1. Introduction
Cardiovascular diseases (CVDs) are a leading cause of mortality globally and responsible for up to 32% of all deaths in the world [1]. One of the major risk factors for CVDs is smoking tobacco. In particular, smoking is associated with the development of atherosclerosis and is known to induce oxidative stress and damage endothelium, which can be observed clinically [Reference Messner and Bernhard2]. Preventive action is necessary to reduce the risk of CVD, mainly by smoking cessation. Smoking cessation is effective in lowering the risk of CVD among smokers when done earlier than 5 years [Reference Duncan, Freiberg, Greevy, Kundu, Vasan and Tindle3]
In recent decades, the electronic cigarette has gained popularity as it is marketed as an alternative to tobacco smoking. The electronic cigarette is a battery-powered device that heats refillable premix liquid (e-liquid) to aerosol. Major compounds in e-liquid include propylene glycol, ethylene glycol, glycerol, flavors, and optional nicotine in various concentrations [Reference Hahn, Monakhova and Hengen4]. The aerosol produced is inhaled by users and the action is commonly known as ‘vaping’.
Since being introduced to the market in the mid-2000s, many people from all over the world have gained access to the device. Users may range from as young as youths to young adults and adults. In the United States and European countries, the electronic cigarette use is more prevalent among males, younger adults, current smokers, and former smokers [Reference Kapan, Stefanac, Sandner, Haider, Grabovac and Dorner5, Reference Villarroel, Cha and Vahratian6]. In a survey by Etter and Bullen [Reference Etter and Bullen7], 96% of 3587 users considered the electronic cigarette as a means of smoking reduction or smoking cessation.
Considering the adverse effects of smoking in general, the health effect of using electronic cigarettes is likewise questionable. Furthermore, the e-liquid, aerosol, and smoke of electronic cigarettes of various brands have been found to contain potentially damaging compounds, such as tobacco-specified nitrosamines (TSNAs), aldehyde, metals, volatile organic compounds (VOCs), and tobacco alkaloids in variable amounts [Reference Cheng8].
The electronic cigarette is deemed a safer option than conventional cigarettes, though not completely safe [Reference Chen, Bullen and Dirks9]. However, the effect of the electronic cigarette use on the vascular system has remained unclear. There is a potentially worrying effect of electronic cigarettes, yet the evidence is still limited [Reference Skotsimara, Antonopoulos and Oikonomou10]. In this article, we performed a systematic review to explore recent literature on the effect of the electronic cigarette, specifically on the vascular system.
2. Methods
2.1. Study Selection
Relevant literature published from January 2016 to August 2021 was obtained from the MEDLINE (PubMed) database. Keywords used on search strategy are (“Electronic Nicotine Delivery Systems”[Mesh] OR “Vaping”[Mesh] OR “E-Cigarette Vapor”[Mesh] OR e-cigarette*[tw] OR “electronic cigarette*”[tw] OR “e-cigarette vapor”[tw] OR vape[tw] OR vapes[tw] OR e-cigs[tw] OR mods[tw] OR “vape pens”[tw] OR “tank systems”[tw] OR “electronic nicotine delivery systems”[tw]) AND (“Blood Vessels”[Mesh] OR “Arteries”[Mesh] OR “Vascular Stiffness”[Mesh] OR “Atherosclerosis”[Mesh] OR aorta[tw] OR “vascular effect*”[tw] OR “endothelial function”[tw] OR “arterial stiffness”[tw] OR “coronary artery”[tw] OR “smooth muscle cell” [tw]). The studies gathered from the database search were exported to the Mendeley reference manager and screened for duplicates. Articles are manually selected that contain relevant studies related to the electronic cigarette and its impact on the vascular system.
Initial screening was done based on article type, title, and abstracts, followed by full-text screening. Studies on cells, case series, case reports, and irrelevant studies were excluded. Included articles must evaluate the chronic impact of electronic cigarettes on the vascular system in terms of clinical adverse events among adult or animal populations within 2016 and 2021. The data was input manually by author.
