1 Introduction
Microsystems – small functional units, such as clinics, wards, or general practices – are the smallest building blocks of any healthcare system. The clinical microsystem improvement approach seeks to engage frontline interprofessional teams, patients, and families in a structured process to improve the quality of care and outcomes, typically focused on one microsystem or a mesosystem (care pathway). It uses a range of tools and frameworks designed to engage patients and families in improvement efforts and co-production of care, increase capability to provide and improve care, improve team dynamics, and create an enhanced sense of ownership of the microsystem or mesosystem. Supporting teams through interventions such as team coaching, it addresses not only technical improvement but also the human and relational aspects involved in change.
The approach has its origins in mixed-method research conducted at The Dartmouth Institute for Health Policy and Clinical Practice (TDI) in the United States in the 1990s examining the attributes of high-performing microsystems.Reference Donaldson and Mohr1, Reference Nelson, Batalden and Huber2 This work led to the development of an approach known as the Dartmouth Microsystem Improvement Curriculum (DMIC) which offers, among other things, a set of tools, techniques, and practices. Subsequent developments have included formalisation of a ‘team coaching’ model and the emergence of mesosystem initiatives that adapt microsystem frameworks and principles to improve care pathways consisting of multiple microsystems.
2 Microsystems and Mesosystems
Box 1 Definitions of microsystems and mesosystems
Microsystems: Small, functional frontline care units or departments, for example, a clinic, a ward, or a surgery. They are defined as the place where patients and the care teams meet.
Mesosystems: A collection of two or more linked microsystems (also known as care pathways or flow levels).
Microsystems (see Box 1) are the building blocks of the healthcare system,Reference Nelson, Batalden and Godfrey3 typically comprising bounded care units or departments. Mesosystems (care pathways) comprise two or more units (microsystems). Microsystems (e.g. a ward) and mesosystems (e.g. a clinical pathway) themselves sit within an organisational context – the macrosystem (e.g. a hospital) – which in turn sits within a broader geopolitical system, such as the NHS.
A clinical microsystem includes not only the multidisciplinary team involved directly in care but also all the other colleagues involved (e.g. booking and reception staff) and patients and families. The work of clinical microsystems is enabled by supporting microsystems, such as pharmacies, estates, and IT, that both operate as microsystems in their own right and are stakeholders in many microsystems across an organisation. Microsystems do not sit in isolation: they are located in and strongly influenced by the context of a broader organisation and healthcare system. Fundamental to microsystem thinking is the concept that the quality and value of care produced by a large healthcare system can be no better than that of the services generated by the small systems of which it is composed.Reference Nelson, Batalden and Godfrey3
Patients rarely receive all their care for a particular condition in one microsystem, but from a collection of linked microsystems termed the mesosystem, flow level, or care pathway. This collection of interrelated microsystems forms a mesosystem. Improvement efforts focused on mesosystems (care pathways) can adapt the Flow approach,Reference Crisp, Watt, Jones, Amevenu and Warburton4 where multiple microsystems that comprise the pathway are discussed in a ‘big room’, loosely based on the Toyota Obeya method for complex product design.Reference Liker5 A virtual or physical space, the big room enables a view of the pathway as a series of interrelated microsystems. It can support recognition of the complex nature of the pathway and target key areas for change by reviewing performance data and processes of the mesosystem pathway together.
In both microsystem and mesosystem approaches, the improvement work is supported by coaching – team coaching for microsystems and Flow coaching for mesosystems. Team coaches guide the improvement team through an ‘improvement ramp’ or roadmap, using skills such as encouragement, reframing, conflict management, and focus to support the human and relational aspects of the change process. Both approaches also require regular team meetings using effective meeting skills – such as timed agendas with meeting roles and ground rules that guide working together – to support progress and enable the improvement team to establish improvement habits and relationships.
3 Tools and Techniques
Both the microsystem and mesosystem improvement approaches promote the practical organisation of improvement work and seek to enhance team communication and dynamics. Field-tested tools and techniques have been integrated into a practical, disciplined, and structured approach to microsystem improvement – the DMIC – that teams can learn and use. We set out three major elements of the microsystem improvement approach – the improvement ramp, 5P assessment, and use of team or Flow coaching – and give examples of each.
3.1 Creating Ownership
The microsystem approach requires the active involvement of the interprofessional team, including leadership, in regular meetings (weekly or biweekly is recommended) to develop a rhythm of improvement work and redesigning care. Key stakeholders who play a part in the care should be involved – including doctors, nurses, therapists, clerical workers, ancillary workers, and managers. There should also be representation from any key supporting microsystems. Bringing patient and family voice and experience into the microsystem improvement meetings is integral and at the heart of all improvement.
Improvement team members are intended to become more engaged in their microsystem in the regular improvement meetings, learning about the processes of care, communicating and problem-solving together, and achieving a sense of ownership of the microsystem. The process of assessing, diagnosing, treating, and sustaining invites all members of the microsystem to participate in the improvement process at some level and so the activity of gaining buy-in becomes less necessary.Reference Lipmanowicz6
3.2 The Microsystem Improvement Ramp
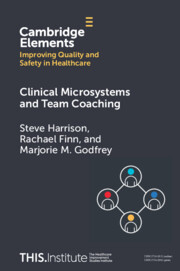
A key element of the DMIC is the microsystem improvement ramp (Figure 1).Reference Nelson, Batalden and Godfrey3
Figure 1 The microsystem improvement ramp
The ramp is a four-step process:
1. Assess: Collectively understanding the current system before improvement begins, providing the interprofessional improvement team with opportunities to learn about each other’s contributions to the processes of care and to see the system of care through new perspectives. 5P assessment (see Section 3.3) can be used to support this understanding.
