The COVID-19 pandemic posed significant threats to adolescent mental health (Fegert, Vitiello, Plener, & Clemens, Reference Fegert, Vitiello, Plener and Clemens2020; Rosen et al., Reference Rosen, Rodman, Kasparek, Mayes, Freeman, Lengua and McLaughlin2021). COVID-19-related stressors such as social isolation (Francisco et al., Reference Francisco, Pedro, Delvecchio, Espada, Morales, Mazzeschi and Orgilés2020; Loades et al., Reference Loades, Chatburn, Higson-Sweeney, Reynolds, Shafran, Brigden and Crawley2020), fear of contracting the virus (Qin et al., Reference Qin, Ding, Gao, Wu, Lv and Wu2021), and financial difficulties (Gassman-Pines, Ananat, & Fitz-Henley, Reference Gassman-Pines, Ananat and Fitz-Henley2020) were associated with significant increases in mental health problems such as depression and anxiety amongst adolescents. Given the severe impact of the pandemic on youth mental health (WHO, 2022), research that focuses on identifying young people at risk of mental ill-health, as well as factors that may foster resilience to stressors such as those associated with the pandemic, is needed. Such research will offer valuable insights into the role that pandemic-related stress plays in mental health among young individuals. Furthermore, exploring the role of protective factors provides an important avenue for the identification of potential targets of early intervention/prevention strategies for young people at-risk of mental ill-health.
It is well-documented that traumatic experiences are associated with increased risk for mental health problems in young people (Kessler et al., Reference Kessler, McLaughlin, Green, Gruber, Sampson, Zaslavsky and Williams2010; McLaughlin et al., Reference McLaughlin, Greif Green, Gruber, Sampson, Zaslavsky and Kessler2012, Reference McLaughlin, Koenen, Hill, Petukhova, Sampson, Zaslavsky and Kessler2013). The stress sensitization theory purports that those with a history of trauma are at heightened susceptibility to mental health problems when exposed to subsequent stressors (Daskalakis, Bagot, Parker, Vinkers, & de Kloet, Reference Daskalakis, Bagot, Parker, Vinkers and de Kloet2013; Harkness & Hayden, Reference Harkness and Hayden2020). Some evidence suggests that those with both childhood adverse or traumatic experiences and high levels of current stress are at an elevated risk for depression (Colman et al., Reference Colman, Garad, Zeng, Naicker, Weeks, Patten and Wild2013; Patten, Reference Patten2013). As such, youth with prior traumatic experiences may be at heightened risk of the negative psychological impact of subsequent stressors such as those introduced by the COVID-19 pandemic. However, research on this topic is yet to be conducted.
Several studies have documented an association between pre-pandemic adverse experiences and poor mental health symptoms during the pandemic (Alradhi, Moore, Patte, O'Leary, & Wade, Reference Alradhi, Moore, Patte, O'Leary and Wade2022; Doom, Seok, Narayan, & Fox, Reference Doom, Seok, Narayan and Fox2021; Guo et al., Reference Guo, Fu, Liu, Zhang, Wang and van IJzendoorn2020; Perry et al., Reference Perry, Mutignani, Gissandaner, Penner, Santos and Sarver2023; Stinson et al., Reference Stinson, Sullivan, Peteet, Tapert, Baker, Breslin and Lisdahl2021). In adults, the association between COVID-19 stressors and mental health symptoms has been shown to be more positive in those with both higher levels of prior adverse experiences and high exposure to COVID-19 stressors (Alradhi et al., Reference Alradhi, Moore, Patte, O'Leary and Wade2022). However, this joint effect of COVID-19 stressors and adverse experiences is yet to be explored in adolescents. Although a prior study found that children and adolescents with higher adverse experiences showed heightened internalizing symptoms during the pandemic, adverse experiences did not moderate the association of COVID-19 impact with internalizing and externalizing symptoms (Perry et al., Reference Perry, Mutignani, Gissandaner, Penner, Santos and Sarver2023). However, given the study's sample comprised of both children and adolescents (age range 5–16 years old), it is difficult to determine if the lack of join effect of adverse experiences and COVID-19 stress observed is relevant for adolescents but not observed due to the wide age range of the sample. As such, further research specifically on adolescents is needed to elucidate whether adverse experiences such as trauma are associated with increased vulnerability to the impact of COVID-19 stressors.