2.2. Risk of Bias Assessment
Studies are differentiated into human randomized interventional study (randomized controlled trial or RCT), human observational cross-sectional study, and animal interventional study. The Cochrane Risk of Bias 2 (RoB 2) was used for human RCTs, NIH Quality Assessment for Cross-Sectional Study for human observational cross-sectional study, and SYRCLE’s Risk of Bias (SYRCLE’s RoB) for animal interventional study.
2.3. Data Extraction
Data were extracted from included articles with a predetermined standardized data form. Extracted data include author, year of publication, characteristics of participants, number of participants, type of interventions, nicotine concentration, length of exposure, and main conclusion. Studies are grouped into human studies or animal studies. Results were described narratively because of the nature of the included studies.
2.4. Systematic Search
The initial search showed 101 results in PubMed from January 2016 to October 2021. A total of 101 articles were selected further to be screened by content. After the full-text screening, 16 articles were included in this systematic review. The PRISMA Flow Diagram is provided in Figure 1.

Figure 1: PRISMA Flow Diagram of study selection.
2.5. Literature Characteristics
The characteristics of the articles included are available in Table 1. There are interventional and observational studies. Interventional studies recruited occasional to heavy smokers and used model mice when assessing the chronic effects of electronic cigarettes with and/or without nicotine. Observational studies recruited nonsmokers and chronic smokers to observe chronic effects of electronic cigarettes.
Table 1: Characteristics of included study.
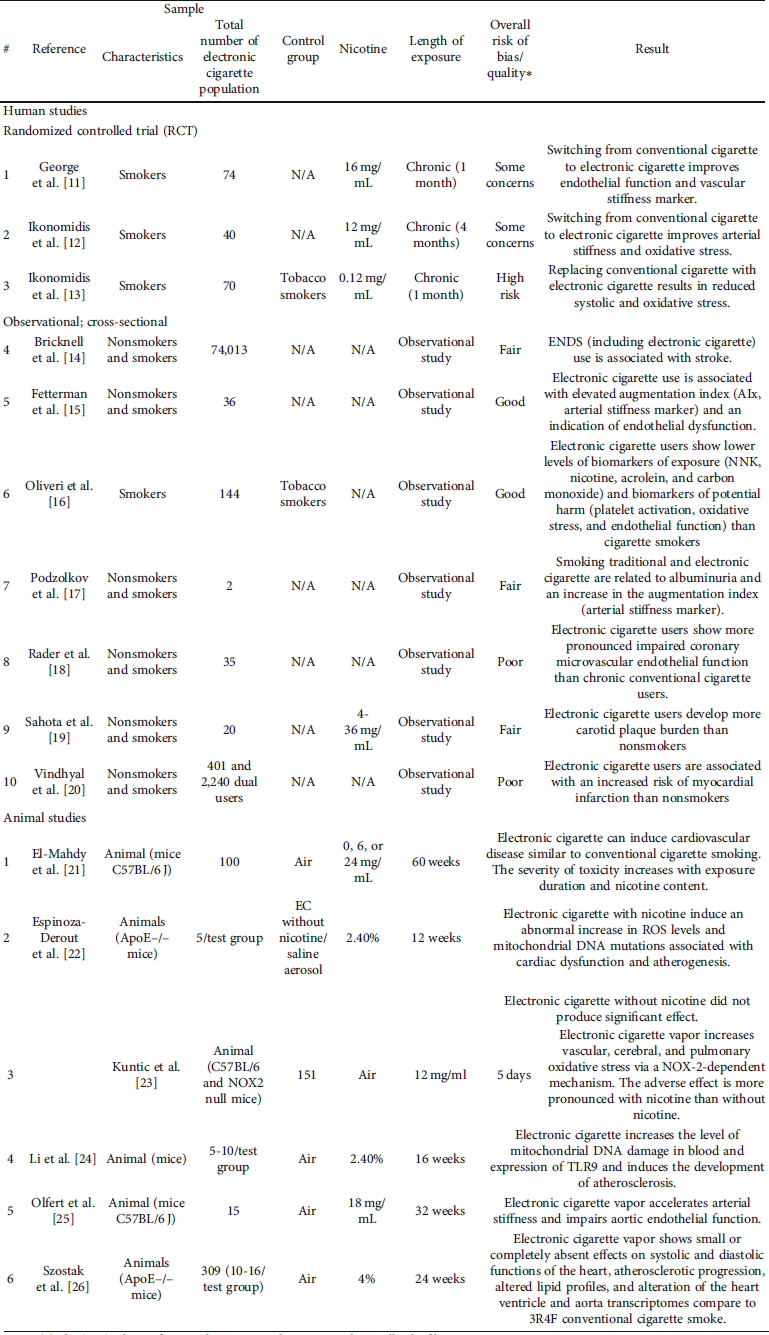
Notes: (*) The SYRCLE’s RoB for animal intervention does not provide overall risk of bias.
