Maternal and child health
Maternal and child health (MCH) refers to the life course involving women before and during pregnancy up to immediately after childbirth and children to their fifth birthday( 1 ). According to the Save the Children's 16th annual Mothers’ index that assessed the wellbeing of mothers and children in 179 countries, the eleven countries that performed poorly in all indicators were all from developing countries in Africa, except for Haiti. On average one in every thirty women dies from pregnancy-related causes and one in every eight children dies before their fifth birthday( 2 ).
The reproductive system consists of interdependent and critical stages that collectively determine the survival of the mother during childbirth, the pregnancy outcome and the health of the newborn child for the first 1000 d( Reference Abu-Saad and Fraser 3 ). This interdependency underscores the importance of appropriate and timely interventions during pregnancy, even starting pre-conception, if possible and systematically continue through pregnancy, childbirth and neonatal to 1000 d at the minimum( Reference Lassi, Mansoor and Salam 4 , 5 ).
Maternal health
The nutritional status of women at the time of conception and during pregnancy are major determinants of the pregnancy outcome as evidenced by the health, growth and development of the fetus and the newborn( 5 , Reference Black, Victora and Walker 6 ). For example, evidence indicates that placental and fetal development is most vulnerable during the period of rapid placental development during the first trimester( Reference Abu-Saad and Fraser 3 ). Neural tube defects, cretinism, intrauterine growth restriction and preterm birth are well-known adverse outcomes of general and specific nutrient deficiencies, such as folate, iodine, iron, calcium, magnesium, phosphorous, potassium, sodium, sulphur, zinc, vitamins B1, B2, B3, B5 and D, that are related to maternal nutritional status during and before conception, thus underscoring the importance of pre-conception care( Reference Wu, Imhoff-Kunsch and Girard 7 ). In addition to mother's’ survival, undernourished women give birth to smaller infants than well-nourished mothers, an independent risk factor for the survival of the newborn( Reference King 8 ). Low-birth weight infants, in turn, are at a higher risk of death due to infections and asphyxia( Reference Abu-Saad and Fraser 3 ).
In addition to compromised pregnancy outcomes, maternal malnutrition and associated poor health are the direct causes of maternal morbidity and mortality as a result of haemorrhage, infection, high blood pressure and obstructed labour( 1 ). For example, calcium deficiency is a risk factor for hypertensive disorders of pregnancy such as pre-eclampsia, while iron deficiency anaemia may increase the risk of maternal mortality during childbirth( Reference Wu, Imhoff-Kunsch and Girard 7 ). Results from two different meta-analyses proved the efficacy of calcium supplementation for reducing gestational hypertensive disorders in pregnant women at high risk of developing hypertension or with low calcium intakes( Reference Imdad and Bhutta 9 , Reference Hofmeyr, Lawrie and Atallah 10 ). The first meta-analysis showed that calcium supplementation during pregnancy significantly reduced the risk of preeclampsia by 52 %, severe pre-eclampsia by 25 %, incidence of severe pre-eclampsia by 24 % and low birth weight by 15 % in women with high risk of developing hypertension during pregnancy( Reference Imdad and Bhutta 9 ). The second meta-analysis found that there was a 35 % reduction in the risk of gestational hypertension in women at high risk, and those with low calcium intake and a reduction by 20 % in maternal death or severe morbidity for women that received calcium supplementation( Reference Hofmeyr, Lawrie and Atallah 10 ). Evidence indicates that maternal survival is determined by the women's nutritional status. Specifically, maternal short stature and undernutrition are indicators of poor nutritional status during childhood; while iron deficiency is associated with a higher risk of death of the mother at delivery and accounts for at least 20 % of maternal deaths( Reference Black, Victora and Walker 6 ). For example, a study from Nepal found that a low mid-upper arm circumference in early to mid-gestation was associated with risk of maternal death during pregnancy( Reference Christian, Katz and Wu 11 ). Similarly, a study conducted by Merchant, Villar and Kestler identified that maternal short stature increases risk of dystocia (difficult labour), as measured by cephalopelvic disproportion or assisted caesarean deliveries( Reference Merchant, Villar and Kestler 12 ). Also, a meta-analysis carried out by Kozuki et al. in short maternal stature proved that short stature was significantly associated with short-gestational-age, preterm appropriate-for-gestational-age and preterm short-gestational age in low and middle income countries( Reference Kozuki, Katz and Lee 13 ).
Neonatal and child health
The Millennium Development Goals (MDG) Report in 2015 showed that for the MDG 4, the number of deaths of children under 5 has declined from 12·7 million in 1990 to almost 6 million in 2015 globally( 14 ). However, the probability of a newborn dying during the first 28 d of life is still high compared with the mortality rate for children between age 1 month and 5 years; 45 % of total deaths in 2015, 5 % more than in 2000( 15 ). Nearly 4 million newborns die (40 % of under 5 deaths) within 28 d of birth( Reference Kerber, de Graft-Johnson and Bhutta 16 ).