Aside from studying what makes adolescents more susceptible to the effects of stressors such as those associated with the pandemic, it is also important to consider factors that can protect those at-risk. This will provide further understanding of the factors that may mitigate risk for mental health problems in at-risk adolescents. Studies have shown that more time spent doing physical activity (Okuyama et al., Reference Okuyama, Seto, Fukuda, Funakoshi, Amae, Onobe and Imamura2021), higher levels of parental support (Wang et al., Reference Wang, Toro, Scanlon, Schall, Zhang, Belmont and Plevniak2021), and closer social relationships with family (Cooper et al., Reference Cooper, Hards, Moltrecht, Reynolds, Shum, McElroy and Loades2021) and peers (Bernasco, Nelemans, van der Graaff, & Branje, Reference Bernasco, Nelemans, van der Graaff and Branje2021) were associated with reduced depression and anxiety during the COVID-19 pandemic. These factors have also been shown to buffer against poor mental health outcomes after childhood adverse experiences (Fritz, de Graaff, Caisley, van Harmelen, & Wilkinson, Reference Fritz, de Graaff, Caisley, van Harmelen and Wilkinson2018; Healy et al., Reference Healy, Eaton, Cotter, Carter, Dhondt and Cannon2022; van Harmelen et al., Reference van Harmelen, Gibson, St Clair, Owens, Brodbeck, Dunn and Goodyer2016). A prior study on adolescents with extreme childhood adversity (i.e. institutionalization) showed that social enrichment within a family context provided via foster care alleviated poor mental health outcomes associated with current stressors (Wade et al., Reference Wade, Zeanah, Fox, Tibu, Ciolan and Nelson2019). This highlights that factors such as family support may promote resilience to subsequent stressors in vulnerable young people with a history of trauma. However, no studies have examined whether these factors also promote resilience to COVID-19 stressor-related mental health difficulties in those with prior traumatic experiences.
The current study aimed to investigate the impact of traumatic experiences on COVID-19 stressor-related mental health difficulties in adolescents, as well as factors that may promote resilience. Specifically, the current study aimed to (a) examine the moderating effect of traumatic experiences on the association between COVID-19 stressors and mental health in adolescents, and (b) examine the role of protective factors including physical activity, parental support, family relationships, and peer relationships, in buffering the impact of COVID-19 stressors on mental health in those with prior traumatic experiences. Given the high prevalence of depression and anxiety during adolescence (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005), and the increased prevalence of these symptoms during the COVID-19 pandemic, the current study focused on internalizing mental health difficulties – sadness, positive affect, and perceived stress (a transdiagnostic risk factor for anxiety and depression; Lynch, Sunderland, Newton, & Chapman, Reference Lynch, Sunderland, Newton and Chapman2021).
Based on prior literature demonstrating poorer mental health in adolescents with prior adverse experiences during the pandemic, we hypothesized that higher COVID-19 stressor exposure would be associated with increased mental health difficulties, and that this association would be amplified in those with prior traumatic experiences. We also hypothesized that the associations between prior traumatic experiences, COVID-19 stressors, and mental health difficulties would vary depending on the level of protective factors. Specifically, we expected there to be an increased positive association between COVID-19 stressors and mental health difficulties in trauma-exposed adolescents with low, but not high levels of protective factors. Based on prior literature, we hypothesized that this effect would be observed for all of the protective factors.
Methods
The current study was pre-registered with the Open Science Framework (https://osf.io/45tkh). Any deviations from the preregistration have been fully described.
Participants
Participants were from the ongoing Adolescent Brain Cognitive Development (ABCD) Study (release 4.0). The ABCD Study is a large-scale longitudinal study with ~11 800 children (aged 9–10 years old at baseline) recruited from 21 sites across the US. The study aims to comprehensively characterize health and cognitive development from late childhood to late adolescence; details of the study protocol and recruitment procedure have been previously described (Barch et al., Reference Barch, Albaugh, Avenevoli, Chang, Clark, Glantz and Sher2018; Garavan et al., Reference Garavan, Bartsch, Conway, Decastro, Goldstein, Heeringa and Zahs2018). The ABCD Study was approved by the Institutional Review Board of each study site. Participant consent was obtained from the participant and their caregivers. For the purpose of the current study, participants were those who had data on any of the variables of interest (i.e. traumatic events, mental health, COVID-19 stressor exposure, and protective factor; n = 9696).
Measures
Trauma exposure
Exposure to traumatic events was assessed at baseline using the parent-report of the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) Post-traumatic Stress Disorder (PTSD) module (Kaufman et al., Reference Kaufman, Birmaher, Axelson, Perepletchikova, Brent and Neal2016). In contrast to the preregistration, trauma was treated as a binary variable (exposed and non-exposed) instead of as a continuous variable (total number of traumatic events endorsed). This was done due to the heavily skewed/zero-inflated distribution of the total trauma score (see online Supplementary Fig. S1). For transparency, results with trauma as a continuous variable have been reported in the Supplementary Material. For the binary variable, adolescents were specified as trauma-exposed if their parent/guardian endorsed any item on the PTSD module (trauma non-exposed n = 6478; trauma exposed n = 3454).