2. Diagnose: Based on the initial 5P data and information assessment, themes for improvement can be identified. To begin with, one improvement theme is selected to focus on. In the diagnosis phase, narrowing the improvement theme identified from the assessment phase occurs by creating a global aim (defining a process to be improved), creating a process map of the selected process, and then writing a specific aim statement (a measurable aim to improve a part of the process), which leads to further detailed diagnosis by creating a fishbone diagram to identify the cause and effects of the current issue or consider an ideal state.
3. Treat: Once the specific improvement process has been diagnosed, practical ideas for improvement are developed through benchmarking and then brainstorming and multi-voting. Multi-voting is conducted with all the interprofessional members and can reduce the number of change ideas to test.Reference Langley, Moen and Nolan7 Measures to assess the success and learning are defined and the change ideas are tested using PDSA cycles – sequential rapid tests of change aimed at generating knowledge about the impact and success of these ideas.
4. Sustain: The last step is to consider how to make the changes become habits and how to sustain this over time. This step aims to ensure that the redesigned process is documented through a playbook process and is usual practice for all members of the microsystem. Repeated review and measurement of the improved processes (standardise-do-study-act (SDSA) cycles) confirms if the new process is ‘the way we do things around here now’.
3.3 5Ps Assessment
Microsystem improvement uses a structured approach known as 5Ps assessment to understand systems and performance (see Table 1). 5P assessment structures understanding of the purpose of the clinical microsystem, the patients/populations being served, the professionals providing care and services, the core and supporting processes of the clinical microsystem, and the patterns (including culture, communication, relationships, and outcomes).Reference Nelson, Batalden and Godfrey3 Doing this work helps to identify the priorities for improvement.
Table 1 The 5Ps assessment
| Purpose | High-performing microsystems have a clear purpose. Agreeing on a purpose statement during the 5Ps analysis supports the team to consider and discuss ‘why does our microsystem exist?’ and ‘do we all share a common goal and aim?’. Active discussion of the purpose connects individual members with each other and the microsystem purpose and is particularly relevant when patients and families are included in the discussion. |
| Patients | General knowledge and facts about the population are often unknown or not shared by all members of the microsystem team, even though many will have their own knowledge of the patients they provide care to. Assessing information about this population can give insights to deliver care more effectively. |
| Professionals | Every member of the microsystem who provides or contributes to the care of patients should be thought of as a professional. Learning more about the staff, what they do, when they work, and how they rate the workplace is an important part of understanding any microsystem. Conversations, focus groups, and staff surveys can provide insights into what would make the microsystem better for patients and the team. |
| Processes | The microsystem members participate in core and supporting processes to care for patients. Often the team has never had the time to review these processes. This lack of knowledge often leads to waste, unreliability, and lack of insight into individual contributions to the overall delivery of care. Different views and perspectives emerge when the team creates flowcharts of work activities. Consensus and appreciation of each member’s contribution to the microsystem builds team dynamics. |
| Patterns | Patterns exist providing hints about the culture, communication, and relationships in the microsystem. These patterns are often not explicitly studied or noticed. Considerations include the nature of relationships, structures for collaboration, involvement of patients and carers, and the visibility of metrics about performance to the care team. |
The understanding that emerges from using the 5Ps is important to the interprofessional improvement team in generating ideas for improvement work. These ideas can be tested using the Institute for Healthcare Improvement (IHI) model for plan-do-study-act (PDSA) cycles.Reference Langley, Moen and Nolan7 Successful ideas can be supported by the SDSA process, which standardises the redesigned process in daily work using repeated testing and measurement cycles.
One team at Sheffield Teaching Hospitals NHS Foundation Trust used the 5Ps approach in seeking to address pressing issues around growing patient numbers while improving quality in the care of people with cystic fibrosis (CF).Reference Godfrey, Foster and Johnson8 Following a period of the ‘work before the work’ – which involved securing senior sponsorship, clarifying overall objectives, and agreeing on expectations – the team completed the 5Ps framework to understand their service more deeply (Table 2).
Table 2 Sheffield cystic fibrosis 5Ps
| Purpose | The purpose of the microsystem is to allow people with CF to live as normal a life as possible. |
| Patients | Patients find it hard to stick to treatment plans because they are human beings. |
| Patients self-manage for 99.99% of the year but this is not supported in a systematic way. | |
| Discussing adherence can make patients feel guilty and uncomfortable, and patients are often not willing to talk about the complexity of following their treatment plan because clinic processes are slow, and patients wait long periods before they are seen. | |
| Professionals | The healthcare team has never been taught how to build habits and support behaviour change. |
| The multidisciplinary team fails to adhere to health advice about weight control and exercise. | |
| Processes | When patients come to the clinic, adherence will be invisible because patients can’t remember how much treatment they have taken. There is a need to make the invisible visible. |
| If it can’t be measured, it can’t be managed. | |
| CF care is practised without accurate adherence data and, as a result, care can be inappropriate and ineffective. | |
| Patterns | People with CF are often admitted to hospital for highly disruptive unscheduled rescue therapy. |
| Rescue therapy is often necessary because patients find it hard to take preventative therapy. | |
| Data show that the median amount of preventive inhaled therapy taken is 36% and even lower if patient characteristics are used to estimate treatment requirements.Reference Daniels, Goodacre and Sutton9 | |
| CF care involves a dynamic balance between disruptive rescue and strategic prevention, and this balance could be influenced by the clinical team. |
The 5Ps exercise developed understanding consensus and ownership within the CF team as they began to settle on themes for improvement (Box 2).
Box 2 CF themes for improvement
1. Clinic flow: In order to support behaviour change in patients, the team needed to redesign the clinic system to eliminate waiting as much as possible. The team used the microsystem improvement ramp to understand the clinic process, aiming to reduce waiting and improve flow. Following a series of PDSA cycles, the team reduced the mean clinic waiting time from 40 to 8 minutes.