In interventional human studies, studies lasted one to four months with the nicotine level used in electronic cigarettes varying in concentration from 0.12-16 mg/mL. Meanwhile, in interventional animal studies, the period of studies was between 5 days to 60 weeks and the nicotine concentration ranged from 6 to 24 mg/mL and 2.4% to 4%. All studies measured various clinical parameters and biomarkers on the vascular function, mostly including arterial stiffness, endothelial dysfunction, inflammation, and atherosclerosis.
3. Results
In human studies, the type of studies can be interventional (randomized controlled trials or RCTs) and observational. The interventional studies evaluating vascular effects of electronic cigarettes essentially used various designs, which caused differences in the number of participants, type of electronic cigarettes used, nicotine concentration in electronic cigarettes, length of study, and employed vascular markers. The observational studies also varied in the number and characteristics of participants, e.g. smokers and nonsmokers.
Animal studies using mice models that evaluated the vascular-related effect of electronic and conventional cigarettes are all interventional. Similar to human interventional studies, the design used in the studies varied in the number of mice, the composition of electronic cigarette vapor, nicotine concentration, length of study, and observed vascular markers.
3.1. Effects on Vascular System
In human studies, despite the difference in the number of participants, nicotine concentration in electronic cigarettes, and length of study, all three RCT studies concluded that electronic cigarettes caused less development in arterial stiffness and endothelial dysfunction compared to conventional cigarettes [Reference George, Hussain and Vadiveloo11–Reference Ikonomidis, Vlastos and Kourea13]. In regards to the nicotine effect, only one study found that electronic cigarettes without nicotine had no better impacts on health than electronic cigarettes with nicotine [Reference George, Hussain and Vadiveloo11], while other studies did not focus on the effect of nicotine.
Four latest observational prospective studies provided level IIB evidences of adverse vascular effects related to electronic cigarette smokers compared to nonsmokers, including increased arterial stiffness (p = 0.003), development of carotid plaque (p < 0.0001), microvascular endothelial dysfunction, and reduced endothelial nitric oxide (eNOS) levels (2.6%; p = 0.018) that related with endothelial dysfunction [Reference Fetterman, Keith and Palmisano15, Reference Podzolkov, Bragina and Druzhinina17–Reference Sahota, Naidu and Jacobi19]. One study did not compare effects of using electronic cigarettes with nonusers but observed that the markers of platelet activation (29%; p = 0.04), oxidative stress (23%; p = 0.02), and endothelial dysfunction (16%; p = 0.02) of electronic cigarette users were lower than conventional cigarette users [Reference Oliveri, Liang and Sarkar16]. The study by Rader et al. [Reference Rader, Rashid and Nguyen18] became the only one reporting a more significant coronary microvascular endothelial dysfunction in chronic electronic cigarette smokers. Thus, the research demonstrated that electronic cigarette smoking leads to vascular damage significantly, compared with nonsmokers.
