Eating regular meals is one of the potential energy balance-related behaviours( Reference Kremers, de Bruijn and Visscher 1 ). Meals are often defined as eating breakfast, lunch, dinner and small snacks such as mid-morning, mid-afternoon and evening( Reference Mota, Fidalgo and Silva 2 ). Main meals are in many countries breakfast, lunch and dinner, but can differ; e.g. in Norway there is usually a fourth main meal: evening meal (served in the evening due to an earlier dinner compared with most countries). Children's meal pattern in the USA have changed over a two-decade period, making skipping of meals more prevalent( Reference Nicklas, Morales and Linares 3 ). Unhealthy dietary habits, including irregular breakfast eating, have also been reported among Norwegian adolescents( Reference Samdal, Leversen and Torsheim 4 , Reference Øverby and Andersen 5 ). Worldwide, the prevalence of obesity increased dramatically during the last decades( Reference Lobstein, Baur and Uauy 6 – Reference Han, Lawlor and Kimm 9 ), although new findings support a levelling off in children and adolescents from Australia, Europe, Japan and the USA( Reference Rokholm, Baker and Sørensen 10 ). In Norway, increasing prevalence of overweight has been observed in children and adolescents over the last decades( Reference Juliusson, Roelants and Eide 11 ). Still, there is overwhelming agreement that the levels of overweight and obesity among children are too high.
High meal frequency (4 or 5 v. ≤3 meals/d) has been observed to be inversely associated with childhood obesity in cross-sectional studies( Reference Mota, Fidalgo and Silva 2 , Reference Toschke, Kuchenhoff and Koletzko 12 – Reference Vik, Overby and Lien 14 ). Longitudinal associations between a regular meal pattern/high meal frequency and obesity are scarce in this field, but a 10-year observational study among American adolescent girls revealed that a frequency of 3+ meals/d was positively related to a lower BMI-for-age Z-score( Reference Franko, Striegel-Moore and Thompson 15 ). The study also revealed that the percentage of girls skipping meals increased from the age of 9 to 19 years( Reference Franko, Striegel-Moore and Thompson 15 ).
Food habits and meal patterns, which are learned and acquired in childhood, tend to persist into later ages. Evidence also shows that childhood overweight tracks into adulthood( Reference Singh, Mulder and Twisk 16 ). Therefore, a focus on eating regular meals could be a possible target for early prevention of overweight and obesity in children and possible longitudinal associations are of particular interest to investigate causality.
The aims of the present study were to: (i) assess the meal pattern of Norwegian schoolchildren in 4th and 7th grade and describe longitudinal changes; and (ii) assess the association between meal skipping and overweight.
Methods
Participants and study design
The present data were obtained from a study of primary-school pupils in Telemark County, Norway. Data collection took place in the spring of 2007 and spring of 2010, when the children were in primary school grades 4 (9–10 years old) and 7 (12–13 years old), respectively. The detailed methods for the 4th grade data collection have been described previously( Reference Oellingrath, Svendsen and Brantsater 17 ). An identical procedure was used for data collection in the 7th grade( Reference Oellingrath, Svendsen and Brantsaeter 18 ).
In brief, all primary schools in Telemark County were invited to participate in the study at both time points. In 2007 (4th grade), 110 schools were invited and seventy agreed to participate. Due to merging of some schools in the period between the two data collection points, 104 schools were invited in 2010 and fifty-three agreed to participate. Of the fifty-three schools participating in 2010, forty-six also attended in 2007 and six schools were new participants.
In total, written parental consent to inclusion in the study was received for 1045 out of 1477 invited children in the 4th grade and 1095 out of 1503 invited children in the 7th grade. This represented about half of the county's 4th and 7th grade pupils at the respective time points.
Weight and height measurements were obtained for 955 (4th grade) and 865 (7th grade) children, while complete weight/height and meal frequency data were obtained for 924 and 690 pupils, respectively. In total, 428 children (207 boys and 221 girls) provided complete weight, height and meal frequency data at both time points.
The study was conducted according to the guidelines laid down in the Declaration of Helsinki and ethical approval and research clearance were obtained from the Norwegian Social Science Data Services. The parents and the children received separate information letters. The parents gave their written consent to participate including a confirmation that their child wanted to participate too.
Dietary information
The children's habitual daily consumption of main meals (breakfast, lunch, dinner and evening meal) during the last 6 months was reported by their parents using a retrospective FFQ that included information about meal frequencies. Meal frequencies were registered with eight response alternatives ranging from ‘never/rarely’ to ‘daily’. The questionnaire was based on a short FFQ developed for use with children in grades 4 and 8 in Norway( Reference Lillegaard, Overby and Andersen 19 ), but was modified to include more dietary questions. Before the study, the FFQ was tested on a sample of parents and followed up by qualitative interviews( Reference Schelling and Streitlien 20 ). Identical FFQ were used at both time points and the questionnaires were distributed at school and returned to school.
