In recent years there has been a growth in services for eating disorders, demand for which is often fuelled primarily by severe anorexia nervosa (AN), although the latter clinical group only represents a small proportion of referrals for specialist help. Those planning such services need to be able to predict the likely demand, both in terms of numbers and types of referral and the likely service input required for a range of patients. Although the epidemiology of eating disorders has been well researched, information about service consumption across the spectrum of eating disorders is less readily available. Button et al (Reference Button, Marshall and Shinkwin1997) described service consumption in a cohort of 100 referrals to an established service for adults with eating disorders. This showed wide variation, with patients with AN having longer and more intensive therapy than those with bulimia nervosa (BN) or ‘partial syndrome’ eating disorders. This cohort, however, included some tertiary referrals from outside the local catchment area who might be expected to receive more intensive treatment.
The present study aims to describe 3 years’ service consumption in a cohort of adult referrals to a specialised eating disorders service arising from a defined catchment area within the National Health Service. It is hoped that the results will help inform others engaged in planning and developing such services.
Method
We identified from clinical records the cohort of patients referred in 1999 to the Leicestershire Adult Eating Disorders Service from the local catchment area, which has a population of about 950 000. The service takes referrals aged 16 and above and offers treatment for AN, BN and eating disorder not otherwise specified (EDNOS). The latter term is a category within the DSM-IV (American Psychiatric Association, 1994) criteria for eating disorders, which includes binge eating disorder and other clinically significant disorders of eating which do not meet all the criteria for AN or BN. Diagnoses were based on the DSM-IV criteria and derived from a detailed semi-structured clinical interview conducted by or under the close supervision of an experienced clinician specialising in eating disorders (consultant psychiatrist, clinical psychologist or clinical nurse specialist). We can thus be fairly confident that diagnostic criteria were as rigorously applied as might be expected in a service setting.
Both electronic and clinical records were inspected and data were extracted concerning demographic and clinical status at assessment. We also recorded ‘ service consumption’ during the next 3 years, including number of referrals, out-patient and day-patient attendance and in-patient admissions.
Statistical analysis
We used the Statistical Package for the Social Sciences (version 11.5 for Windows) to provide basic descriptive statistics, as well as exploring subgroup differences and correlational data.
Results
Baseline clinical characteristics
In total, 147 local patients who had been assessed during 1999 were identified. They were predominantly female (96%), with a mean age of 26.3 years, and 91% were classified as ‘White British’. Only 4.3% were of Asian (Indian subcontinent) background, which is an under-representation of what might be expected in a multicultural city such as Leicester (Reference Ratan, Ghandi and PalmerRatan et al, 1998).
Most (82%) referrals were directly from general practitioners. Although only 16% were re-referrals to the service, about a third had received some previous form of professional help.
The most common diagnosis was EDNOS (43% of the cohort and 45% excluding those with a missing diagnosis), followed by BN (36.7%) and AN (6.8%). Only 1 in 9 patients were not considered to have a clinical eating disorder. These were heterogeneous and included vomiting phobia, low weight/loss of appetite in association with anxiety, depression or some physical illness and people who were overweight, but with no binge-eating or significant compensatory behaviour.
The main clinical details at assessment by diagnosis are summarised in Table 1. As expected, AN patients differed from the other diagnostic groups in terms of weight (P<0.005) and menstrual status (P<0.05). EDNOS patients were of similar weight and menstrual status as those with BN. It should be noted, however, that the EDNOS group had a higher standard deviation for current body mass index than the other groups, suggesting that they are a rather diverse group in terms of body size. EDNOS patients showed similar levels of eating pathology as AN and BN, with 69% restricting eating at least most days. The next most common weight control strategy in EDNOS patients was strenuous exercise, with 36% partaking at least weekly, a level similar to those with BN. For self-induced vomiting (32%) and laxative abuse (13%) they showed levels intermediate between AN and BN. EDNOS patients also showed similar levels of attitudinal concerns as those with AN and BN in terms of intense fears of weight gain (81%), body image disturbance (48%) and self-evaluation unduly influenced by weight or shape (78%).
