not meeting the recommended fibre intake in 578 pregnant women attending general medical practices in southern Brazil, 2006–2007
To assess the degree to which exclusion of women with outlying quantities of intake altered the percentage of women not meeting recommended daily total fibre intake, we reanalysed this percentage. Without these exclusions, 294 (41·3 %) women did not reach the recommended intake.
Discussion
In the present study of pregnant women receiving prenatal care in general public medical practices in southern Brazil, we found a mean daily dietary fibre intake of 30·2 g/d, above the minimal recommended value. However, the intake of 50 % of the sample was below this level, indicating the need for nutritional guidance. Moreover, the principal source of fibre was refined cereals.
The use of Dietary Reference Intakes to analyse individual intake(Reference Beaton36, Reference Murphy, Guenther and Kretsch37) has been questioned. These quantitative estimates of nutrient intake, published by the Food and Nutrition Board since 1998, were established for nutritional assessment and planning of groups of individuals. For instance, Murphy and colleagues(Reference Murphy, Guenther and Kretsch37), in their recommendations regarding the use of Dietary Reference Intakes to assess adequacy of intake, state that comparison of mean intake of nutrients with an established value of Adequate Intake between groups is appropriate, and that a mean intake above the recommended value indicates a low prevalence of inadequacy.
However, physiological mechanisms(Reference Heaton38) – displacing available nutrients from the diet; requiring chewing, which slows down intake and promotes satiety; and reducing the absorptive efficiency of the small intestine – by which gram quantities of dietary fibre are thought to protect against disease are quite different from those by which microgram quantities of diverse micronutrients such as vitamins and trace minerals exert their beneficial effects. As such, while assessment of nutritional adequacy in groups by mean values may be the most appropriate approach for micronutrients such as vitamins, we believe that they are not for fibre.
Therefore we believe that our finding of 50 % of women with intake below the cut point indicates an important prevalence of inadequate fibre intake. Our finding is all the worse given that the overall energy consumption of our sample, which contributes to total fibre intake, was above that recommended by the IOM(29) of 10 460 kJ/d (2500 kcal/d) for the second and third trimesters of gestation. Another recent study of Brazilian pregnant women(Reference Castro, Kac and Sichieri39) reported a similar finding: 12 088 kJ/d (2889 kcal/d). Part of the present obesity epidemic results from excess weight gain in pregnancy, documented to be frequent in Brazil(Reference Nucci, Schmidt, Duncan, Fuchs, Fleck and Santos Britto5, Reference Kac40). Thus, increased fibre content must be achieved in conjunction with a reduction in overall energy intake.
The inadequacy of fibre intake in pregnancy we describe is not exclusive to southern Brazil. The mean daily fibre intake of our sample was two- to three-fold higher than in recent American(Reference Qiu, Coughlin, Frederick, Sorensen and Williams7, Reference Giddens, Krug, Tsang, Guo, Miodovnik and Prada19) and British samples(Reference Rees, Doyle, Srivastava, Brooke, Crawford and Costeloe23).
Nutritional education in routine prenatal care is a useful tool in the management of weight gain during pregnancy(Reference Nielsen, Gittelsohn, Anliker and O’Brien41, Reference Polley, Wing and Sims42). Advice about the energy density of foods is essential to avoid excessive weight gain, with foods rich in fibre being a critical part of this recommendation.
Given the lack of Brazilian studies assessing dietary fibre intake in pregnancy, we additionally contrasted the reported fruit and vegetable intake with recommendations of the Nutritional Guidelines for Brazilians, published in 2006(14). That 30–40 % of our sample did not achieve the recommended intake is in consonance with a recent national survey which estimates that a three-fold increase in consumption of these food items is necessary to meet recommended intake(43).
Our results also document the importance of consumption of legumes and fruits, which together furnished approximately half of total fibre intake. Indeed, consumption of beans has decreased considerably over the years in Brazil, and nutritional guidance should emphasize the nutritional value and low cost of this foodstuff. Fruits are somewhat more expensive, but again, strategies exist to increase availability and consumption of fruits, even among those with limited incomes.
The qualitative analysis of fibre intake showed that whole-grain cereals made up only 1 % of fibre intake from cereals. Several studies support the protective effect of whole-grain cereals against chronic diseases and mortality(Reference Jacobs, Meyer, Kushi and Folsom3, Reference Jacobs, Pereira, Meyer and Kushi25, Reference Murtaugh, Jacobs, Jacob, Steffen and Marquart44) and the consumption of most cereals as whole grains is a unanimous recommendation of nutrition guidelines. Our study thus emphasizes the distance between recommendation and reality in this regard, drawing attention to the importance of assessment and counselling concerning this most appropriate source of dietary fibre.