2. Capacity: The team needed outpatient capacity to deal with increasing numbers of patients and to allow time for complex interventions. The team tested several ideas, including introducing nurse-led clinics, standardising follow-up rules, and streaming clinics to best direct the right capacity to the patients who needed it.
3. Adherence: This became the metric that matters. The team needed to make the invisible visible, so they began testing the use of interventions, such as motivational interviewing and the ‘chipping’ of home-used nebulisers to understand motivations, as well as referring to the actual patient adherence data. Later they developed an online platform, Cystic Fibrosis Health Hub, which has been used in a national programme and a research programme to support improved patient outcomes and adherence.
3.4 Team Coaching and Flow Coaching
Microsystem improvement requires commitment, ownership, and time from leadership and the interprofessional improvement team. Engagement, willingness to be involved, and a clear understanding of the improvement process from stakeholders are prerequisites. Leaders cannot command performance, but they can create the conditions to support staff time and space to work on improvement.
Improving quality in healthcare can be challenging and complex, requiring more than the application of techno-mechanical tools and processes used in Lean, Six Sigma, PDSA cycles, or data collection. Microsystem improvement leaders recognise that making improvements in healthcare is as much about changing behaviours and improving teamwork and relationships as it is about redesigning systems and processes. To support these improvements, the microsystem approach may use team coaches who are trained in sociocultural skills, effective meeting skills, and navigating conflict to enable a productive relationship-centred conversation.
Evidence from research shows that having a team coach to help and support improvement work can increase the likelihood of improvement success and team dynamics.Reference Godfrey10 The team coaching model used in the clinical microsystems improvement approach is based on data from research summarising factors found important to successful improvement experiences,Reference Godfrey10 Donald Schön’s reflective practice perspective, Hackman and Wageman’s theory of team coaching, and Edgar Schein’s principles of helping, humble inquiry, and humble leadership.Reference Nelson, Batalden and Godfrey3, Reference Schön11–Reference Schein15 The model, shown in Figure 2, is intended to support people to reflect on experience to learn, and provides a way of guiding, reinforcing, and encouraging busy interprofessional frontline improvement teams. The model also intentionally includes a framework for developing improvement capability for everyone at the frontline of care.
Flow coaching is an adaptation of these elements to support mesosystem improvement work. In the mesosystem approach,Reference Crisp, Watt, Jones, Amevenu and Warburton4 which brings together interprofessional staff with patients and families across the care pathway (multiple microsystems), into a big room, co-coaching is normally used, where a coach (often a clinician from within the pathway) pairs with an external coach. The pair supports each other through the complexities of pathway redesign. Both coaches offer improvement knowledge and skills, with the internal clinical coach bringing experience and knowledge of the pathway, and the external coach bringing impartiality and challenge.
1. Work before the work: Aim to ensure clarity of improvement goals, expectations, and leadership support.
2. Pre-phase: Aim to help the team coach and improvement team begin to understand their system context, and for the team coach to meet the team where they are at.
3. Action phase: Aim to coach the improvement team through the microsystem improvement ramp.
4. Transition phase: Aim to coach the improvement team to reflect on the improvement process, assess what has been learnt, celebrate success, and continue independent improvement activities.
3.5 Flow Coaching for Mesosystems
Flow coaching focuses on the mesosystem and involves coaching multiple microsystems, each with different cultures, that form the mesosystem.Reference Godfrey, Foster and Johnson8 As described previously, the mesosystem is co-coached by two Flow coaches, one with insider clinical expertise and the other external to the care pathway. The microsystems are studied and assessed for their individual and collective contributions to the mesosystem care pathway, using a modified 5Ps structure called the 5Vs.
A key feature of this approach is the physical or virtual big room, where the assessment and improvement work of the mesosystem is coordinated by two Flow improvement coaches. The Flow coaches engage multidisciplinary colleagues, as well as patients, to learn different perspectives about the pathway. The big room members typically meet for an hour every week on a continuous basis coached by the Flow coaches.Reference Crisp, Watt, Jones, Amevenu and Warburton4
Multidisciplinary teams and their patients share data, experiences, stories, and evidence openly, and plan collectively to create new or improved ways of providing care, following the Flow roadmap. The Flow roadmap (Figure 3) modifies the same conceptual approach and structure as the microsystem improvement ramp, with some changes made to account for the increased complexity of mesosystems as compared with microsystems.
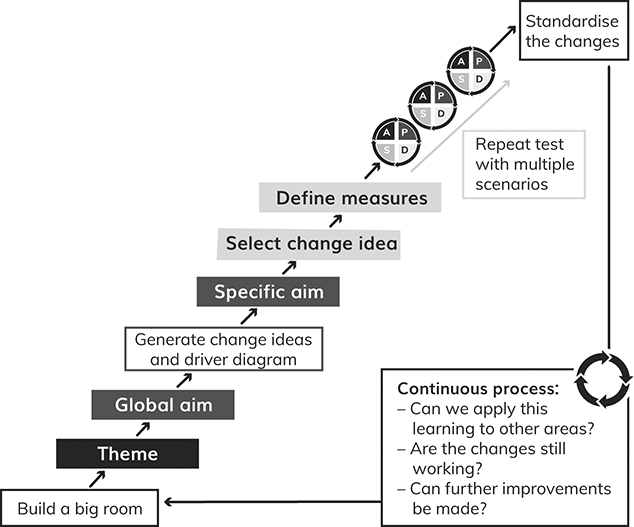
Figure 3 The Flow roadmap
Instead of the 5Ps, we now have the 5Vs:
Value: What do patients define as the value they need from the care pathway? How well is this delivered? What does patient experience tell us about the system?
inVolve: What do the multidisciplinary teams who work along the pathway consider to be what works and what doesn’t in delivering quality care?