All interventional animal studies have differences in study design, particularly nicotine concentration and duration of the study. There is a consistent conclusion that there were unfavorable effects of electronic cigarette use [Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21–Reference Szostak, Wong and Titz26]. Observed adverse vascular outcomes as summed from those studies, including damaged endothelium-dependent and endothelium-independent vasodilation [Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21], increased oxidative stress [Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21–Reference Kuntic, Oelze and Steven23], increased inflammation [Reference Espinoza-Derout, Hasan and Shao22, Reference Li, Huynh and Cornwell24], increased endothelial dysfunction [Reference Espinoza-Derout, Hasan and Shao22, Reference Kuntic, Oelze and Steven23], development of atherosclerotic lesions [Reference Espinoza-Derout, Hasan and Shao22, Reference Li, Huynh and Cornwell24], and increased arterial stiffness [Reference Olfert, DeVallance and Hoskinson25].
The study by Kuntic et al. [Reference Kuntic, Oelze and Steven23] is also worthy to note as it is the only study that reported increased oxidative stress by NOX-2 mechanism within 5-days observation, the shortest period among other chronic animal studies. In contrast, one study specifically noted that the effect of electronic cigarettes on some vascular health markers, which included arterial stiffness, inflammation, and oxidative stress, was small to absent [Reference Szostak, Wong and Titz26]. Regarding the nicotine effect, two studies reported that more significant disadvantageous outcomes were observed in electronic cigarettes with nicotine than without nicotine [Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21, Reference Espinoza-Derout, Hasan and Shao22].
3.2. Other Adverse Events
There are other unfavorable health effects of electronic cigarette use indicated by observational human studies, including association with stroke [Reference Bricknell, Ducaud and Figueroa14] and myocardial infarction [Reference Vindhyal, Okut, Ablah, Ndunda, Kallail and Choi20]. Another adverse outcome from animals studies was observed by one study [Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21] in which electronic cigarette vapor caused the development of cardiac hypertrophy.
3.3. Risk of Bias Assessment
Risk of bias assessment was done according to the type of the included studies. Based on the assessment using RoB 2, two studies [Reference George, Hussain and Vadiveloo11, Reference Ikonomidis, Katogiannis and Kostelli12] have some concerns for bias and one study [Reference Ikonomidis, Vlastos and Kourea13] was judged as high risk for bias. The summary of this result is available in Table 2.
Table 2: Risk of bias assessment of 3 randomized controlled trial studies using RoB 2.

For observational study, the NIH Quality Assessment was used to determine the quality of studies. Table 3 shows the summary of the quality assessment. Two studies were judged as good [Reference Fetterman, Keith and Palmisano15, Reference Oliveri, Liang and Sarkar16], three studies were fair [Reference Bricknell, Ducaud and Figueroa14, Reference Podzolkov, Bragina and Druzhinina17, Reference Sahota, Naidu and Jacobi19], while two studies were deemed as poor [Reference Rader, Rashid and Nguyen18, Reference Vindhyal, Okut, Ablah, Ndunda, Kallail and Choi20].
Table 3: Risk of bias (quality) assessment of 7 observational (cross-sectional) studies using NIH Quality Assessment.

Animal studies were assessed with SYRCLE’s RoB as summarized in Table 4. Most studies have unclear to high risk of bias results, especially on items about randomization, allocation concealment, and blinding protocol.
Table 4: Risk of bias assessment of 6 animal studies using SYRCLE’s RoB.

Notes: In the SYRCLE’s RoB, ‘Yes’ indicates low risk of bias; No indicates high risk of bias; ‘Unclear’ indicates unclear risk of bias.