The numbers of days reported eating breakfast, lunch, dinner and evening meals were then collapsed into dichotomous variables. Children who ate these main meals fewer than 7 d/week were classified as breakfast, lunch, dinner and evening-meal skippers, respectively. Children who ate these main meals every day were classified as regular breakfast, lunch, dinner and evening-meal consumers. These dichotomous variables were then combined to create a summary variable referred to as ‘all regular meals’, i.e. those eating all meals (1) v. those skipping meals (0) in respectively 4th and 7th grade. For the longitudinal analyses in the present study, the children were further categorized into a new variable to describe meal skipping longitudinally, giving a variable of four categories: (i) CONTINUED skippers (skipping meals at both time points); (ii) START all meals (meals skippers in 4th grade, eat all meals in 7th grade); (iii) STOP all meals (eat all meals in 4th grade, meal skippers in 7th grade); and (iv) ALL meals (eat all meals at both time points).
Other variables
To measure physical activity, the parents provided information about how many hours their children spent on sports or exercise that made them sweat or feel breathless outside school, with response alternatives ranging from ‘none’ to ‘seven hours or more during a normal week’.
Maternal educational level was collected by asking for the highest completed education and divided into three categories: (i) ‘primary and lower secondary education’ (10 years or less); (ii) ‘upper secondary education’ (3 to 4 years of secondary education); and (iii) ‘university or university college’.
BMI categories
The weight and height of all the participating children were measured by public health nurses at each school at both time points. The children were weighed wearing light clothing (i.e. trousers, T-shirt, socks), using identical calibrated, electronic scales measuring in 100 g increments. BMI (kg/m2) of each child was calculated on the basis of these measurements. Child BMI categories (underweight, normal weight, overweight, obese) were calculated using sex- and age-specific cut-off points of the International Obesity Task Force( Reference Cole, Flegal and Nicholls 21 , Reference Cole, Bellizzi and Flegal 22 ). Due to small numbers, we included underweight children in the normal-weight group and obese children in the overweight group.
Statistics
Descriptive data comparing 4th and 7th graders in Norway were analysed by paired-sample t tests for continuous variables and χ 2 tests for categorical variables. Four separate groups were described (i.e. CONTINUED skippers, START all meals, STOP all meals and ALL meals). ALL meals, as the preferred meal pattern, was compared with the rest of the study sample. Odds ratio estimates, including confidence intervals, with weight status as the dependent variable, were determined through logistic regression analyses (Table 2). All of the following logistic regression models were adjusted for maternal education and gender. Furthermore, model 1 included meal pattern (CONTINUED skippers, START all meals, STOP all meals v. ALL meals as the reference; Table 2). Model 2 included meal pattern and physical activity and model 3 included meal pattern, physical activity and overweight status in 4th grade (Table 2). All statistical analyses were performed using the statistical software package IBM SPSS Statistics 19·0.
Results
The children with complete data in both 4th and 7th grade were generally from families with somewhat higher educational level than those without complete data (56 % v. 51 % of the parents, respectively, had ‘university or university college’; P = 0·003). No difference in participation with regard to gender was observed.
In 4th grade, a total of 203 (47 %) of the children were reported to eat all four meals every day whereas 146 (34 %), sixty-six (15 %), eleven (3 %) and two (1 %) children ate three, two, one or none of these main meals every day during a week, respectively. In 7th grade, a total of 166 (38 %) of the children were reported to eat all four meals every day whereas 143 (33 %), ninety-one (21 %), twenty-two (5 %) and eight (2 %) children ate three, two, one or none of the main meals every day during a week, respectively.
In both 4th and 7th grade, approximately 90 % of the children had regular breakfast habits and 85 % consumed dinner regularly (Table 1). Further, the results showed a significant decrease in the proportion reporting to eat regular lunch meals, from 81 % to 75 % (P = 0·010), and regular evening meals, from 67 % to 53 % (P < 0·001), between 4th and 7th grade. Thus, the frequency of children who ate all four main meals regularly decreased significantly from 4th grade (47 %) to 7th grade (38%; P = 0·001). No gender differences in meal skipping were observed in 4th grade or 7th grade (data not shown). A significant increase in physical activity (P < 0·001), but no change in the overweight prevalence among children was observed from 4th to 7th grade (Table 1). Tracking of 4th grade overweight/obese children (n 68) showed that forty-four (65 %) remained overweight/obese in 7th grade (Fig. 1). Among the 4th grade normal-weight children (n 360), 339 (94 %) remained normal weight and twenty-one (6 %) became overweight/obese in 7th grade (Fig. 1).