For the children that survive the first 28 d, being able to survive and thrive the first 1000 d requires a concerted effort of a healthy mother, exclusive breastfeeding, a sanitary environment, appropriate complementary food at 6 months and access to preventive healthcare at minimum( 2 ). Although exclusive breastfeeding has proved to save babies from dying of infections, it does not prevent stunting among low-income, overworked and malnourished mothers who might not be able to produce sufficient milk to meet the needs of a 2–6 months old baby. Malnutrition as evidenced by the high rates of stunting, wasting and micronutrient deficiencies is a major threat to MCH, accounting for 35 % of the disease burden in children under 5. This translates into 3·5 million maternal and child deaths for which the underlying cause is undernutrition( Reference Black, Allen and Bhutta 17 ). These findings imply that more dietary assistance is needed for low-income mothers over and above the recommendation to exclusively breastfeed their children. In addition to lack of proper nourishment, impoverished mothers may not have access to clean water or environment and a diverse diet, making it easy for the opportunistic diseases like infections claiming the lives or compromising children's nutritional status( 18 ).
According to the MDG assessment report, the global under-5 mortality rate has significantly dropped by more than half, from ninety to forty-three deaths per 1000 live births between 1990 and 2015( 2 , 14 ). Despite this great achievement, it is noteworthy that about 16 000 children under 5 continue to die every day, and an estimated 5·9 million children die before their fifth birthday and almost half of those deaths take place within the first month of life( 15 ). Evidence indicates that preventable causes such as pneumonia, diarrhoea and malaria accounted for 43 % of the under-5 deaths according to the UNICEF 2015 report( 15 ). Lack of access to effective care and resources at the community level is therefore the underlying cause of these deaths. For example, antibiotics for pneumonia are available to only about 31 % of affected children, and diarrhoea treatment only to 35 %( 19 ). Specifically, for the prevention of pneumonia the Hib vaccine is widely used around the globe except in China and Thailand where they only have access to this vaccine in the private market. According to the Pneumonia & Diarrhoea Progress Report there are still some countries that have an extremely low coverage of this vaccine, including India (20 %), Indonesia (21 %), Somalia (42 %) and Chad (46 %)( 20 ). It is therefore clear that the global advance in child survival has failed to protect many of the world's youngest children from vulnerable situations. If the present trend continues, it will take 10 or more years to reach the global target( 15 ).
Continuum of care
To address these complex and multilevel issues, the Global Business Plan for MDG 4 and 5 recommends use of the continuum of care( Reference Stoltenberg 21 ). Understanding that the health of the mother and child are interrelated, and that the nutritional and health status of the mother affects the health of the child, the goal of the continuum of care is to provide comprehensive seamless and integrated health services for women and their children throughout the life cycle, starting from pre-pregnancy through delivery and the immediate postnatal period to the child's fifth birthday (Fig. 1)( Reference Lawn, Tinker and Munjanja 22 – Reference Tinker, ten Hoope-Bender and Azfar 24 ).
Fig. 1. Continuum of care( Reference Kerber, de Graft-Johnson and Bhutta 16 ).
Similarly, the interventions and delivery of care should be interrelated and mutually supportive and available in all the places that the mothers and children live, play and work starting from the household , community and outpatient or healthcare centres based on the complexity of the care needed( Reference Kerber, de Graft-Johnson and Bhutta 16 ). This approach is cost and time effective, especially in low-income countries where continuum of care is more critical than specialised care; however, it will require more comprehensive training for the healthcare providers with competences ranging from preconception to childhood nutrition and health needs( Reference Tran, Portela and de Bernis 25 ).
Evidence indicates that there is a shortage of health workforce in low-income countries( Reference Cancedda, Farmer and Kerry 26 ), but a more critical question is whether the healthcare providers are receiving adequate training and competences to deliver an integrated service from pre-pregnancy to childhood. A review conducted by Jongh et al.( Reference Jongh, Gurol-Urganci and Allen 27 ) identified lack of training as a barrier to delivering an integrated tuberculosis, prevention of mother-to-child transmission and antenatal care (ANC) programme in South Africa, where not all healthcare workers were trained in all care aspects, contributing to poor tuberculosis case identification among pregnant women. The complexity of the continuum of care and the differences in economic, social, political and cultural backgrounds in each country complicates specifying the competences needed to deliver integrated care. An important first step is to ensure competent healthcare providers that have been trained with the continuum of care approach in mind for each country or region. If human and other resources are available to implement the continuum of care as recommended, it is possible to address the issues of the mother and the child at different stages, making it possible to provide health and nutrition practice messages personalised and tailored at different stages to prevent maternal and child mortality( Reference Kerber, de Graft-Johnson and Bhutta 16 ).
An estimated 700 million women, alive today, were married before their eighteenth birthday( 28 ). Preconception care would be a great entry point to discuss the adolescent's nutritional needs and how that affects their pregnancy outcome. Major micronutrients to be assessed and discussed would include iron status and folic acid assessment for the prevention of iron deficiency anaemia and neural tube defects, respectively. A randomised control trial conducted in pre-pregnant women in Tanzanian adolescents aged 15–29 years old found that supplementation of folic acid and iron significantly reduced the risk of hypochromic microcytic anaemia by 30 %( Reference Gunaratna, Masanja and Mrema 29 ). A meta-analysis conducted on micronutrient supplementation of pregnant women found that folic acid supplementation improved mean birth weight, and significantly reduced the incidence of megaloblastic anaemia by 79 %( Reference Haider and Bhutta 30 ). Other counselling that would be helpful at this level is delaying childbirth till adult onset for the adolescent( Reference Jaffee, Caspi and Moffitt 31 ).