Table 1. Clinical characteristics at assessment by diagnosis (percentages unless otherwise stated)
| Variable | Whole cohort (n=147*) | Anorexia nervosa (n=10) | Bulimia nervosa (n=54) | Eating disorder not otherwise specified (n=63) |
|---|---|---|---|---|
| Current body mass index: mean (s.d.) | 23.5 (8.3) | 15.5 (1.6) | 24.1 (5.5) | 25.0 (10.5) |
| Regular periods (excluding those on the pill) | 40.1 | 0.0 | 61.0 | 54.3 |
| Restrained eating (at least most days) | 56.0 | 90.0 | 48.9 | 68.8 |
| Self-induced vomiting (at least weekly) | 46.0 | 10.0 | 82.4 | 31.7 |
| Strenuous exercise (at least weekly for weight control) | 35.3 | 60.0 | 39.2 | 36.2 |
| Laxatives (at least weekly for weight control) | 12.8 | 10.0 | 17.6 | 12.9 |
| Binge-eating (at least weekly) | 47.8 | 10.0 | 100.0 | 23.3 |
| Intense fear of weight gain | 73.0 | 90.0 | 86.0 | 80.6 |
| Body image disturbance | 47.5 | 50.0 | 65.3 | 47.5 |
| Self-evaluation unduly influenced by weight/shape | 79.9 | 90.0 | 98.0 | 78.3 |
Service consumption
During the 3 years after referral in 1999, the majority of patients had only one episode of care with the service, but 12.3% were discharged and re-referred during this period. Two patients were referred three times.
The predominant form of treatment was out-patient only (93.9% of patients). The number of out-patient appointments attended was highly skewed, with a median of 6.5 and a range of 1-139. Almost one-third of patients (31.3%) attended only once or twice. However, 7 patients (4.8%) had over 40 appointments. Of these, 4 had a diagnosis of EDNOS.
Only 9 patients (6.1%) had in-patient treatment with the service during the 3 years. Two of these had more than one admission, 1 of whom had four admissions. Two patients (1.4%) attended our day programme, both of these patients had also had in-patient treatment. For the 9 patients receiving in-patient treatment, the median stay was just 15 days, with a range of 5-236 days. In the case of day care, 1 patient stayed 89 days and the other 193 days. Surprisingly, only 1 of the 9 patients had a diagnosis of AN. Almost half of all in-patient days were accounted for by 1 EDNOS patient alone. The majority of admissions were associated with low mood and suicidal risk.
Length of contact and status after 3 years
The median length of contact with the service was 5.7 months, but the length of contact with the service was highly variable, as illustrated in Fig. 1.
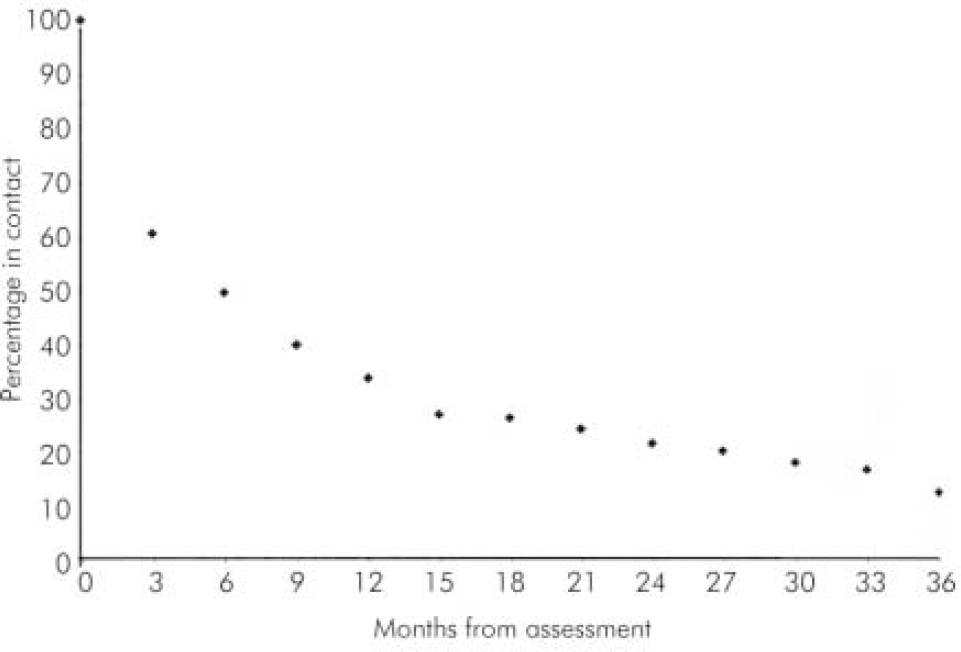
Fig. 1. Percentage of patients in contact over time.