Visualisation: Patient shadowing, value stream mapping, spaghetti diagrams, and other visualisation tools are used to understand the pathway more deeply.
eVidence: Data are used to understand the demand, flow, waiting, and waste inherent in the pathway.
Vision: What would the vision of ideal care look like?
An example of the big room mesosystem approach in action can be seen in a project led by Imperial College NHS Foundation Trust to improve sepsis management. This included an Electronic Patient Record (EPR) alert for sepsis, and processes to give information on the treatment required and trigger care to occur quickly and effectively.Reference Crisp, Watt, Jones, Amevenu and Warburton4
A wide-ranging multidisciplinary team was involved in the work of the sepsis big room. Meeting weekly, staff came together in an hour-long coached session to discuss improvements and learning. They used the Flow roadmap (Figure 3) and piloted the alert at the acute medical unit at St Mary’s Hospital in London. The pilot revealed that several improvements were needed: not just in technical aspects of the alert, but also a range of issues about effective communication between staff and departments. The big room engaged the team in testing changes to improve the alert system, then expanded the changes out to the emergency departments at St Mary’s Hospital, Charing Cross Hospital, and the haematology service. The big room provided a regular, structured, supportive forum to enable collaboration and shared structured problem-solving during these multiple interventions.Reference Crisp, Watt, Jones, Amevenu and Warburton4
The EPR alert has made a significant impact. The team initially improved the identification of sepsis and increased patients coded with a diagnosis of sepsis by 85% – that is, from an average of 26 cases per week to 48 cases per week. They then implemented interventions that decreased sepsis mortality by 23%. Retrospective analysis of the introduction of the alert was associated with:
lower odds of mortality;
lower odds of long hospital stay;
increased odds of receiving timely antibiotics within 60 minutes.
In short, more patients were correctly diagnosed with sepsis and, of these, more of them survived sepsis. Research evidence showed that the effectiveness of EPR alerts is mixed. An alert system in the EPR alone might not have led to such a level of improved outcomes. At Imperial, the introduction of the alert was a driver for Flow and team coaching improvement initiatives to make sure that there were effective treatment responses to the alert.Reference Crisp, Watt, Jones, Amevenu and Warburton4
4 Critiques of the Microsystems Approach
Since its early development and the generation of evidence on characteristics of high-performing microsystems at Dartmouth,Reference Nelson, Batalden and Huber2 the adoption of the microsystems approach has spread within and beyond the United States over the past two decades. In Europe, this has also been supported by programme initiatives to spread the approach to build frontline capability through team coaching at both the microsystem level (Sheffield Microsystem Coaching Academy (MCA)) and mesosystem level (Flow Coaching Academy). The evidence base across diverse care settings on the effectiveness of the microsystems approach, its key strengths and limitations, and the conditions needed for success continues to grow. Overall, the current evidence points to a role for microsystems within the healthcare improvement landscape as an approach focused on building frontline, data-driven team capability for care and service redesign, and its potential to deliver improvements to processes and patient outcomes.
However, the evidence on the effectiveness of the approach is both complex and emergent, and there is a need for further ongoing, rigorous research and evaluation of the approach to accompany further spread across international contexts, informing comparisons of its relative benefits and limits in relation to other improvement approaches. Current evidence is drawn from a range of sources, with varying methodological approaches and rigour. There are inherent challenges to evaluating microsystems as a complex intervention, where effectiveness needs to be understood as a product of interaction between the approach and its organisational and policy context.Reference Dixon-Woods and Martin16 Perhaps, rather than asking ‘does the microsystems approach work?’, we need to ask what works, how, when, and for whom. By implication, effectiveness is not simply about the application of a specific approach but about ‘enabling a receptive institutional context so that the approach is useful and appropriate’.Reference Williams, Dickinson, Robinson and Allen17
Appropriate and feasible study designs for evaluating this kind of complex interventionReference Dixon-Woods and Martin16 are not always available, giving rise to challenges around rigour, quality, and interpretation of the available evidence, not least in capturing and attributing any impacts – positive, negative, and unintended – to the approach.Reference Broeks, Iakovidou and Pollard18, Reference Cote, Beogo and Abasse19, 20 Variations in fidelity, implementation, specific focus in practice, and use of team coachingReference Williams, Dickinson, Robinson and Allen17, Reference Broeks, Iakovidou and Pollard18 compound the challenges. For those adopting and evaluating the microsystems approach, the complexities of identifying, operationalising, and robustly measuring appropriate process and outcome measures to assess effectiveness are further compounded by challenges associated with availability, capability, and capacity around data in healthcare contexts.
4.1 Evidence from Studies of Microsystems
The current evidence base on the microsystems approach spans what Portela et al. (2015) refer to as the ‘practical’ (aimed at producing change) and ‘scientific’ (aimed at producing new knowledge), loosely differentiated by primary aims and design of the work.Reference Portela, Pronovost, Woodcock, Carter and Dixon-Woods26 The distinction between this practical and scientific evidence is somewhat blurred in reality – microsystems improvement projects are often applied and self-evaluating, but can contribute valuable evidence to wider improvement communities. Furthermore, independent evaluations can be embedded within improvement initiatives and generate new insights that contribute formatively to the ongoing development of microsystem20 and mesosystem interventions.Reference Broeks, Iakovidou and Pollard18
First, self-evaluation of microsystems through improvement projects and networks has a primary aim to support improvement work itself, including sharing lessons with others adopting the approach.Reference Nelson, Batalden and Huber2, 20, Reference Woodcock, Liberati and Dixon-Woods21 The Sheffield MCA published case studies on its website for this purpose.22 More broadly, among those employing the team coaching model, a rich evidence base is being generated and shared throughout a network of international collaborating partners including Sheffield MCA (UK), The Microsystem Academy (USA), Jönköping Academy for Improvement of Health and Welfare (Sweden), and Qulturum Jönköping (Sweden). This highlights potential benefits for improved healthcare quality in addition to deepening understanding of the challenges and conditions needed for success to directly inform organisational decision-making and policy-makers.