Maternal care unlevelled playfields
The maternal mortality ratio decreased by 45 % between 1990 and 2015 globally( 14 ). In 2009 approximately 1500 women died from preventable causes related to pregnancy and childbirth every day( 18 ), while over the past decade the number has decreased to 800 women. Furthermore, 80 % of maternal deaths could have been avoided by access to essential maternity and basic health services( 32 ). Unfortunately, the improvement is not proportional across the globe as the poor countries are still losing a large number of mothers in the process of reproduction( 14 ). These maternal deaths reflect inequalities in access to health services, which highlights the gap between rich and poor( 2 ). For example, skilled care during childbirth is only available to 60 % of women, and even fewer (less than 40 %) receive a postnatal visit according to a review conducted by the International Federation of Red Cross and Red Crescent Societies( 5 ). As a result of the MDG 5 recommendations, levels of ANC have increased in many parts of the world, but only 46 % of women in low-income countries benefit from skilled care during childbirth, leaving millions of births without assistance by a midwife, a doctor or a trained nurses( 32 ). The continuum of care recommends that the mothers receive prenatal micronutrients such as folic acid and calcium in addition to adequate protein and energy, as these are specifically related to the growth of the fetus and the health of the mother, during pregnancy( Reference Lassi, Dean and Mallick 33 ). Also, this would be an opportune time to discuss the effect of alcohol, tobacco, pica and other drugs related to the health of the mother and the baby( Reference Wong, Ordean and Kahan 34 , Reference Miao, Young and Golden 35 ). The use of alcohol, tobacco and other drug substances can result a significant number of antenatal complications, neonatal and long-term negative effects in child health. In addition, women that abuse these substances are also less likely to seek prenatal care, higher risk of infections such as HIV, hepatitis or other sexual transmitted infections( Reference Wong, Ordean and Kahan 34 ). A meta-analysis carried out by Miao, Young and Golden indicated that the consumption of non-food items, such as earth, raw starch and ice generally referred to as pica, was significantly associated with the presence of anaemia, lower Hb and haematocrit concentrations and lower zinc concentrations in plasma( Reference Miao, Young and Golden 35 ). Understanding that maternal undernutrition is a risk factor for fetal growth, assessment of food insecurity as an underlying cause of nutrient deficiency is critical in achieving the sustainable development goals targeting MCH( Reference Black, Victora and Walker 6 ).
Child services care
A child born in a least developed country is fourteen times more likely to die within first 28 d of life as compared with an industrialised country( 18 ). According to the UNICEF predictions, 69 million children under age 5 will die between 2016 and 2030( 36 ). In low income countries, the majority of vulnerable mothers are still birthing their children at home unattended or attended by traditional birth attendants. Also, the practice or early clamping of the umbilical cord after birth is the norm. Thus encouraging and teaching the benefits of delayed cord clamping to increase the Hb levels of the newborn is an important first step( Reference Rabe, Diaz-Rossello and Duley 37 ). As important as vitamin K supplementation is in preventing Vitamin K deficiency bleeding, to date we do not have a mechanism of providing vitamin K to babies born at home( Reference Rabe, Diaz-Rossello and Duley 37 ).
Although there is enough evidence to show that exclusive breastfeeding is associated with infant survival, evidence that exclusive breastfeeding among low-income mothers supports normal growth is unconvincing( Reference Bhutta, Des and Rizvi 38 ). This is shown by the many children that are exclusively breastfed and are stunted as early as age 6 months( Reference Patwari, Kumar and Beard 39 , Reference Young and Martorell 40 ). A study by Brown et al. questions the adequacy of milk production on cases where the mother is food insecure or undernourished herself( Reference Brown, Akhtar and Robertson 41 ). This author recommends promotion and provision of an adequate diverse diet for the mother during the first 6 months of exclusive breastfeeding( Reference Brown, Akhtar and Robertson 41 ).
The WHO recommends the introduction of safe and nutritious foods in addition to breastfeeding at about age 6 months( 42 ). It is, however, important that we understand that for food insecure or low-income households, recommendations alone are not sufficient( Reference Lassi, Das and Zahid 43 ). For example, food contamination is a threat to the health and growth of the infant with the introduction of solid foods, underscoring the importance of educating mothers on the principles of food safety( Reference Motarjemi, Käferstein and Moy 44 ). In addition to the provision of food, it is critical to prevent childhood diseases by providing immunisations in a timely manner( Reference Guerra 45 ).
Conceptual healthcare
According to the 2015 Maternal, Newborn and Child Survival report, a total of twenty-five countries achieved their MDG 4 target by reducing childhood mortality by at least 4·4 %, while only six countries achieved the MDG 5 target by reducing maternal mortality by at least 5·5 %( 46 ). The purpose of this section is to identify the factors that contributed to the attainment of the MDG 4 and MDG 5 by at least 5·0 and 5·5 % respectively, and determine the level of the intervention, based on the conceptual framework for maternal and neonatal mortality and morbidity established by UNICEF (Table 1)( 18 ).