COVID-19 stressor exposure
In response to the COVID-19 pandemic, the ABCD Study conducted seven adolescent and parent-reported COVID-19 rapid response research (RRR) surveys from May 2020 to May 2021 that asked about participants' experiences during the pandemic. Based on previous studies on COVID-19 stressors and mental health (Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020; Kujawa, Green, Compas, Dickey, & Pegg, Reference Kujawa, Green, Compas, Dickey and Pegg2020; Ye et al., Reference Ye, Wu, Im, Liu, Wang and Yang2020), we examined six domains of COVID-19 stressors: (1) COVID-disease burden (two items relating to risk to contracting the virus); (2) interpersonal disruptions (three items relating to separation or disrupted contact with social support, and experiences of racial discrimination); (3) financial difficulties (six items relating loss of wage or other kinds of financial difficulties); (4) academic challenges (one item relating to schoolwork difficulties); (5) COVID-related family conflict (two items relating to increased family discord during the virus outbreak); and (6) access to medical needs (two items relating to difficulty accessing medical/mental health services). See Supplementary Material for a detailed description.
Due to the close timing of the COVID-19 surveys, some participants may have completed multiple surveys very close together, leading to potential overlaps in assessment responses. Based on this and prior studies showing evidence for a cumulative effect of COVID-19 stressors on mental health outcomes (i.e. higher number of stressor experienced was associated with poorer mental health; Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020; Kujawa et al., Reference Kujawa, Green, Compas, Dickey and Pegg2020; Rosen et al., Reference Rosen, Rodman, Kasparek, Mayes, Freeman, Lengua and McLaughlin2021), we assessed exposure to COVID-19 stressors using a cumulative count of unique stressor domains endorsed across waves. If a participant endorsed any item within a particular COVID-19 stressor domain at any point during the study's duration, we classified them as having been exposed to that particular domain. This approach resulted in a cumulative count of COVID-19 stressors for each participant, ranging from 0 to 6, reflecting the number of domains to which they were exposed during the pandemic period. We chose this approach because the stressor domains contained varying numbers of items, and items within each domain could be highly correlated and interdependent.
Moderator (protective factor) variables
We calculated average scores across the seven survey waves for the following protective factors.
Physical activity: Frequency of moderate/vigorous physical activity in the past week was measured using the International Physical Activity Questionnaire (IPAQ) short form (Lee, Macfarlane, Lam, & Stewart, Reference Lee, Macfarlane, Lam and Stewart2011). While a measure of physical activity duration was available, we did not use it due to high missingness (60–83%). The use of the frequency measure is supported by evidence indicating that the frequency of participation in physical activity is associated with a reduction in both depression and anxiety symptoms (Singh et al., Reference Singh, Olds, Curtis, Dumuid, Virgara, Watson and Maher2023).
Family and peer relationships: Changes in family and peer relationship quality were assessed by two individual items that asked the adolescent to rate their relationship with their family and friends respectively in the past week, on a 5-point Likert scale (1 = a lot worse, 3 = about the same, and 5 = a lot better).
Parental support: Parental support was assessed using an item that asked about the number of days a parent was involved with the child's schoolwork in the past week (maximum = 7 days).
As not all measures were administered at all waves, the use of average scores, as opposed to sum scores, provide an indication of the overall level of protective factors during the COVID-19 period assessed by the ABCD Study. In addition, the use of average scores also minimizes the impact of missing values on the results. All variables used for this calculation were extracted from the youth report section of the RRR surveys.
Outcome variables
Average scores for perceived stress, sadness, and positive affect were calculated across the seven RRR surveys. Averages rather than sum scores were calculated for the same reason as the moderator variables. All variables were youth reported.
Perceived stress: Perceived stress was measured at every survey wave using the four-item version of the Perceived Stress Scale that has been widely used to assess stress levels (Cohen, Kamarck, & Mermelstein, Reference Cohen, Kamarck and Mermelstein1983). A total perceived stress score was calculated by summing across the four items. The items asked about how often the respondent felt stressed about how things went in the past months (e.g. how often have you felt that you were unable to control the important things in your life). Items were measured on a 5-point Likert scale, ranging from 0 to 4, with 0 = never, and 4 = very often.
Sadness and positive affect: Both sadness and positive affect were measured using the National Institute of Health Toolbox Emotion Battery (v2.0). Sadness was measured (at survey 1, 3, 5, and 7) by eight items asking the adolescent about experiences of low mood in the past week (e.g. in the past week, I felt unhappy). Responses were recorded on a 5-point Likert scale, ranging from 1 to 5, with 1 = never, and 5 = almost always. Positive affect was measured (at survey 2, 4, and 6) by 9 items asking the adolescent about their positive emotional experiences such as happiness, calmness, and enthusiasm in the past week. Responses were recorded on a 3-point Likert scale where 1 = not true, and 3 = very true. Sum of raw scores were then created for both sadness and positive affect.
Covariates
Age (averaged across the seven RRR surveys), sex, socioeconomic status (SES), family, and site were included as covariates in all statistical models. SES was measured using income-to-needs ratio assessed at baseline (the most recent timepoint prior to the COVID-19 outbreak). A value of one would indicate being at the poverty threshold whereas values greater or less than one suggests being above or below the threshold, respectively (see Supplementary Material for a detailed description).