Second, independent evaluationsReference Broeks, Iakovidou and Pollard18, 20 and research across diverse clinical domains have sought to contribute to building a generalisable, scientific evidence base through robust study designs to inform future practice and decision-making around microsystems. Gerrish et al. Reference Gerrish, Keen and Palfreyman23 evaluated a clinical microsystems improvement initiative used to promote integrated care across a falls pathway, and Helou et al. Reference el Helou, Samiee-Zafarghandy and Fusch24 examined the introduction of microsystems within neonatal intensive care. Together, this growing evidence base advances understandings of what works, who for, and within what circumstances.Reference Pawson and Tilley25 They highlight key conditions for success and the potential of the approach to deliver enhanced care processes and outcomes.
Multi-site studies offer strength in capturing the importance of context. Williams et al. Reference Williams, Dickinson, Robinson and Allen17 were commissioned to undertake a mixed-method evaluation of 100 microsystems in the NHS that had adopted the improvement approach in areas as diverse as reducing the length of hospital stay, DNA levels in surgery, staff sickness and turnover rates, and inefficient prescribing behaviour. Overall, the evidence suggested that microsystems did positively impact quality and system redesign through enhanced team engagement, morale, commitment, clarity of purpose, and – to a lesser extent – a shift towards a culture of improvement, signalling the integrating potential of microsystems through an increased number of empowered improvers. Organisational conditions were key to these successes, including leadership support, institutional framing aligned to a democratic, capability-building approach (as opposed to a top-down, target-driven approach), and resource provision. Evidence of the impact on patient outcomes was less clear, with a lack of routine service data and robust outcome measurement, the challenges of attributing impacts, and a preponderance of qualitative measures and staff-reported benefits highlighting the need for investment and infrastructure for data capabilities to support the future legitimacy of microsystems.
4.2 The Complexities of Analysing and Evaluating the Evidence Base
The range of studies across diverse local and national contexts makes synthesising the evidence complex. Cote et al. Reference Cote, Beogo and Abasse19 noted the absence of a robust, systematic analysis of the evidence base, where ‘despite the widespread implementation of the microsystems approach … the published evaluations of the microsystems performance in terms of tangible results remains unclear’. Addressing this gap, they critically appraised and synthesised the best available evidence across databases on the current implementation and effectiveness of microsystems, aligned to IOM’s six dimensions of safety, effectiveness, patient-centredness, timeliness, efficiency, and equity.Reference Gerrish, Keen and Palfreyman23 This highlighted the challenges of aggregating and synthesising evidence on microsystems, which included different study designs, varying degrees of rigour, inconsistency of quantitative outcome measures used, some inherent publication bias, and the dominance of United States and Dartmouth-affiliated studies (27 and 11 studies respectively from a total of 38 papers meeting inclusion criteria).
Despite these issues, Cote et al. Reference Cote, Beogo and Abasse19 note some evidence pointing to the effectiveness of the microsystem approach, emphasising the importance given to enhancing understanding, operational processes, and care quality through healthcare system redesign at the frontline as a unique feature. The approach promotes an interdisciplinary, patient-centred method that builds improvement skills and capability, improves care processes, increases patient and staff satisfaction, and may lead to improved patient outcomes (such as reduced length of hospital stay and infections). Overall, ‘the implementation of microsystems helped to provide safe, effective, patient-centred care that is timely, equitable, integrated, and efficient’.Reference Cote, Beogo and Abasse19 However, given the complex picture and inherent role of context, the authors caution that ‘despite the transcending merit of the microsystems approach … efforts still need to be made to legitimise the approach in various healthcare settings worldwide’,Reference Cote, Beogo and Abasse19 suggesting the evidence base does not consistently demonstrate that the approach succeeds everywhere, due to a variety of complex contextual factors.
Some evaluations have also examined programme initiatives aimed at training coaches to enhance team capability at the frontline through a microsystem approach for improved patient outcomes. Through an independent mixed-method, formative, and summative evaluation, Gerrish et al. 23 evaluated the Sheffield MCA as a training entity for enhancing capability against seven dimensions of success (delivery, capability and capacity development, impact, cultural change, organisational ownership, sustainability, spread, and return on investment) in addition to assessing its impact across seven case study microsystems. This study found that the MCA achieved a high level of success in developing coaches and in sharing learning, but there was a mixed picture in terms of the impact on patient outcomes – on the one hand, a number of microsystems were leading to measurable improvements in service delivery, efficiency savings, and patient experience, but despite being an inherent and central part of a microsystem approach, the involvement of patients and carers in improvement was underdeveloped, with comparatively few microsystems involving patients directly.
Echoing the early work of Nelson et al. Reference Nelson, Batalden and Huber2 and Williams et al.,Reference Williams, Dickinson, Robinson and Allen17 the evaluation of the Sheffield MCA gave rich insights into the challenges faced and the organisational conditions influencing success, including leadership support, time, and resource to support the sustainable engagement of coaches and teams, alignment to organisational strategic objectives, the ability to demonstrate positive outcomes to secure buy-in, and the creation of a conducive climate for improvement and microsystems through broader initiatives. Overall, this work emphasises the critical need to consider and invest in creating the conditions to support effective microsystems initiatives.