Table 1. Achievement of Millennium Development Goals (MDG) 4 and 5 on selected countries by level of intervention.
* Significance of colour green is to identify the percentage that is above the stated MDG 4, 5 or both.
† Significance of colour red is to identify the percentages of the countries that are below the stated MDG 4, 5 or both.
![]() Interventions at 3 levels and countries that achieved MDG 4 and 5.
Interventions at 3 levels and countries that achieved MDG 4 and 5.
![]() Interventions at 3 levels and countries that achieved MDG 4.
Interventions at 3 levels and countries that achieved MDG 4.
![]() Interventions at 2 levels (underlying and direct) and countries that achieved MDG 4.
Interventions at 2 levels (underlying and direct) and countries that achieved MDG 4.
![]() Interventions at 3 levels and countries that achieved MDG 5.
Interventions at 3 levels and countries that achieved MDG 5.
![]() Intervention at 2 levels (underlying and direct) and countries that achieved MDG 5.
Intervention at 2 levels (underlying and direct) and countries that achieved MDG 5.
![]() Interventions at 2 levels (underlying and direct) and countries that did not achieve MDG 4 and 5.
Interventions at 2 levels (underlying and direct) and countries that did not achieve MDG 4 and 5.
![]() Interventions at 1 level (direct) and countries that did not achieve MDG 4 and 5.
Interventions at 1 level (direct) and countries that did not achieve MDG 4 and 5.
The Maternal, Newborn and Child Health conceptual framework illustrates the different levels of morbidity and mortality causes starting with basic causes, followed by the underlying causes and direct causes (Fig. 2). The basic causes address societal level interventions such as politics, economics, equality and their influence on overall health and access to resources. The underlying causes, for most part a product of the basic causes, reflect causes at the community and household levels. Unaddressed underlying causes lead to the direct causes assessed at the individual level (Fig. 2)( 18 ).
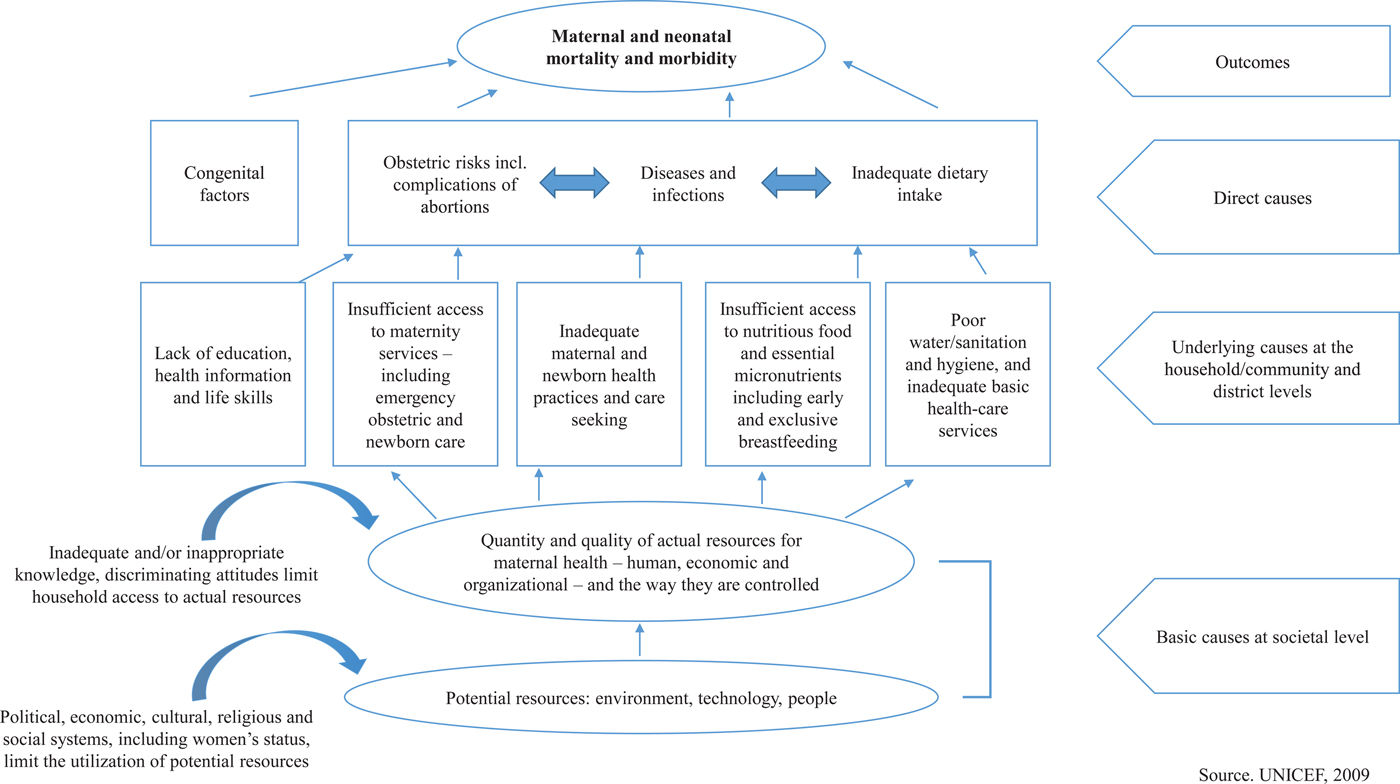
Fig. 2. Conceptual framework for maternal and neonatal mortality and morbidity( 18 ).