Statistical analysis
All analyses were conducted using the lme4 package (v1.1–33; Bates, Mächler, Bolker, & Walker, Reference Bates, Mächler, Bolker and Walker2015) in R version 4.3.0 (R Core Team, 2022). To address Aim 1, we conducted linear mixed-effects models with mental health variables (perceived stress, sadness, and positive affect) as the outcome variable (in separate models) and the interaction between trauma exposure and COVID-19 stressors as the predictors (lower order main effects were also included). For our second aim, models included mental health variables as the outcome variable in separate models and three-way interactions between trauma, COVID-19 stressors, and protective factors (i.e. physical activity, family relationships, peer relationships, and parental support) as predictors. Lower-order main and interaction effects were automatically included. Each protective factor was analyzed in a separate model. As such, a total of 12 models were run (four protective factors by three mental health difficulties). False discovery rate (FDR) correction across all models was utilized to correct for multiple comparisons (pFDR < 0.05; Benjamini & Hochberg, Reference Benjamini and Hochberg1995). Age, sex, and SES were included as fixed effects and family ID and study site were included as random effects in all models. In follow-up analyses to aid interpretation of the three-way interaction effects, we examined the association of two-way interactions of (1) COVID-19 stressor and protective factors and (2) trauma exposure and protective factors with mental health outcomes. Each two-way interaction was included in a separate model (with main effects included). This resulted in 24 models (2 two-way interactions × 4 protective factors × 3 mental health outcomes). An FDR correction of p < 0.05 was applied to each set of two-way interaction models for each mental health outcome (8 models).
Missing data
Analyses were conducted using cases with no missing data for the variables included in each model. Participants with missing data for all items of a particular scale were excluded from analyses. Missingness of specific items within scales were handled either by using a cumulative count of data (for total trauma and COVID-19 stressor exposure variables), or by average across waves (for the protective factors and outcome variables).
Sensitivity analyses
Preregistered sensitivity analyses using data from participants who responded to at least 50% of the surveys (i.e. ≥4 surveys), were not possible to conduct due to some measures having been collected only at three waves. Additional analyses were also performed with trauma as a continuous variable for transparency. Given that prior mental health problems are a strong predictor of mental health problems during the pandemic (Neelam, Duddu, Anyim, Neelam, & Lewis, Reference Neelam, Duddu, Anyim, Neelam and Lewis2020), primary analyses were also repeated with pre-COVID (i.e. baseline) total mental health problem as an additional covariate. Pre-COVID total mental health problem was assessed using the parent-reported Child Behavior Checklist total problems subscale (Achenbach, Reference Achenbach and Maruish1999).
Results
Demographic information
A total of 9696 participants (4624 females; M age = 12.85 years, s.d.age = 0.88, range = 10.71–15.58) were included in analyses. N for each analysis ranged from 5589 to 7973. The smallest sample included in analyses (N = 5589) were not statistically different from sample not included in terms of baseline age (t[11 711] = −1.09, p = 0.275; mean age for analyzed sample = 9.91 years v. not included in sample = 9.92 years). However, in comparison to the sample not included, the analyzed sample showed significantly higher income-to-needs ratio (M = 4.07 v. 3.27; t[10 494] = 17.16, p < 0.001) and parent education attainment (M = 15.94 v. 14.66 years; t[11 849] = 26.24, p < 0.001), indicating higher SES in the analyzed sample. The analyzed sample also showed significantly lower total number of traumatic events endorsed (M = 0.46) in comparison to those not included (M = 0.55; t(11 541) = −5.29, p < 0.001). For detailed demographic information and descriptive statistics, refer to Table 1.
Table 1. Demographics and descriptive statistics

Note: All variables, except for income-to-needs ratio, trauma, and COVID-19 stressors, are averaged scores across the seven available waves of the ABCD COVID-19 RRR survey. ^ denotes percentages calculated from the total number of trauma exposed participants as opposed to the total sample. We have only included the top five type of trauma (of the 17 recorded by the KSADS measure) endorsed by participants here. For details on endorsement of other types of traumatic experiences refer to Supplementary Material.
Relationship between trauma, COVID-19 stressors, and mental health outcomes
Three separate linear mixed-effects models were conducted with perceived stress, sadness, and positive affect as outcomes. The main effect of COVID-19 stressors was significant in all models (Table 2). Specifically, higher levels of COVID-19 stressors were associated with higher sadness and perceived stress and lower positive affect. The main effect of trauma exposure was significant for perceived stress and sadness whereby mean stress and sadness were higher in trauma-exposed than trauma non-exposed adolescents. However, trauma exposure was not associated with positive affect. Trauma exposure significantly moderated the association between total COVID-19 stressors and sadness, but not perceived stress or positive affect (Fig. 1). Specifically, the association between COVID-19 stressors and sadness was more positive in trauma-exposed than non-exposed adolescents. See Supplementary Material Table S6.1–6.3 for detailed model output. Results were unchanged using cumulative trauma exposure as a continuous variable (see Supplementary Material section S11). Similarly, results remained consistent when we accounted for pre-COVID total mental health problems with one exception; the main effect of binary trauma exposure on perceived stress and sadness was no longer significant (see Supplementary Material section S12).