4. Discussion
This systematic review explored the vascular effect of the use of electronic cigarettes on humans and animals (mice). Overall, there are potential adverse effects on arterial stiffness and endothelial function from the use of electronic cigarettes [Reference Fetterman, Keith and Palmisano15, Reference Podzolkov, Bragina and Druzhinina17–Reference Sahota, Naidu and Jacobi19, Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21–Reference Szostak, Wong and Titz26], though a few studies noticed its more pronounced effect was attributable to the presence of nicotine [Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21, Reference Espinoza-Derout, Hasan and Shao22]. In addition, studies that compared the vascular effect of electronic cigarettes to conventional cigarettes showed consistent results in favor of electronic cigarettes [Reference George, Hussain and Vadiveloo11–Reference Ikonomidis, Vlastos and Kourea13, Reference Oliveri, Liang and Sarkar16, Reference Sahota, Naidu and Jacobi19, Reference Vindhyal, Okut, Ablah, Ndunda, Kallail and Choi20]. However, it does not provide clear evidence on whether electronic cigarette smoking is harmless to the vascular system.
Contact with combustion products of conventional cigarette is one of the primary sources of its harm [Reference Benowitz and Fraiman27]. Likewise, the unfavorable impact of e-cigarettes on vascular health found in both human and animal studies may possibly be related to the products of e-liquid heating. The heating of propylene glycol (PG) and glycerol (Gly) produces short-lived free radicals and concerning compounds including formaldehyde, acetaldehyde, and acrolein among other compounds that are detrimental when inhaled at certain concentrations [Reference Geiss, Bianchi and Barrero-Moreno28–Reference Jensen, Strongin and Peyton30]. Formaldehyde, acetaldehyde, and acrolein can generate oxidative stress and form adducts with protein, RNA, DNA, which impair cell function [Reference LoPachin and Gavin31, Reference Moghe, Ghare and Lamoreau32]. In some e-cigarettes, traces of tobacco-specific nitrosamines (TSNAs), volatile organic compounds, and metals are also found in their aerosol or vapor, which may exhibit toxicity [Reference Cheng8, Reference Goniewicz, Knysak and Gawron33, Reference Margham, McAdam and Forster34].
It is generally known that the electronic cigarette does not produce carbon monoxide (CO) as there is no tobacco combustion. However, recent studies showed otherwise by reporting the presence of potential carbon monoxide from electronic cigarettes. Son et al. [Reference Son, Bhattarai, Samburova and Khlystov35] also showed that several electronic cigarette brands emitted carbon monoxide, alongside carbonyls, in varying amounts between 0 to 30 μg/puff in a normal vaping condition. In the study by Casebolt et al. [Reference Casebolt, Cook, Islas, Brown, Castle and Dutcher36] the CO concentration can reach over 180 ppm after e-liquid is heated. Carbon monoxide can attach strongly to hemoglobin in the place of oxygen, which can result in reduced oxygen availability in blood. So far, there have been known cases of carbon monoxide reaching a toxic level that may lead to cardiovascular complications, including functional anemia, angina pectoris, congestive heart failure, increased ventricular ectopy, and reduced ventricular fibrillation threshold [Reference Benowitz and Fraiman27].
Nonetheless, exposure to harmful substances generated from heated e-liquid is known to be lower than from combusted tobacco leaf [Reference Eaton, Kwan and Stratton37]. Combusted tobacco leaf in conventional cigarettes generates more than 7,000 chemicals, which can still be highly varied depending on initial compounds inside the tobacco blends and whole cigarette components [Reference Benowitz and Fraiman27, 38]. The difference in generated products of e-liquid and tobacco leaf is evidence for smokers to switch from conventional cigarettes to electronic cigarettes [Reference George, Hussain and Vadiveloo11–Reference Ikonomidis, Vlastos and Kourea13, Reference Oliveri, Liang and Sarkar16, Reference Sahota, Naidu and Jacobi19, Reference Vindhyal, Okut, Ablah, Ndunda, Kallail and Choi20]. However, long-term exposure to the mentioned e-liquid heating byproducts, though in little amounts, still explains the health chronic effects that are supported by the rest of the studies [Reference Fetterman, Keith and Palmisano15, Reference Podzolkov, Bragina and Druzhinina17–Reference Sahota, Naidu and Jacobi19, Reference El-Mahdy, Mahgoup, Ewees, Eid, Abdelghany and Zweier21–Reference Szostak, Wong and Titz26].