Broeks et al. Reference Broeks, Iakovidou and Pollard18 independently evaluated the initial three-year phase of the innovative Health Foundation’s Improving Flow Programme. This programme applied microsystems principles (combining team co-coaching and improvement research) to the pathway-level mesosystem to improve patient flow. It did this by training a network of coaches and establishing Flow coaching academies nationally – in a social franchising model of spread – to build system-level, frontline improvement capability across the NHS. Findings align with the wider evidence, showing an emerging credible model to deliver at scale and effectiveness in enhancing team factors of capability, satisfaction, confidence, communications, ownership, ideas sharing, flattened hierarchies, and culture, with a more mixed, emergent picture on measurable patient outcomes. At the time of the evaluation (and noting that evidence continues to emerge), while there was some clear evidence of demonstrable improvements on patient outcome measures in some pathways (see Section 3.5), the qualitative evidence overall outstripped systematic, and quantitative evidence. Issues with the availability of appropriate, rigorous process, and outcome measures, coupled with capability and capacity issues for undertaking complex analysis, meant that attributing outcomes to improvement activities undertaken and understanding the impact of local context was sometimes challenging. The significance of a conducive organisational environment – including leadership support, resource, and organisational alignment to a democratised, capability-building approach to healthcare improvement – was again clear, as was the relative absence of patient involvement, despite being integral to the design of the methodology.
It has also proven challenging to assess the relative cost-benefits of a microsystems approach in practice relative to other healthcare improvement initiatives in specific settings, not least when there is an absence of robust economic evaluations of implementing and sustaining the approach.Reference Broeks, Iakovidou and Pollard18 While there is some evidence that microsystems can deliver efficiency savings (see Section 4.1), assessing the economic cost-benefits is a complex but often essential element of securing sustained strategic investment and showing ‘return on investment’ in relation to other improvement approaches. This is complex, needing a system-level view and a recognition that efficiency savings are not always an appropriate or desirable indicator of effectiveness, given broader, multifaceted understandings of quality in complex improvement initiatives.Reference Portela, Pronovost, Woodcock, Carter and Dixon-Woods26
Overall, the microsystems approach might be seen as a promising but still emergent approach to quality improvement, with variable but growing evidence of the impact on patient experience and outcomes.
5 Key Strengths and Limitations of the Microsystems Approach
The current collective evidence on the microsystems approach points to key strengths, key limitations, and the organisational conditions necessary for success, as the basis of recommendations for practitioners, leaders, and policy-makers to support the approach in practice. Future research can further enhance the evidence base and success of the approach in diverse contexts.
The microsystems approach occupies a distinct place in the healthcare improvement landscape. It has a democratic, strengths-based focus on building frontline improvement capability alongside supportive structures and workplace routines, and on the socio-behavioural aspects of change, not just technocratic improvement.Reference Godfrey, Foster and Johnson8, Reference Williams, Dickinson, Robinson and Allen17 The approach has its origins in improvement research and data-led methods. It emphasises obtaining rigorous, timely and accessible information to enhance understanding and service redesign around dimensions of the microsystem – the 5Ps of purpose, patients, professionals, process, and patterns – and developing evidence of improvements using the structured improvement ramp. The team coaching model combines this rigour with human dimensions of change, with the aim of nurturing interdisciplinarity, team cohesion, enhanced communication, knowledge-sharing, and flattened hierarchies, all of which are associated with improved care processes and outcomes.
The microsystems approach targets the IOM’s six dimensions of performance: safety, effectiveness, patient-centredness, timeliness, efficiency, and equity. A focus on the smallest unit of care delivery fosters a better understanding of services from the patient perspective in frontline teams,Reference Nelson, Batalden and Godfrey3 creating opportunities for dialogue and for the direct involvement of patients and carers in service redesign. Rather than top-down, externally driven improvement initiatives, the microsystem approach sees the development, expertise, and knowledge of staff as the most important asset of these systems. The evidence shows that the focus on frontline ownership of improvement initiatives can increase staff engagement, morale, and commitment to improvement in addition to improving team communication, knowledge-sharing, and relational processes.Reference Williams, Dickinson, Robinson and Allen17, Reference Cote, Beogo and Abasse19 The creation of sustained spaces for determining shared meanings, relationship-building, and problem-solving grounded in practice through an interdisciplinary, inclusive commitment to flattening hierarchies is a distinctive strength of the microsystems approach.Reference Liberati, Gorli and Scaratii27 The breadth of settings in which a microsystems approach has been adopted suggests that it offers a flexible, adaptable framework to improvement when supported by conducive leadership support and organisational conditions. It is scalable to the mesosystem care pathway level, which aligns with policy emphases on a whole systems approach to healthcare and offers to fulfil a need for healthcare improvement that can drive system-level transformation.Reference Broeks, Iakovidou and Pollard18
An emphasis on sustainability through team capability is inherent to the approach, with the potential to embed routine practices and build a culture of improvement, enhancing resilience in the face of external challenges. These strengths align with Senge’s Reference Senge28 model of the ‘learning organisation’ – an ideal environment that fosters embedded, normalised continuous learning, improvement, and innovation, through systems thinking, the questioning of assumptions, a collective team vision and common goals, and facilitative leadership (coach rather than cop) focussed on creating conditions versus top-down mandates. This takes a holistic view of cultures for improvement as emergent from, responsive to, and inextricably linked to, the organisational conditions in which employees solve problems, adapt, and learn from experience, rather than a separate variable to be managed.Reference Schein29 The evidence highlights the way in which conducive organisational conditions (or consistent cues) are essential to successful microsystem processes and outcomes.Reference Williams, Dickinson, Robinson and Allen17–20
Dixon-Woods and Martin Reference Dixon-Woods and Martin16 stress that too many healthcare improvement approaches are seen as ‘magic bullets’ that can lead to improvement in any situation and context, failing to pool resources or develop collective solutions. In contrast, the development of the microsystems approach has been supported by formal and experiential evidence and – particularly when supported through programme initiatives of training academies and networks of microsystems20 and mesosystemsReference Broeks, Iakovidou and Pollard18 – adoption is supported by a pooling of resources and guidance for practical implementation choices that reinforce fidelity, encourage sensitivity to unintended adverse impacts, and adaptation to local contexts.Reference Broeks, Iakovidou and Pollard18
Nonetheless, further research is needed on microsystems in diverse care settings internationally,Reference Cote, Beogo and Abasse19 using rigorous study designs with appropriate processes and outcomes measures capable of capturing the role of organisational and policy factors in shaping the implementation and outcomes of the approach. There is also a need to better understand the ‘black box’ of implementation across contexts, highlighting issues of fidelity to the approach, and strengthening explanatory power regarding those elements of the approach that are critical to success.Reference Broeks, Iakovidou and Pollard18 Together, such work would further inform practitioners, leadership teams, and policymakers about the conditions needed for success. Furthermore, it is important to be able to holistically assess the cost-benefits of a microsystems approach – including robust economic assessment – to compare with other healthcare improvement approaches in particular settings and improvement challenges.