Table 2. Model output for interaction between trauma exposure and total COVID-19 stressors in association with mental health outcomes
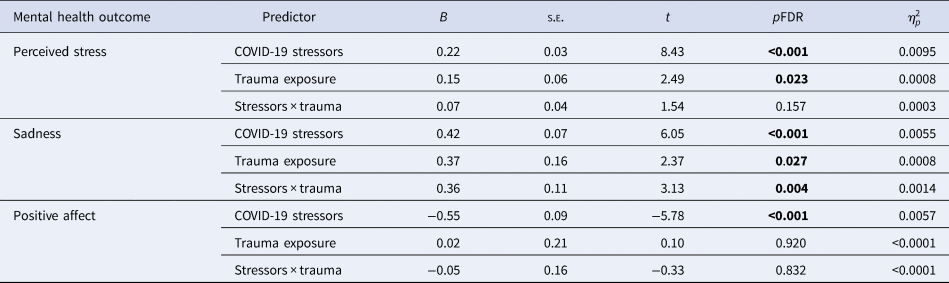
Note: Bold text indicates significant results (pFDR < 0.05). Partial eta-square was generated using R package ‘effectsize’ (Ben-Shachar, Lüdecke, & Makowski, Reference Ben-Shachar, Lüdecke and Makowski2020), which computes effect size approximate conversions from test statistics.

Figure 1. Interaction plot for the interaction effect of trauma exposure and COVID-19 stressors on sadness, perceived stress, and positive affect.
Note: Interaction between COVID-19 stressors and trauma exposure and sadness (a), perceived stress (b) and positive affect (c). * indicates significant effects. Simple slopes for trauma-exposed and non-exposed depicted are statistically significant (p < 0.001) for all models. The interval around the regression line depicts 95% CI for the association.
The role of protective factors in the relationship between trauma, COVID-19 stressors, and mental health outcomes
No significant three-way interaction between trauma exposure, total COVID-19 stressors, and protective factors (i.e. physical activity, parental support, and changes in family and peer relationships) was observed for sadness, perceived stress, or positive affect (see Table 3 for model output summary). Results using a continuous trauma score remained largely consistent with our main analyses, with the exception of a significant three-way interaction for positive affect. Follow-up analyses of simple slopes revealed that adolescents with higher parental support for schoolwork had higher levels of positive affect at a high number of COVID-19 stressors, but only if they had a lower number of traumatic experiences. In adolescents with high traumatic experiences, higher parental support was associated with higher levels of positive affect only when COVID-19 stressor experience was low. See Supplementary Material section S11.3 for a detailed description and interaction plot. Results with pre-COVID total mental health problems as an additional covariate were also consistent with the main results (see Supplementary Material section S12).
Table 3. Model output for three-way interaction between protective factor, trauma exposure, and total COVID-19 stressors in association with mental health outcomes
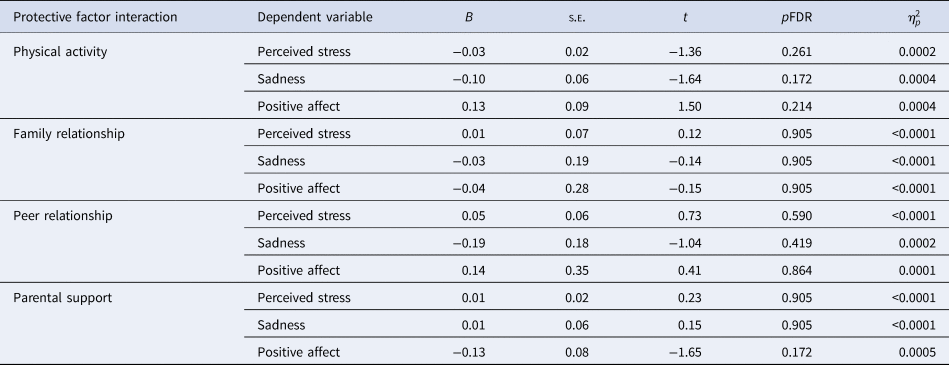
Note: The results reported are for the three-way interaction between the moderator, total COVID-19 stressors, and trauma exposure. Partial eta-square was generated using R package ‘effectsize’ (Ben-Shachar et al., Reference Ben-Shachar, Lüdecke and Makowski2020), which computes effect size approximate conversions from test statistics. For detailed model outputs for these reported models, refer to Supplementary Material section S7.
Given the lack of significant three-way interactions in main analyses, we conducted follow-up mixed effects models to examine the lower-order two-way interactions between each protective factor and COVID-19 stressors, as well as between each protective factor and trauma exposure. This approach enabled us to assess whether the non-significant three-way interactions stemmed from protective factors exhibiting consistent protective effects regardless of the presence or absence of trauma or COVID-19 stressors. Each two-way interaction was included in a separate model (with main effects included). These analyses revealed that no protective factors moderated the association between trauma exposure and mental health outcomes. That is, higher levels of all protective factors were associated with lower levels of mental health difficulties for both trauma-exposed and non-exposed adolescents (see Supplementary Material section S8 for detailed model output). Changes in family and peer relationship quality significantly moderated the association between COVID-19 stressors and all three mental health outcomes (see Table 4). Specifically, the positive associations between COVID-19 stressors and both perceived stress and sadness were attenuated when there were relatively greater improvements in both family and peer relationship quality (see Fig. 2). Similarly, the negative association between COVID-19 stressors and positive affect was also reduced when there were relatively greater improvements in family and peer relationship quality (see Fig. 2). No significant moderating effects were observed for physical activity and parental support on the association between COVID-19 and mental health difficulties.