Factors that contributed to the achievement of Millennium Development Goals 4 and 5
The Countdown to 2015 Maternal, Newborn and Child Survival Report stated the countries that succeeded in both the reduction of child and maternal mortality as Cambodia, Nepal and Rwanda( 46 ). These three countries targeted all three levels of intervention starting with the basic causes, underlying causes and direct causes of maternal and child mortality. For example, Cambodia targeted the coverage of reproductive and maternal health services and elimination of poverty through a range of for-poor health financing and supply-side policies( Reference Dingle, Powell-Jackson and Goodman 47 ). Nepal, on the other hand, focused on extending the access and availability of primary care by increasing the human resources for health (nurses, doctors and midwives), training programmes for the health professionals in maternal care, and offering free child birth and travel costs to women. Nepal also improved their community interventions by engaging non-health professionals in providing safe MCH education in men and women( Reference Malla, Giri and Karki 48 , 49 ). Rwanda prioritised reproductive, maternal, newborn and child health throughout its policies and implemented major health sector reforms. For example, they improved the health system through the coordination of different governmental institutions, increased the national expenditures in health, and improved the health workforce and infrastructure. Also, they involved the community by implementing different programmes to improve the contraceptive prevalence rates, child immunisation and exclusive breastfeeding. In general, Rwanda prioritised its approaches in the health sector, and other areas such as education, nutrition, water supply and sanitation( 50 ).
Millennium Developmental Goal 5 achievement
While the 2015 report indicated that no country achieved MDG 5, the preliminary report in 2013 identified countries that achieved MDG 5 (reducing maternal death by 5·5 %) as Equatorial Guinea, Eritrea and Lao PDR( 46 ). According to the Countdown to 2015 Maternal, Newborn and Child Survival Report, in 2013, Eritrea, achieved their MDG goal by creating a specific package for maternal and child healthcare and nutrition, which focused on the direct and underlying causes( 46 ). For example, they improved the knowledge and healthcare skills related to MCH in the population, by giving post abortion care and counselling, advocacy, community mobilisation and capacity building, reorientation of ANC by increasing routine iron, folic acid and vitamin A supplementation, and improving family care practices. These efforts strengthened the health system, improved the attendance at birth and the emergency obstetric care services( 51 ).
Equatorial Guinea, focused on the basic social services such as health, education and protection. Also, the country programmes in coordination with UNICEF and other international agencies worked in the improvement of knowledge in basic care practices starting with the local authorities, community and families( 52 ). Lao PDR, focused on decreasing maternal mortality rates by implementing a decree that waived service fees related to childbirth and child health for pregnant women and children under age 5 at all health centres and public hospitals. In addition, to encourage participation at the community level, the operational guidelines included a financial incentive for village health workers who referred pregnant women and children under age 1 year to the health facility( 53 ).
Millennium Development Goal 4 Achievement
Bangladesh, Brazil, China, Egypt, Ethiopia, Liberia, Malawi, Mexico and Peru are among the countries that achieved more than 5 % reduction in childhood mortality( Reference Kuruvilla, Schweitzer and Bishai 54 – 62 ). The majority of the countries that achieved MDG 4 focused on the improvement of immunisation coverage and the promotion of exclusive breastfeeding. For example, Mexico focused on the direct and underlying causes by increasing immunisation rates in children, exclusive breastfeeding rates and inclusion of the neonatal screening of metabolic, auditory and retinopathy diseases( 61 ). Other countries focused on all three different levels. For instance, Ethiopia targeted all three levels of intervention in a systematic way. First, they improved the country basic services such as education and healthcare, as well as decentralisation of the policies by including different sectors and institutions for the basic causes of child mortality. Secondly, they improved the coverage of immunisation, the delivery of services to the people in their local communities by training health workers, and the promotion of healthy feeding for the infants and young children. Lastly, they addressed the direct causes by screening children for acute malnutrition, providing therapeutic foods for medically uncomplicated cases, and referring complicated cases to health facilities for admission to inpatient therapeutic feeding services( Reference Tadesse, Defar and Gatachew 58 ).
Countries with low rates in the reduction of Millennium Developmental Goals 4 and 5, or both
In an effort to understand factors that hindered the achievement of MDG 4 and 5, three countries that did not reach their target goals were chosen for this review, namely Zimbabwe, Botswana and Cameroon. Zimbabwe only decreased their under-5 and maternal mortality by 0·3 and 0·4 %, respectively. Although the country implemented several programmes in MCH at direct and underlying levels, they did not target the basic causes and important barriers at the underlying levels. For example, mothers’ religious beliefs hindered accessing healthcare at the health centres and did not include or allow health workers to offer health services at the household level. A country level intervention on the belief system would have encouraged the mothers to seek healthcare and allow healthcare workers to offer help at home. This example underscores the importance of targeting the basic and underlying causes to achieve country wide targets( 63 ).