5.1 Key Limitations and Recommendations for Success
Evidencing effectiveness is key to the legitimacy of the microsystems approach and securing engagement, leadership support, strategic investment, and its sustainability. While the evidence on the effectiveness of microsystems to impact measurable patient outcomes is growing, it remains mixed both in terms of study design quality and in robust demonstrations of effectiveness. In common with studies of other complex improvement interventions,Reference Woodcock, Liberati and Dixon-Woods21 lack of appropriate data availability, capability, and infrastructure are significant problems, impacting on the ability to evaluate and attribute outcomes to microsystem interventions. Organisational investment in data analytics and infrastructure to support microsystems initiatives is recommended, in addition to dedicated resources to support rigorous evaluation.
Second, although the microsystems approach places the patient at the centre of system redesign and improvement, in practice it is done in different ways, with relatively few microsystems involving patients directly in improvement work.Reference Williams, Dickinson, Robinson and Allen17, Reference Broeks, Iakovidou and Pollard18, Reference Cote, Beogo and Abasse19 Innovative examples of engaging patients in improvement work include the Cystic Fibrosis Foundation (CFF) in the United States, where for almost two decades, any improvement team has been expected to include patients with CF or their family members.Reference Kelly30 Exemplars like the CFF can provide guidance and recommendations to enhance patient and family involvement to promote further development of creative patient and public involvement and mechanisms to collaboratively assess with patients the approaches taken.Reference Williams, Dickinson, Robinson and Allen17, 20 A key area for future research is patient and carer involvement in microsystems improvement, with comparative and evaluation studies of innovative approaches to further inform the development of recommendations and share best practices.Reference Cote, Beogo and Abasse19 This is essential if the microsystems’ approach is to fully deliver on its promise of patient-centred improvement.
A further challenge lies in the need for a conducive organisational environment.Reference Williams, Dickinson, Robinson and Allen17, Reference Cote, Beogo and Abasse19 Leadership support at all levels is necessary for the microsystems approach to work – including allocating time and resources for participating staff, advocating, making successes visible, and framing the approach as capability-building rather than a top-down mechanism to achieve targets. Leadership support and resources need to extend beyond initial phases for benefits to be realised, but expectations for earlier demonstrations of positive impact in the face of wider organisational strategic pressures and pressures on teams may become overwhelming. Organisations that embed clinical microsystem improvement within their HR departments and set expectations within job descriptions are more likely to have sustainable habits and systems.Reference Broeks, Iakovidou and Pollard18, 20 Delivering on these requirements for long-term leadership and infrastructural support is not easy, not least due to the strategic, operational, and financial pressures, the competing priorities facing organisations, and the amount of time the approach can take to deliver tangible change. This represents a potential limit on which settings a microsystems approach is likely to be appropriate for and the sort of improvement challenges it can successfully address.
6 Conclusions
The evidence base on microsystems as an improvement approach continues to emerge. While some evaluations show the potential of the method to deliver measurable patient benefitsReference Cote, Beogo and Abasse19, 20 and to promote staff engagement, collaboration, and satisfaction due to the focus on the socio-behavioural aspects of change,Reference Kelly30, Reference Zimmerman, Lindberg and Plsek31 further robust studies are required to address the current gaps in understanding to inform future practice.
As healthcare systems change, with new technologies and models of care emerging, further development of the mesosystem or care pathway improvement approach will be essential. People travel through multiple microsystems on their healthcare journey and the effectiveness of these mesosystems will determine the overall quality of their care. With increased complexity, further advancing and modifying the microsystems approach to mesosystems is needed. This will support healthcare providers to ensure that their systems and resources are organised in the optimal way to deliver optimal quality care for their populations.Reference Godfrey, Foster and Johnson8
7 Further Reading
The Microsystem Academy (TMA), United States, https://clinicalmicrosystem.org/ 32 – formerly the Dartmouth Institute Microsystem Academy at The Dartmouth Institute for Health Policy and Clinical Practice until 2020, TMA enhances and develops individual and team capabilities for research, practice, improvement, and innovation. TMA generates ongoing evidence through its team coaching action learning and research programme, shared and developed via its international network of partners (in Europe, Canada, and the United States), its network of learning events, and its website of resources and publications.
Microsystems Coaching Academy (MCA), Sheffield Teaching Hospitals NHS Foundation Trust, UK, https://www.sheffieldmca.org.uk/22 – Sheffield MCA combines improvement research and team coaching to build continuous improvement capability into the workforce and service redesign for patient benefit. Representing a large community of practice with international partners, MCA shares lessons and an evidence base of success.
Flow Coaching Academy, Sheffield Teaching Hospitals NHS Foundation Trust, UK, https://flowcoaching.academy33 – Flow Coaching Academy (FCA) (Health Foundation-funded programme established in 2016) trained improvement coaches to build team capability and improve patient outcomes at the mesosystem level, sharing learning and evidence through a network of Flow Coaching Academies.