Another explanation of the adverse effects of e-cigarettes possibly lie in the presence of nicotine. A study investigated nicotine exposure on smokers and found nicotine exposure by spray and smoking can induce short-term endothelial dysfunction [Reference Neunteufl, Heher and Kostner39]. In obese rats, nicotine administration caused a further rise in oxidative stress, inflammation, and endothelial dysfunction markers, probably by a pathway involving TNF-α [Reference Liu, Zhou and Li40]. Interestingly, two animal studies also provided histological results showing the development of atherosclerotic lesions from electronic cigarette with nicotine use [Reference Espinoza-Derout, Hasan and Shao22, Reference Li, Huynh and Cornwell24]. Using Oil Red O with hematoxylin and fast green staining, Espinoza-Derout et al. [Reference Espinoza-Derout, Hasan and Shao22] found notable development of atherosclerotic lesion area in the aortic root of mice exposed to 2.4% nicotine electronic cigarette vapor in contrast to saline treatment. Li et al. produced similar results using the same concentration of electronic cigarette vapor, showing increased atherosclerotic lesions in the whole aorta by Oil Red O staining and inside the aortic root by hematoxylin and eosin staining in mice in contrast to air-exposed mice. The effect of nicotine is also associated with atherosclerosis by causing inflammation.
Nicotine is known to induce the generation of inflammation-related factors, such as C-reactive proteins, which have a role in the development of atherosclerosis. An animal study by Catanzaro et al. supported that nicotine has contributed to the development of atherosclerosis as evident by the buildout of aortic lesions. Wu et al. concluded that nicotine stimulates ROS production and NLRP3 activation to possibly incite cellular pyroptosis after conducting an experiment on ApoE-/- mice and human aortic endothelial cells. Besides atherosclerosis, nicotine is thought to induce smooth muscle cells to proliferate by modulating angiotensin II. Angiotensin II is able to activate complex pathways, including Nox5 activation, ROS production, and inflammatory proteins, that eventually cause a rise in oxidative stress and endothelial dysfunction. These possible mechanisms may explain the more notable adverse outcomes observed in a few animal studies. Evidences gathered in this review indicate that chronic use of electronic cigarettes may lead to unfavorable effects on the vascular, especially elevation of oxidative stress and inflammation that impact vascular damage. So far, evidences on adverse events mostly come from nonrandomized observational and animal studies. Although there is a suggestion that electronic cigarettes are less harmful than conventional cigarettes, smoking an electronic cigarette still induces unbeneficial effects to the vascular system. Our study is in line with previous study about impact of electronic cigarettes on vascular damage as a risk factor of cardiovascular disease. Even though using an electronic cigarette is apparently safer than conventional cigarettes, previous research demonstrated that the molecular changes on the cardiovascular system clearly leads to oxidative stress and inflammation [Reference Espinoza-Derout, Shao and Lao41]. More studies about the impact of electronic cigarette smoking on the vascular system will describe the mechanism with more details.
The restriction of including only studies in the last five years was made to focus on updates from recent evidence regarding electronic cigarette effects on the vascular, nonetheless, a few studies also mentioned cardiac effects. Notwithstanding, this review still has limitations. The outcomes of included studies were highly diverse, thus making them unfit for meta-analysis. A descriptive review has been provided instead to summarize current updates on this topic.
5. Conclusion
Evidences from several RCTs seemingly support the popular belief that electronic cigarettes have less effect on the vascular system when compared to conventional cigarettes. However, exposure to electronic cigarettes can cause adverse effects, such as elevated oxidative stress, endothelial dysfunction, inflammation, arterial stiffness, and the development of atherosclerotic lesion. Future studies should broaden perspectives and reveal more about the mechanism of how electronic cigarettes impact the vascular system.
Conflicts of Interest
The authors have no conflict of interest to report.