Botswana decreased their child mortality rate by only 0·9 and a 3·1 % for MDG 5. The country focused on direct and some indirect interventions, also ignoring the basic causes. At the direct causes level, they improved the immunisation coverage and the management of diseases, while at the underlying level they focused on mobilising healthcare to the communities. However, the implementation of the programmes lacked quantity in health personnel and the inclusion of training for the actual health workers for the improvement of preventive health practices( 64 ). Cameroon only decreased their maternal mortality by 0·9 % from 1990 to 2013 compared with 1·8 % for child mortality. Their activities focused on the reduction of the direct causes like emergency obstetric care, but did not target the underlying or basic causes( Reference Mbiydzenyuy 65 ).
In general, the countries that were more likely to achieve MDG 4 and MDG 5 employed tailored interventions targeting affected populations through the direct causes. They also engaged multiple sectors to address the underlying causes by mobilising partners across the society using timely, robust evidence for decision-making and a triple planning approach to consider immediate needs, long-term objectives and adaptation to change. In addition, successful countries established guiding principles that directed progress and aligned stakeholder action( Reference Kuruvilla, Schweitzer and Bishai 54 ). Significant multisector factors for reducing maternal and child mortality included gross domestic product, poverty, skilled birth attendance, doctors per 100 people, immunisations, prenatal care, sanitation, total fertility rate and total years schooling for the females.
As analysed and described earlier, the 2015 MDG report( 14 ) indicated that the regions that succeeded in achieving their MDG goals are the ones that mitigated the problem starting at the basic level, followed by the underlying causes and the direct causes (Fig. 3). Evidences indicate that at least 20 % of the burden of disease in children under 5 years old, is related to poor maternal health and nutrition, as well as quality of care at delivery during the newborn period( Reference Black, Victora and Walker 6 ). It is therefore critical that a high proportion of interventions targeting health and survival of under 5 year old children, lay a strong foundation in targeting the pregnant mother and her health and avail skilled services needed during delivery( Reference Ramakrishnan, Grant and Goldenberg 66 ). Evidence further indicates that the nutritional status of a pregnant mother is associated with a healthy birth outcome, underscoring the importance of appropriate interventions for the mother before and during pregnancy( Reference King 8 ). Similarly, it is critical for the mother to be adequately nourished to be able to successfully breastfeed exclusively for the first 6 months( Reference Chapman and Nommsen-Rivers 67 ). There is enough evidence that exclusive breastfeeding is associated with the survival of an infant, but based on the number of exclusively breastfed children that are stunted as early as 2 months old, it is critical that the nourishment of the exclusively breastfeeding mother be assured( Reference Patwari, Kumar and Beard 39 ). It is critical that mothers are provided with nutrition education, appropriate nutritious foods and supplements to complement their diet, especially where food insecurity and poverty are prevalent( Reference Dollahite, Olson and Scott-Pierce 68 ). This is especially concerning as the 2015 report on the achievements of the MDG indicated that none of the seventy-five countries had been successful in achieving MDG 5 that targeted reducing maternal health by reducing three quarters of the maternal mortality ratio between 1990 and 2015. Conversely, only twenty-five countries met the minimum target for the MDG 4 that states to reduce child mortality by two thirds in the under-five mortality rate, between 1990 and 2015( 69 ). Lack of adequate services may explain the findings by UNICEF that stated that a child born in a least developed country is fourteen times more likely to die within the first 28 d of life than one born in an industrialised country( 18 ). According to the 2015 MDG report, twenty-five of the seventy-five countries were successful in achieving the MDG 4 targets but none of the countries achieved the MDG 5 targets( 14 ).