Our finding that receiving nutritional guidance was positively associated with meeting the recommendation for fibre intake emphasizes the role of the dietary counselling in prenatal care. Currently, nutritional guidance is not routinely structured within prenatal care in Brazil, leading to considerable variation in counselling across different practice settings. Greater efforts to educate pregnant women about fibre intake benefits and appropriate sources and quantity of dietary fibre might thus be of benefit.
Additionally, as those drinking alcoholic beverages were less likely to meet the fibre recommendation, poor dietary fibre intake may be part of a pattern of unhealthy behaviour. As this was an observational study, it is possible that women seeking healthy habits sought more dietary advice, avoided alcohol consumption and consumed greater quantities of fibre-rich foodstuffs.
Our study has limitations. It was not designed to be representative of pregnant women in the cities studied. On the other hand, we know of nothing particularly different in our sample from pregnant women in general seeking care at public primary care units in southern Brazil, and representative studies have not yet been undertaken. Another limitation is the important fraction of women excluded from analyses. Excluded subjects showed no important differences in basic sociodemographic criteria, thus minimizing risk of serious bias. Exclusion of women reporting extremes of total energy or fruit and vegetable intake probably led to some underestimation of total daily fibre intake. Yet, even with their inclusion, the percentage of women reporting inadequate intake was 41 %, still a large fraction of the sample. The true fraction of inadequate total daily fibre intake thus probably lies somewhere between 41 % and 50 %.
The difficulty in estimating food consumption accurately and precisely in epidemiological studies is also a limitation. No method exists which is capable of measuring dietary intake flawlessly in large samples. FFQ such as ours are widely used to assess habitual diet in epidemiological research, including that in pregnancy(Reference Olson13, Reference Harley, Eskenazi and Block20, Reference George, Hanss-Nuss, Milani and Freeland-Graves22, Reference Arkkola, Uusitalo, Pietikainen, Metsala, Kronberg-Kippila, Erkkola, Veijola, Knip, Virtanen and Ovaskainen45), given their ability to classify individual eating patterns, their ease of administration and their relatively low cost. That we had previously validated the questionnaire used in the present study against 24 h dietary recalls of pregnant women for this population increased its accuracy and precision.
The present study can contribute to clinical practice by drawing attention to an important issue in nutritional prenatal care – low dietary fibre intake. Few studies of nutritional intake in pregnancy have assessed dietary fibre intake within the context of the nutritional transition in low- and middle-income countries. Greater attention should be given to consumption of dietary fibre in order to improve the profile of food intake, providing greater nutritional density, i.e. more nutrients per kilojoule consumed, while augmenting satiety. The assessment of food habits in pregnancy is fundamental to guide nutritional education. Health policies should emphasize the importance of a healthy diet in pregnancy and encourage a more appropriate level of dietary fibre intake.
Conclusions
Approximately half of pregnant women studied did not meet the cut point of 28 g/d used as a recommendation for dietary fibre intake. Receiving nutritional guidance and greater ingestion of legumes and fruits were positively associated with reaching this cut point. The greatest source of dietary fibre intake was refined cereals, with whole-grain cereal providing a trivial percentage of fibre intake. Specific guidance in prenatal care nutritional counselling is needed regarding fibre intake in order to maximize short-term health benefits for pregnant women and long-term prevention of chronic disease.
Acknowledgements
This submission represents original work and has not been published previously. It is not currently being considered by another journal, and following acceptance for Public Health Nutrition will not be published elsewhere in the same form, in English or in any other language, without the written consent of the Nutrition Society. Each author has seen and approved the contents of the submitted manuscript. The authors have no conflict of interest.
Contribution of each author to the manuscript: The data reported in the present article were collected as part of the first author’s MS dissertation that was supervised by M.A.N., S.C. and M.I.S. All authors were responsible for the design and performance of the ECCAGE Study. C.B. was responsible for the dietary assessment. C.B. and S.C. analysed the data. C.B., B.B.D. and M.I.S. wrote the paper with contributions from the other co-authors.
Sources of funding: Centers of Excellence Grant of CNPq (the Brazilian National Council of Technological and Scientific Development); CAPES/MEC (the Brazilian Ministry of Education).