Table 1 Descriptive data of the study sample of primary-school children (4th graders in 2007, 7th graders in 2010), Telemark County, Norway (n 428)
*Paired-sample t test was used to analyse changes in physical activity and χ 2 tests were used to analyse changes in all other variables.
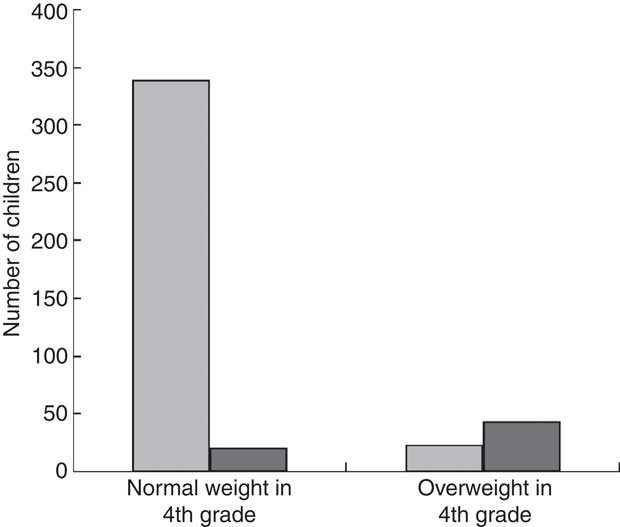
Fig. 1 Changes in BMI status between 4th and 7th grade among a sample of primary-school children (4th graders in 2007, 7th graders in 2010), Telemark County, Norway (n 428): ![]() , normal weight in 7th grade;
, normal weight in 7th grade; ![]() , overweight in 7th grade
, overweight in 7th grade
Among the total sample, 41 % of the children skipped meals in both 4th and 7th grade (CONTINUED skippers) whereas 11 % reported to eat all meals only in 7th grade (START all meals) and 21 % reported to eat all meals only in 4th grade (STOP all meals; data not shown). A total of 27 % of the children reported to eat all meals (ALL meals) at both time points (data not shown).
Those included in the category STOP all meals did have greater odds of being overweight in 7th grade, adjusting for sex, maternal education and physical activity, than those who ate ALL meals (OR = 3·1; 95 % CI 1·1, 9·0), but the odds ratio was not statistically significant after adjusting for overweight in 4th grade (Table 2). The odds of being overweight in 7th grade among those included in the categories START all meals and CONTINUED skippers was not significantly different from those who ate all meals.
Table 2 Logistic regression models describing odds of being overweight in 7th grade, adjusted for physical activity and overweight in 4th grade, among a sample of primary-school children (4th graders in 2007, 7th graders in 2010), Telemark County, Norway (n 428)
Ref., reference category.
All three models were adjusted for gender and maternal education.
*CONTINUED skippers = meal skippers at both time points; START all meals = meal skippers in 4th grade, eat all meals in 7th grade; STOP all meals = eat all meals in 4th grade, meal skippers in 7th grade; ALL meals = eat all meals at both time points.
Discussion
The present study showed an overall increase in meal skipping with increasing age. While the frequency of breakfast and dinner skippers remained relatively stable (approximately 10 % and 16 %, respectively), significant increases in skipping lunch (from 19 % to 25 %) and evening meals (from 33 % to 47 %) were reported between 4th and 7th grade. Few other studies have described longitudinal changes in meal pattern among children and adolescents.
In agreement with results from the present study, a cross-sectional study among children of pre-school age in Canada reported that one-tenth of the children ate breakfast on fewer than 7 d/week( Reference Dubois, Girard and Potvin Kent 23 ). An American study showed that 20 % of 4th grade students were skipping breakfast and/or lunch at least three times per week( Reference Franko, Striegel-Moore and Thompson 15 ), whereas a Finnish study reported that practically all children between 10 and 11 years old (99 %) had breakfast, 94 % had lunch and 80 % had dinner regularly( Reference Haapalahti, Mykkänen and Tikkanen 24 ). Among Swedish adolescents in 9th grade, only 76 % of girls and 88 % of boys reported to eat breakfast regularly( Reference Sjoberg, Hallberg and Hoglund 25 ). Unhealthy dietary habits, including irregular breakfast eating, have also been reported among Norwegian adolescents( Reference Samdal, Leversen and Torsheim 4 , Reference Øverby and Andersen 5 ).
In addition to age- and regional-related trends, studies from the 1970s to today have reported a tendency towards a decrease in meal frequency and going from regular meals to skipping main meals among children and adolescents( Reference Nicklas, Morales and Linares 3 , Reference Samuelson 26 ).