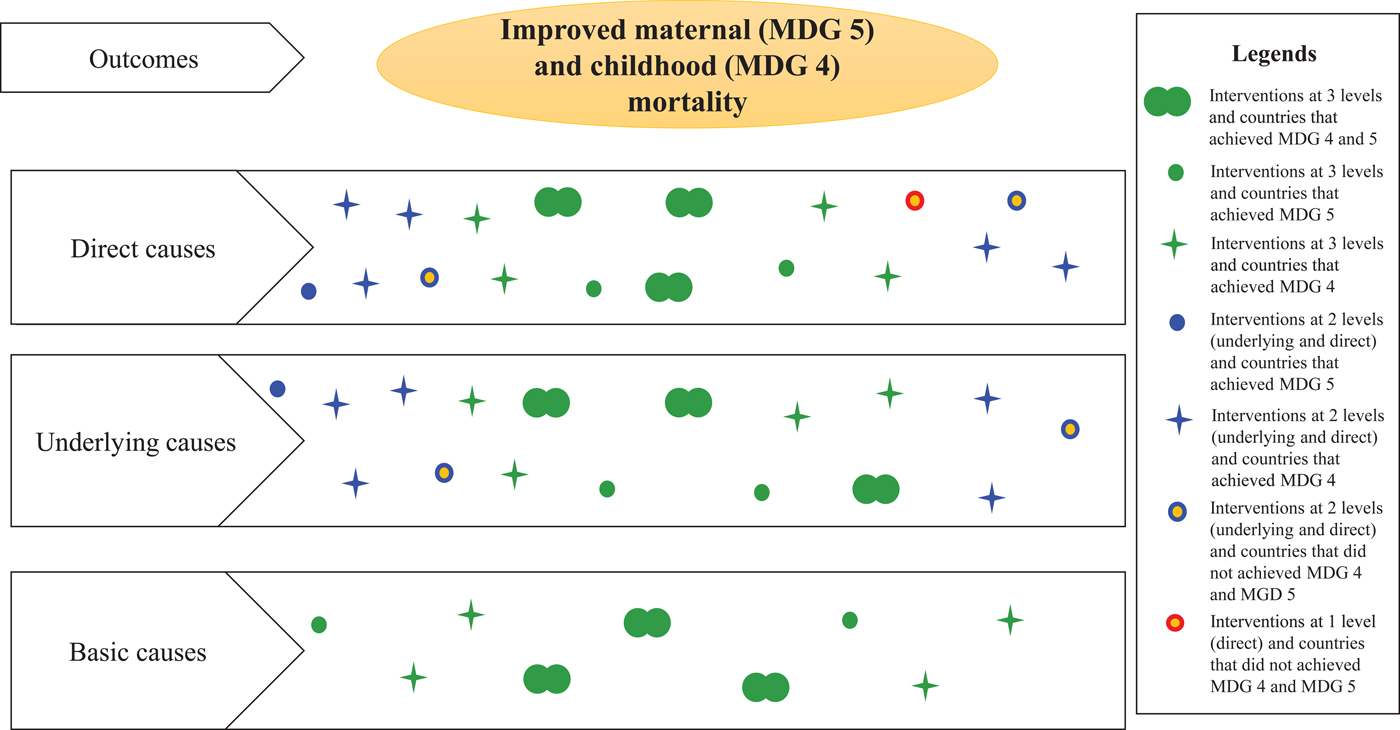
Fig. 3. Level of intervention in selected countries according to the conceptual framework.
Accessing the right care at the right time is crucial
In 2015, an estimated 303 000 women died from pregnancy-related causes( Reference Alkema, Chou and Hogan 70 ), 2·7 million babies died during the first 28 d of life( 71 , 72 ) and 2·6 million babies were stillborn( Reference Cousens, Blencowe and Stanton 73 ). Quality healthcare during pregnancy and childbirth could have prevented many of these deaths, yet globally only 64 % of women receive antenatal (prenatal) care four or more times throughout their pregnancy( 72 ). ANC is a critical opportunity for health providers to deliver care, support and information to pregnant women( 71 , 72 ). This includes promoting a healthy lifestyle, good nutrition, detecting and preventing common childhood diseases, providing family planning counselling and supporting women who may be experiencing intimate partner violence( 71 , 72 ).
The WHO new ANC model recommends increasing the number of contacts a pregnant woman has with health providers throughout her pregnancy from four to eight( 72 ). Recent evidence indicates that a higher frequency of antenatal contacts by women and adolescent girls to the health providers was associated with a reduced likelihood of stillbirths( 72 ). This reduction could be explained by the increased opportunities to detect and manage potential problems( 72 ). A minimum of eight contacts for ANC can reduce perinatal deaths by up to eight per 1000 births when compared with a minimum of four visits( 72 ). The new model increases maternal and fetal assessments to detect problems, improves communication between health providers and pregnant women, and increases the likelihood of positive pregnancy outcomes. It recommends pregnant women to have their first contact in the first 12 weeks’ gestation, with subsequent contacts taking place at 20, 26, 30, 34, 36, 38 and 40 weeks’ gestation( 72 ). However, for poor resource countries, this level of access and frequency of contact may not materialise unless extensive capacity building is initiated. In addition, the comprehensive nature of integrated healthcare will call for extensive skilled training that might not be possible with the basic training offered to community health workers( Reference Bhutta, Des and Rizvi 38 ). Integrated healthcare requires a broad level of expertise ranging from pre-pregnancy, pregnancy as well as to newborn and infant feeding( Reference Bhutta, Lassi and Pariyo 74 ). We are not convinced that the present community health workers have the required training and competences to offer those service( 1 , Reference Bhutta, Des and Rizvi 38 , Reference Bhutta, Lassi and Pariyo 74 ). The present review recommends simplifying training by forming teams of community health workers to work together with each team member trained in a specific area. For example, community health workers should be trained in groups of three with one specialising in pre-conception and pregnancy, a second specialising in infant feeding from breastfeeding to complementary foods, while yet another health worker, specialising in the healthcare for children 12–59 months and covering immunisation and diseases management( 1 ).
Unfortunately, despite the advances achieved through the MDG in MCH, WHO has projected that if the trends of the past 15 years continue for the next 15 years, by 2030, an estimated 167 million children will still be living in extreme poverty, approximately 3·6 million children under age 5 will die from mostly preventable causes, and approximately 250 000 additional deaths will occur annually from malnutrition, malaria, diarrhoea and heat stress attributable to climate change( 71 ). As a result, during 2014 the UN Open Working Group proposed a set of sustainable development goals with seventeen goals and 169 targets for a 15 year period from 2015 to 2030, which includes thirteen targets related to maternal, newborn and child health( 75 ).