Jönköping Academy for Improvement of Health and Welfare, Jönköping University, Sweden, https://ju.se/center/ja/en.html33 – a collaboration platform for Jönköping University, County Council of Jönköping and Jönköping County, this academy functions as a national and international forum for research and education in improving knowledge and leadership within healthcare and social care with practitioners, decision-makers, researchers, and students.
Qulturum, Region Jönköping County, Sweden, https://www.rjl.se/qulturum/_in-english/about-qulturum/34 – Qulturum is a centre for development of improvement knowledge and innovation in healthcare and improvement unit using a clinical microsystem improvement approach and sharing new insights. Qulturum hosts the annual Microsystem Festival to share microsystem learning across the international microsystems’ community.
Nelson et al.Reference Nelson, Batalden and Godfrey3 – this textbook captures the foundational theory of clinical microsystems in healthcare.
Godfrey et al.Reference Godfrey, Foster and Johnson8 – this textbook demonstrates the utility of microsystem application in health systems around the world and expands the theory to the mesosystem including a new action guide.
Crisp et al.Reference Crisp, Watt, Jones, Amevenu and Warburton4 – this text reviews the learning from the RAND evaluation of the Flow Coaching Academy summarising how the FCA approach was planned, designed, and implemented.
All authors have contributed equally to the writing of the original draft, subsequent review and editing. All authors have approved the final version.
Conflicts of Interest
None.
Acknowledgements
We thank the peer reviewers for their insightful comments and recommendations to improve the Element. A list of peer reviewers is published at www.cambridge.org/IQ-peer-reviewers.
Funding
This Element was funded by THIS Institute (The Healthcare Improvement Studies Institute. www.thisinstitute.cam.ac.uk). THIS Institute is strengthening the evidence base for improving the quality and safety of healthcare. THIS Institute is supported by a grant to the University of Cambridge from the Health Foundation – an independent charity committed to bringing about better health and healthcare for people in the UK.
About the Authors
Steve Harrison is Deputy Director of Organisational Development at Sheffield Teaching Hospitals (STH) NHS FT, with experience working in organisational development and quality improvement. He led the Microsystem Coaching Academy and Flow Coaching Academy programmes and has collaborated on initiatives at a local, national and international level.
Rachael Finn is Dean of Sheffield University Management School. Her research lies within the field of organisation studies, with a particular focus on the realities of health and social care organisation. She has a particular interest in critical management and qualitative methodologies, including discursive perspectives on organisational life.
Dr Marjorie M. Godfrey is a leading expert in quality improvement and leadership in healthcare. She has helped organisations and healthcare professionals worldwide to enhance care quality and co-founded impactful institutes at Dartmouth and the University of New Hampshire. She is a bestselling author, promoting applied microsystem theory and person-centred practice with multidisciplinary teams.
The online version of this work is published under a Creative Commons licence called CC-BY-NC-ND 4.0 (https://creativecommons.org/licenses/by-nc-nd/4.0). It means that you’re free to reuse this work. In fact, we encourage it. We just ask that you acknowledge THIS Institute as the creator, you don’t distribute a modified version without our permission, and you don’t sell it or use it for any activity that generates revenue without our permission. Ultimately, we want our work to have impact. So if you’ve got a use in mind but you’re not sure it’s allowed, just ask us at [email protected].
The printed version is subject to statutory exceptions and to the provisions of relevant licensing agreements, so you will need written permission from Cambridge University Press to reproduce any part of it.
All versions of this work may contain content reproduced under licence from third parties. You must obtain permission to reproduce this content from these third parties directly.
Editors-in-Chief
Mary Dixon-Woods
THIS Institute (The Healthcare Improvement Studies Institute)
Mary is Director of THIS Institute and is the Health Foundation Professor of Healthcare Improvement Studies in the Department of Public Health and Primary Care at the University of Cambridge. Mary leads a programme of research focused on healthcare improvement, healthcare ethics, and methodological innovation in studying healthcare.
Graham Martin
THIS Institute (The Healthcare Improvement Studies Institute)
Graham is Director of Research at THIS Institute, leading applied research programmes and contributing to the institute’s strategy and development. His research interests are in the organisation and delivery of healthcare, and particularly the role of professionals, managers, and patients and the public in efforts at organisational change.
Executive Editor
Katrina Brown
THIS Institute (The Healthcare Improvement Studies Institute)
Katrina was Communications Manager at THIS Institute, providing editorial expertise to maximise the impact of THIS Institute’s research findings. She managed the project to produce the series until 2023.
Editorial Team
Sonja Marjanovic
RAND Europe
Sonja is Director of RAND Europe’s healthcare innovation, industry, and policy research. Her work provides decision-makers with evidence and insights to support innovation and improvement in healthcare systems, and to support the translation of innovation into societal benefits for healthcare services and population health.
Tom Ling
RAND Europe
Tom is Head of Evaluation at RAND Europe and President of the European Evaluation Society, leading evaluations and applied research focused on the key challenges facing health services. His current health portfolio includes evaluations of the innovation landscape, quality improvement, communities of practice, patient flow, and service transformation.
Ellen Perry
THIS Institute (The Healthcare Improvement Studies Institute)
Ellen supported the production of the series during 2020–21.
Gemma Petley
THIS Institute (The Healthcare Improvement Studies Institute)
Gemma is Senior Communications and Editorial Manager at THIS Institute, responsible for overseeing the production and maximising the impact of the series.
Claire Dipple
THIS Institute (The Healthcare Improvement Studies Institute)
Claire is Editorial Project Manager at THIS Institute, responsible for editing and project managing the series.
About the Series
The past decade has seen enormous growth in both activity and research on improvement in healthcare. This series offers a comprehensive and authoritative set of overviews of the different improvement approaches available, exploring the thinking behind them, examining evidence for each approach, and identifying areas of debate.