There is a marked drop-out during the first 3 months, by which time only around 60% of patients assessed are still in contact. The rate at which patients lose contact declines steadily during the next year, so that by 12 months around one-third are still in contact. At the end of 3 years, only 18 patients (12.2%) were still active (appointment attended within last 3 months) and 87% were discharged.
The most common reason for discharge from the service was ‘ drop-out’ (58.8%). A further 7.8% of discharges involved referral to another service and in one-third of patients (32.8%) there was an ‘ agreed discharge’, in which patient and therapist had jointly agreed to end therapy.
Service consumption by diagnosis
After excluding patients with no eating disorder, there was no statistical association between service consumption and diagnosis either for appointments or length of contact. One half of all out-patient appointments were for patients diagnosed as EDNOS at first assessment. Moreover, of the 18 patients still in contact after 3 years, 8 were from the EDNOS group.
Discussion
The majority of referrals were considered appropriate, with a DSM-IV diagnosis of eating disorder, and the most common diagnosis was ‘eating disorder not otherwise specified’ (43%). EDNOS patients presented with clinical symptoms similar to those characteristic of AN and BN, including high levels of restrained eating, intense fear of weight gain, and self-evaluation unduly influenced by weight/shape. They also showed significant levels of vomiting, laxative abuse and strenuous exercise for weight control. These findings are similar to a study by Ricca et al (Reference Ricca, Mannucci and Mezzani2001), which also reported a similar proportion of EDNOS patients (43.8%) in a consecutive series of out-patients attending two Italian eating disorder units.
The main focus of the study was service consumption among local referrals; among all patients the predominant form of treatment is at out-patient level and generally is relatively short-term, although the distribution of the number of appointments is highly skewed. Many quickly dropped out of contact with the service, but 12% were still in touch after 3 years. Compared with the previous study from the same service (Reference Button, Marshall and ShinkwinButton et al, 1997), this cohort had a lower overall level of service consumption. However, the earlier study included referrals from outside the catchment area.
The most striking finding from the present study is the lack of relationship between service consumption and diagnosis. Patients with EDNOS had at least as many out-patient appointments as those with AN or BN and account for a half of all appointments across the cohort and a similar proportion of in-patient days. This is in contrast to an earlier study from the same service (Reference Button, Marshall and ShinkwinButton et al, 1997), in which patients with AN had more appointments and longer contact with the service; however, the earlier cohort included tertiary referrals, many of whom would have had severe AN and would have required more intensive treatment. It is also possible that the present cohort was unusual in that it may have included fewer than expected local patients with severe AN. Nevertheless, such patients are always likely to form only a small minority of people with eating disorders presenting to a service based on catchment area.
Our data show that EDNOS patients are the most common diagnostic group and take up around one-half of the resources of our service. This is an important consideration given that the demand for services for eating disorders tends to emphasise the major syndromes of AN and BN. This is also reflected in the recent National Institute for Clinical Excellence guidelines (NICE, 2004) which are largely taken up by detailed recommendations for the treatment of these two disorders.
The present study is limited by being based on a single service in one English county and it cannot be assumed that patterns of service delivery and consumption are the same elsewhere. Moreover, the study is based on only 1 year's cohort and we cannot be sure how representative this year was; it is possible that patterns of service delivery and consumption vary over time.
In conclusion, the results from our local cohort suggest that service consumption for patients with eating disorders is highly variable and cannot simply be accounted for by diagnosis. Our findings suggest that where specialist secondary services for adults with clinical eating disorders are available, EDNOS patients are likely to form a major part of the demand. Such people should not be seen as presenting trivial symptoms and their need for help is similar to those with AN and BN. The substantial needs of patients with EDNOS should be taken into account in planning specialised services for adults with eating disorders. Further research is required to examine factors other than diagnosis that may predict service consumption.





eLetters
No eLetters have been published for this article.