The relationship between meal pattern and overweight has been widely debated; several cross-sectional studies have observed a positive association between meal skipping and the prevalence of overweight( Reference Mota, Fidalgo and Silva 2 , Reference Sjoberg, Hallberg and Hoglund 25 , Reference Storey, Forbes and Fraser 27 – Reference Croezen, Visscher and ter Bogt 30 ), while others have not supported these associations( Reference Nicklas, Morales and Linares 3 ). However, few longitudinal studies have been published. We have previously shown that children adhering to a ‘varied Norwegian’ eating pattern, which included regular breakfast and eating lunch, were less likely to remain overweight( Reference Oellingrath, Svendsen and Brantsaeter 18 ). The present study showed that those who stopped eating regular meals after 4th grade were three times more likely to be overweight in 7th grade compared with those who ate regular meals in both 4th and 7th grade after adjusting for physical activity. However, this relationship did not remain significant after adjusting for overweight in 4th grade, but remained of comparable amplitude. Not surprisingly, overweight in 4th grade appeared to be the most important predictor of overweight in 7th grade. We have previously reported a high degree of BMI tracking from 4th to 7th grade in the same cohort( Reference Oellingrath, Svendsen and Brantsaeter 18 ). However, adjusting for physical activity had a larger impact than overweight at 4th grade on the estimated odds ratios for meal skipping. This indicates an important association between physical activity, regular meal pattern and overweight.
Other longitudinal studies have reported an inverse relationship between meal frequency and BMI( Reference Rokholm, Baker and Sørensen 10 , Reference Lillegaard, Overby and Andersen 19 , Reference Singh, Mulder and Twisk 31 – Reference Affenito, Thompson and Barton 33 ), but contrary to the present study, a 9-year American longitudinal study described that this association was not significant after adjusting for physical activity( Reference Affenito, Thompson and Barton 33 ).
An important strength of the present study is the longitudinal design, which allowed for examining long-term associations between effects of meal regularity and overweight. The objective measurement of the children's weight and height at both time points, further categorized into BMI categories by international criteria( Reference Oellingrath, Svendsen and Brantsater 17 , Reference Oellingrath, Svendsen and Brantsaeter 18 ), is another major strength of the study.
A lack of statistically significant associations, despite a high odds ratio between irregular meal consumption and overweight in the analyses after adjusting for all confounders, may be explained by insufficient statistical power. The present study also has other limitations. First, it included the use of parental self-reported data. Although validated survey components were used, self-reported data may represent recall bias and response bias regarding dietary habits( Reference Bandini, Must and Cyr 34 ). Under-reporting of food intake has been widely reported, and this is particularly evident for individuals who are overweight( Reference Lobstein, Baur and Uauy 6 , Reference Wang and Lobstein 7 ). We cannot exclude the possibility that parents of overweight children may have under-reported unhealthy meal habits. However, this might be a minor problem in the present study as parents reported only meal habits and not detailed information about children's food intake. In Norway, there are no school-prepared meals, so most children bring their own lunchbox consisting of cold sandwiches. Most schools offer a milk prescription programme and water is available from the tap. Some misreporting of children's lunch consumption is likely, as parents normally are aware of what the children bring for lunch at school, but not if they actually eat it. In addition, the results from the present study may partly be limited by the sample size, i.e. a relatively low number of overweight children who were defined as meal skippers. Despite the limitations mentioned, few other longitudinal studies have focused on the association between meal pattern and overweight.
Conclusion
The present study showed significant increases in overall meal skipping among children between 4th and 7th grade. The results indicate an association between overweight and meal skipping, but additional prospective and longitudinal analyses and intervention trials are warranted to confirm this relationship. The results indicate that a focus on a regular meal pattern should be considered when developing guidelines to prevent childhood overweight.
Acknowledgements
Sources of funding: This research was supported by Telemark University College, Telemark Hospital, the Research Council of Norway and the Public Health Programme of Telemark. The Research Council of Norway and the Public Health Programme of Telemark had no role in the design, analysis or writing this article. Conflicts of interest: The authors certify that no actual or potential conflicts of interest in relation to this article exist. Ethics: The study was conducted according to the guidelines laid down in the Declaration of Helsinki. The research protocol was approved by the Regional Committee for Ethics in Medical Research and the Norwegian Data Inspectorate. Ethical approval and research clearance and were obtained from the Norwegian Social Science Data Services. Authors’ contributions: I.M.O. and M.V.S. were responsible for the study design and data collection. T.H.S. and E.B. were responsible for the statistical analyses. All authors contributed to the interpretation of the results. T.H.S. and F.N.V. drafted the manuscript, and the other authors revised it critically. All authors read and approved the final version of the manuscript. Acknowledgements: The authors appreciate the cooperation of the children and their parents, the faculty and staff of the Telemark County primary and lower secondary schools, and the public health nurses who participated in the study.