Table 4. Model outputs for significant two-way interactions between protective factor and COVID-19 stressors

Note: The results reported are for the two-way interaction between total COVID-19 stressors, and protective factors. All results are significant (pFDR < 0.05). Partial eta-square was generated using R package ‘effectsize’ (Ben-Shachar et al., Reference Ben-Shachar, Lüdecke and Makowski2020).

Figure 2. Association between COVID-19 stressors and perceived stress, sadness, and positive affect, at varying levels of change in family and peer relationship quality.
Note: Association between COVID-19 stressors and perceived stress (a), sadness (b), and positive affect (c), at various levels of change in family relationship quality (i.e. at mean and ± 1 s.d.). Association between COVID-19 stressors and perceived stress (d), sadness (e), and positive affect (f) respectively, at various levels of peer relationship quality (i.e. at mean and ± 1 s.d.). * indicates significant interaction effects. Simple slopes for family and peer relationship quality depicted are statistically significant at mean and ± 1s.d. (p < 0.001) for all models. The interval around the regression line depicts 95% CI for the association.
Discussion
The present study aimed to examine whether prior trauma exposure exacerbated the association of COVID-19 stressors with mental health difficulties in adolescents. We further examined whether the presence of protective factors, such as physical activity, parental support, and family and peer relationship quality reduced the strength of this association. We found that trauma exposure strengthened the positive association between COVID-19 stressors and sadness, but not for perceived stress or lower levels of positive affect. We also found that improvements in family and peer relationship quality reduced the strength of the association between COVID-19 stressors and mental health difficulties regardless of prior trauma exposure.
Consistent with our hypotheses, trauma exposure moderated the association between COVID-19 stressors and sadness such that the association between COVID-19 stressors and sadness was more positive in trauma-exposed adolescents. Our findings extend previous research that showed a positive association between traumatic experience and mental health difficulties among adolescents during the pandemic period (Guo et al., Reference Guo, Fu, Liu, Zhang, Wang and van IJzendoorn2020; Stinson et al., Reference Stinson, Sullivan, Peteet, Tapert, Baker, Breslin and Lisdahl2021) by showing that this effect is most pronounced in those who are also exposed to higher levels of current stressors. Importantly, findings align with the stress sensitization theory that purports that trauma exposure makes one more susceptible to, or ‘sensitizes’ one to the negative psychological effect of subsequent stressors (Daskalakis et al., Reference Daskalakis, Bagot, Parker, Vinkers and de Kloet2013; Harkness & Hayden, Reference Harkness and Hayden2020). These results are also consistent with studies in adults. Specifically, it has been shown that mental health symptoms were greatest in adults with both higher number of adverse experiences and high COVID-19 stressor exposure (Alradhi et al., Reference Alradhi, Moore, Patte, O'Leary and Wade2022). Our results suggest that stress sensitization starts early and is present during adolescence. This highlights the need to provide early support to adolescents with a history of traumatic experiences to reduce the impact of future stressors. The same relationship was not observed for perceived stress and positive affect. Past evidence of the stress sensitization theory has shown an increased risk of depression in young people with adverse or traumatic childhood experiences (Colman et al., Reference Colman, Garad, Zeng, Naicker, Weeks, Patten and Wild2013; Patten, Reference Patten2013). It is therefore possible that the trauma-associated sensitization effect is specific to domains of depression such as sadness or negative affect, as opposed to other domains such as anhedonia (i.e. lack of ability to experience positive affect/pleasure). However, this is speculative and further work is needed to clarify these relationships.
The association between COVID-19 stressors and mental health difficulties was reduced when family and peer relationship quality had improved during the pandemic, for both trauma-exposed and non-exposed adolescents. This finding, which suggests a universal protective effect of these factors against COVID-19 stressors for all adolescents, was consistent with our hypothesis. These findings align with prior research and theory that has consistently suggested a beneficial impact of stronger family and peer relationships in mitigating the psychological toll of COVID-19 stressors on adolescents (Bernasco et al., Reference Bernasco, Nelemans, van der Graaff and Branje2021; Cooper et al., Reference Cooper, Hards, Moltrecht, Reynolds, Shum, McElroy and Loades2021; Montero-Marin et al., Reference Montero-Marin, Hinze, Mansfield, Slaghekke, Blakemore and Byford2023; Prime, Wade, & Browne, Reference Prime, Wade and Browne2020).