What is the role of nutrition education in achieving the sustainable development goals?
The purpose of health related interventions is to improve the health of the target population. While major components of improving the health of a population is beyond the control of the target population, for the impact of the interventions to be sustained, behaviour change on part of the target population is imperative( Reference Kumar, Kumar and Ghosh 76 ). Unfortunately, many MDG, especially MDG 4 and 5, were not designed for the desired behaviour change of the target population. The evaluation and monitoring process emphasised the final outcome measure at the expense of the process and sustainability of the behaviour at the individual, community and country levels. For example, while it is desirable to reduce stunting, it is more important to know that the mothers of the stunted children are highly motivated in care seeking and nutrient-dense complementary food preparation and that they have the ability to purchase and prepare food to maximise nutritional values( Reference D'Alimonte, Deshmukh and Jayaraman 77 , Reference Lingam, Gupta and Zafar 78 ). A study carried out in Nepal found a strong positive relationship between the dietary quality and feeding practices of mothers with the nutritional status of the children. It is critical to not only recommend practices, but teach how to apply the recommendations( Reference Locks, Pandey and Osei 79 ). In addition, it is critical that the target population have inbuilt triggers for action. For example, a trigger can be hunger symptoms, malnutrition symptoms or timing of messages from the community health workers or peers. The Fogg Behaviour Model asserts that for a behaviour to be sustainably performed, motivation, ability and a trigger are critical factors to be considered for the action of an intervention( Reference Fogg 80 ). All three factors are essential for behaviour sustainability( Reference Fogg 80 ). The expected health outcome may be a motivating factor for the mother and therefore the benefits of the target behaviour should be well explained in an effort to motivate the mothers( Reference Davis, Wambach and Nelson 81 ). To increase motivation, it is critical to make sure that basic needs have been met, and that there are environmental and social support to perform the behaviour( Reference Jensen, Frongillo and Leroy 82 ). In addition to motivation, it is critical to assess the ability to perform the desired behaviour and to ensure that the target behaviour is easy to perform. The main purpose of increasing ability is making the behaviour easy to perform( Reference Newson, Lion and Crawford 83 ). The third aspect of persuasive behaviour model is setting a trigger. A trigger is a form of a reminder to act, this could be mothers understanding her child's hunger cues, or time to wash hands, or understanding child growth milestones so that she can take the child to the clinic( Reference Newson, Lion and Crawford 83 ).
In addition, effective nutrition and health education should identify the behaviour changes that are needed, based on the problem to be solved by the intervention. A proper assessment of the problem will identify the determinants and barriers of the behaviour, and the target population, followed by the intervention plan and related evaluation( Reference Ritchie, Khan and Moore 84 ). In addition, the desired behaviour should be based on evidence and this might be different in different countries( Reference Vélez, Sanitato and Barry 85 ).
Conclusions
According to the present review, the 2015 report( 14 ) on the status of the MCH gives us hope in reducing infant and maternal mortality rates and improving the health of the survivors. However, according to WHO projections, unless we change the present trend, by 2030, approximately 3·6 million children under age 5 will die from preventable causes.
An analysis of the interventions that were conducted by selected countries based on their success in achieving their targets for both MDG 4 and 5, indicate that they systematically addressed all three levels of the maternal and child framework starting with the basic or societal causes, underlying causes and finally the direct causes. An important aspect of the interventions conducted by the countries that achieved their goals was capacity building that included increasing healthcare workers and providing them with adequate training.
Conversely, the majority of the countries that did not reach their target did not address concerns at the basic or societal level and most did not include capacity building such as comprehensive training on the protocols for the healthcare workforce, shortage of medical professionals and they included a fee for their basic service. Others designed poor interventions that did not address the causes of the problems such as poor rural transportation, unavailability of drugs and medical supplies and poor quality of water in rural and urban areas.
Going forward to sustainable development goals, it is critical for each country to work on societal level problems, address the cause of the problems by addressing the underlying causes and focus on capacity building. In addition, focusing on behaviour change and identifying the barriers to change will lead to sustainable changes. As discussed earlier the countries that were more likely to succeed focused on capacity building by training their healthcare and community educators. Nutrition education is a major pillar in maternal and child survival making nutrition education a critical part of any sustainable intervention. The ability to reach the community at all levels with the appropriate intervention a function of funding is imperative. It is therefore critical that the community healthcare professionals understand factors that motivate and limit their target population in the desired behaviour change. In addition, policy makers have an important role in the development and implementation of the programmes in MCH by creating and/or improving the interventions and addressing direct, underlying, and basic causes simultaneously and in collaboration with different institutions and organisations.
Acknowledgements
The authors acknowledge Dr Md. Ruhul Amin for formatting the paper for submission and identifying some references as part of my research team, and Dr Wilhelmina Theron for critically reviewing the manuscript.
Financial Support
None.
Conflicts of Interests
None.
Authorship
M. M. conceived the idea of the manuscript, conceptualised the direction of the manuscript and revised the first drafts. A. F. M. C. identified the references, drafted the manuscript and designed the figures and table.