Stable and/or improved family relationship quality (e.g. more time spent together and increased support from family members) was commonly observed during the COVID-19 pandemic (Bülow, Keijsers, Boele, van Roekel, & Denissen, Reference Bülow, Keijsers, Boele, van Roekel and Denissen2021; Martin-Storey, Dirks, Holfeld, Dryburgh, & Craig, Reference Martin-Storey, Dirks, Holfeld, Dryburgh and Craig2021; Rogers, Ha, & Ockey, Reference Rogers, Ha and Ockey2021). In contrast, peer relationship quality has generally been reported to have decreased during the pandemic due to school closure and lack of in-person social interactions (Rogers et al., Reference Rogers, Ha and Ockey2021; Widnall et al., Reference Widnall, Adams, Plackett, Winstone, Haworth, Mars and Kidger2022). Given the protective role of family and peer relationships for COVID-19-related mental health problems in youth, identifying strategies for improving family and peer relationship quality, such as increasing quality family time and improving digital social interaction quality (James et al., Reference James, Silk, Scott, Hutchinson, Wang, Sequeira and Ladouceur2023), may be beneficial for youth mental health, especially for those with a history of traumatic experiences. However, this is only speculative, and future research is needed to examine the effectiveness of strategies for improving family and peer relationship quality in reducing youth mental health difficulties.
Social relationships during adolescence, such as those with family and peers, have been suggested to promote healthy stress responses via supporting the healthy development of emotion regulation, coping, and problem solving abilities in adolescents, which in turn protect adolescents from the negative impact of stressors (Chen & Harris, Reference Chen and Harris2019; Thoits, Reference Thoits2011). Animal and adult research has also suggested that positive social relationships are associated with better emotional experiences during stressor exposure via changes in the neurophysiological stress response, such as reduced sympathetic system activity and increased activity in brain regions involved in detection of safety (Eisenberger, Reference Eisenberger2013). These findings may have implications for promoting mental health during stress exposure; however, further research in this area is needed to shed light on the specific neurobiological and neurophysiological mechanisms underlying the buffering effect of peer and family relationships for adolescent mental health.
We did not observe the same protective effect of physical activity. The lack of a protective effect of physical activity is inconsistent with prior literature, which has shown the buffering effects of physical activity on COVID-19 stressor-related mental health difficulties (Okuyama et al., Reference Okuyama, Seto, Fukuda, Funakoshi, Amae, Onobe and Imamura2021). In contrast to our study, which assessed frequency of participation, past work on the protective effect of physical activity has primarily considered the duration of time spent participating in physical activity. Our choice to use frequency was partially based on high levels of missingness for the duration measure within the sample. As such, the null results here may not necessarily suggest that physical activity has no role to play in resilience, but instead reflect that duration rather than frequency of physical activity participation may promote resilience to stressor-related mental health difficulties. Given the compelling evidence in support of the anti-depressive effects of physical activity for adolescents (Oberste et al., Reference Oberste, Medele, Javelle, Lioba Wunram, Walter, Bloch and Zimmer2020), further exploration of its protective role in trauma-exposed adolescents is warranted.
This study is the first to examine the role of parental support for schoolwork in promoting resilience to mental health problems in the context of COVID-19 stressors and traumatic experiences. Our results, although preliminary, suggest that parent support for schoolwork may not be relevant for promoting resilience to COVID-19 stressor-related mental health difficulties. Prior research on the protective role of parental support examined aspects of social support as opposed to academic support from parents (Wang et al., Reference Wang, Toro, Scanlon, Schall, Zhang, Belmont and Plevniak2021). This suggests that despite the pandemic period being a period of reduced school support for adolescents, parental social support, as opposed to academic support, may likely be of more benefit to adolescent mental health during the COVID-19 pandemic.
However, when prior trauma was modelled as a continuous variable (i.e. total number of traumatic experiences), the results showed that higher parental support for schoolwork was protective against reductions in positive affect for adolescents with either high levels of traumatic experiences or a high number of COVID-19 stressors (but not both). That is, higher parent academic support cannot mitigate the joint negative effect of high trauma and COVID-19 stressors. However, given that this finding was not present when the trauma variable was binarized, caution must be taken when interpreting the results. The mixed finding observed in the present study for the protective effect of parental support for schoolwork highlights the need for further research on the topic.
The following limitations should be considered when interpreting findings. First, we did not consider the type or severity of trauma, which have both been suggested to have implications for adolescent mental health post traumatic experiences (Hodgdon et al., Reference Hodgdon, Spinazzola, Briggs, Liang, Steinberg and Layne2018). Second, all traumatic events were not equally endorsed; the most endorsed traumatic events were death of someone close, family physical conflicts, and involvement in accidents or disasters, with fewer participants endorsing childhood maltreatment experiences such as physical/sexual abuse and neglect. Our results may not extend to traumatic experiences that were not commonly reported in the ABCD sample. To better understand the intricate association between past trauma, response to subsequent stressors, and mental health outcomes in adolescents, future work should consider the influence of chronicity, intensity, and type of experience.
In addition, given that there is low agreement between parent and adolescent reports of certain traumatic events, such as social victimization and interpersonal trauma (Stover, Hahn, Im, & Berkowitz, Reference Stover, Hahn, Im and Berkowitz2010; Tang, Saadi, Dunn, & Choi, Reference Tang, Saadi, Dunn and Choi2023), the parent-reported measure of trauma used in the present study may not have accurately captured some aspects of adolescent experiences. However, as the most commonly reported traumatic events in the ABCD sample were not interpersonal in nature, and prior evidence has indicated moderate agreement between parent and child reports of non-interpersonal trauma (Stover et al., Reference Stover, Hahn, Im and Berkowitz2010), the accuracy of these reports are likely less affected. Nevertheless, caution should be exercised when interpreting the results.
Third, the results may also have been impacted by not all variables of interest being measured at all waves. Despite our efforts to minimize the impact of this via averaging as opposed to summing scores, some questions only asked participants about experiences in the past week (e.g. mental health outcomes). This may have led to transient experiences at specific timepoints being captured by the measure, potentially overlooking mental health occurrences between these periods where the measures were not administered.
Fourth, our examination of peer and family support is also limited by the ambiguity of the timeframe. Participants were asked to rate on whether their relationship with family/friends was ‘a lot better’, ‘a little better’, ‘about the same’, ‘a little worse’, or ‘a lot worse’ in the past week. However, as the items lacked a specific reference point is (e.g. pre-pandemic or prior to last week), there might have been variability in participants' interpretations (e.g. some may have compared to levels before the pandemic whereas others may have compared it to a different point during the pandemic). As such, we cannot comment on whether the observed effects of improvements in family and peer relationships promoting resilience was in relation to changes relative to pre-pandemic or more recent levels of relationship quality and support.
Fifth, we were unable to consider other modifiable protective factors such as sleep quality, time spent in green spaces, positive school environment, and community cohesion that have been found to promote resilience in adolescents (Cooper, Di Biase, Bei, Quach, & Cropley, Reference Cooper, Di Biase, Bei, Quach and Cropley2023; Masten, Lucke, Nelson, & Stallworthy, Reference Masten, Lucke, Nelson and Stallworthy2021; Rakesh, Zalesky, & Whittle, Reference Rakesh, Zalesky and Whittle2023; Rosen et al., Reference Rosen, Rodman, Kasparek, Mayes, Freeman, Lengua and McLaughlin2021). Future studies would benefit from exploring the role of other factors in resilience to the negative psychological impact of traumatic experiences and/or future stressors in adolescents. Further, the mental health outcomes explored in the present study were limited to internalizing-type problems. As such, we cannot comment on whether the buffering effect observed extends to different domains such as externalizing symptoms, an important avenue for future research in the area.
It should also be noted that we only examined the role of protective factors in the context of COVID-19 stressors. Given the relative lack of research on other stressors in this context, it is unclear whether these protective effects extend beyond stressors associated with the COVID-19 pandemic. Moreover, although all six domains of COVID-19 stressors examined in the present study (i.e. academic challenges, disease burden, family conflict, financial difficulties, interpersonal disruptions, and limited medical access) were relatively evenly endorsed by participants (see online Supplementary Fig. S10), family conflict and interpersonal disruptions were the most highly endorsed of all. Therefore, the buffering effect of social relationships observed in the present study may be most relevant to family conflict and interpersonal disruptions. Future studies should investigate the protective effects of family and peer relationships on response to stressors outside of the pandemic context. This would shed light on the generalizability of these protective effects and their applicability to various types of stressors. Finally, it should be noted that participants in the analyzed sample were of relatively higher SES and endorsed lower total number of traumatic events in comparison to those not included in the analyses. As such, our findings may be limited to this particular sample of adolescents.
In summary, the present study demonstrated an increased vulnerability to the impact of COVID-19 stressors on sadness levels in trauma-exposed young people. We also showed a universal protective effect of improvements in family and peer relationships for COVID-19 stressor related mental health difficulties, which seem to be relevant for both trauma-exposed and non-exposed adolescents. This latter finding underscores the significance of social support networks in resilience, highlighting their potential to be instrumental in buffering against the detrimental mental health effects of current stressors, including those related to the unique challenges posed by the COVID-19 pandemic. Our findings provide further evidence in support of the stress-sensitization theory of early traumatic experiences. They also suggest potential early intervention targets for young people currently experiencing stress, including those with a history of traumatic experiences.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724001806.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. However, the author, L. Z., acknowledges the support provided by the Research Training Program Scholarship offered by the University of Melbourne and the Australian Commonwealth Government, and the Nick Christopher Scholarship offered by the University of Melbourne during the research process. This research utilized data from the Adolescent Brain Cognition Development (ABCD) Study, which is funded by NIH and federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. For a comprehensive list of the funding partners, please visit https://abcdstudy.org/federal-partners.html. The authors would like to acknowledge all researchers, staff, and participating families and young people that have contributed to the ABCD Study.









