Introduction
The World Health Organization (WHO) is the United Nations Agency lead for directing and coordinating international health [1]. The WHO is grouped into six regions including the African region which is composed of 47 countries constituting its Member States, all of which are from the African continent (with the exception of African countries pertaining in the WHO Eastern Mediterranean region). The WHO African region is characterised by the largest infectious disease burden and the weakest public health infrastructures [Reference Kebede2], thus posing a threat to global health security [Reference Marinissen3].
Indeed, the rapidly growing global interconnectedness has led to the increased occurrence of emerging or reemerging infectious diseases with the potential to spread rapidly and affect populations across international borders. This has created the need for global solutions such as the International Health Regulations (IHR) adopted in 2005 [4]. The IHR (2005) aims to proactively develop public health systems that can prevent the spread of infectious disease and provide better containment mechanisms [4, Reference Wolicki5]. The IHR (2005) is a legally binding agreement according to which WHO Member States have the obligation to report all events that may constitute public health emergencies of international concern, including outbreaks of infectious diseases [4]. In order to help non-compliant nations to meet the IHR requirements, a new global health security agenda was launched in 2014 as an international collaborative partnership aiming to provide a more secure and safe world [Reference Wolicki5].
In the WHO African region, the 2014–2016 Ebola virus disease (EVD) outbreak in West Africa highlighted the significance of reducing the vulnerability of communities to threats of infectious diseases that spread across national borders [Reference Heymann6]. The late detection of this epidemic revealed the weaknesses of the disease surveillance systems in several African countries [Reference Marston7]. Since then, the WHO regional office for Africa has increased its efforts in supporting Member States to rapidly detect public health events (PHE) of international concern and rapidly implement effective public health actions. This is being done through the implementation of the integrated disease surveillance and response (IDSR) strategy by ministries of health [Reference Kasolo8] and the establishment of an epidemic intelligence unit at the WHO regional office. Epidemic intelligence is a conceptual framework within which the WHO can fulfil its mandate of strengthening surveillance and guiding public health control strategies in order to enhance health security [Reference Paquet9]. This process relies on the systematic collection and assessment of both structured data gathered from routine surveillance systems (indicator-based surveillance – IBS) and unstructured data gathered from formal and informal sources (event-based surveillance – EBS) in order to rapidly detect outbreaks.
The WHO supports countries to respond to outbreaks and other public health emergencies which are formally reported to the organisation. An internal grading system is used to determine the level of operational response required by the WHO, as part of its emergency response framework [10].
The purpose of this paper is to provide an overview of outbreaks of communicable diseases (epidemic prone diseases, diseases targeted for eradication or elimination and other major diseases of public health importance) reported in 2018 by the African region Member States to the WHO under the IHR, as well as to characterise their geographical spread, time to reporting to the WHO, burden of disease and need for the WHO and external support.
Methods
We conducted a retrospective descriptive analysis of infectious diseases outbreaks reported to the WHO from 1 January to 31 December 2018 by Member States of the WHO African region as part of their obligations under the IHR. The study was limited to 2018 due to insufficient completeness of variables on events reported to the WHO in previous years.
An event was defined as any public health emergency reported to the WHO by Member States according to their obligations under the IHR. Only events related to infectious disease outbreaks and officially notified to the WHO in 2018 were included in this study. Events related to humanitarian crises and natural disasters as well as events notified before 1 January 2018 and still ongoing in 2018, were excluded in order to include only events detected during the course of the year of study.
The data used were obtained from the PHE database maintained by the Health Emergency Programme of the WHO Regional Office for Africa, which contains records of all PHE formally reported to the WHO after detection by the Member States via IDSR, as well as those reported after detection through epidemic intelligence activities conducted at the WHO Regional Office for Africa (WHO AFRO) such as media monitoring using the Epidemic Intelligence for Open Sources (EIOS) system and the Hazard Detection and Risk Assessment System (HDRAS) [Reference Abdelmalik11, Reference Enderlein and Regmi12]. These systems allow the monitoring of a wide range of digital media sources to detect signals of potential PHE.
Variables captured by the database included country name, event name, event category, grade of the event according to the WHO internal grading mechanism [10], date of notification to the WHO, method of detection, date of onset of the index/first case, total case count, total death count and case fatality ratio (CFR).
The distribution of events over time, by country and disease category was analysed. Infectious disease outbreaks reported by Member States were classified into three events categories: epidemic prone diseases, diseases targeted for eradication or elimination and other major diseases of public health importance.
Epidemic prone diseases included any disease with the potential to cause a serious public health impact due to their ability to spread rapidly internationally, except for those targeted for eradication or elimination by a specific WHO programme (such as poliomyelitis and measles) [13]. Any other disease outbreak, which was not complying with the criteria of the two precedent categories, was classified as other major diseases of public health importance.
The distribution of events by grade, the median notification delay, the estimated number of people directly affected and the CFR with its associated 95% confidence intervals (95% CI), were also analysed.
The WHO grading of PHE consists of assigning to an acute event one of the following level of operational response required by the WHO [10]:
• ungraded: an event that is being monitored by the WHO but does not require an operational response by the organisation;
• grade 1: a single event that requires a limited response by the WHO and that can be managed with in-country assets.
• grade 2: a single or multiple country event that requires moderate response by the WHO and exceeds the capacity of the country office. The provision of support to the WHO country office is coordinated at the WHO regional office.
• grade 3: a single or multiple country event that requires major response by the WHO. The provision of support to the WHO country office is coordinated at the WHO Regional office with assistance from the WHO headquarters to coordinate organisation wide inputs.
The delay in notification was defined as the number of days between the estimated disease onset of the first or index case and the notification of the outbreak to the WHO. The estimated disease onset of the first or index case was found in the official declaration of the outbreak, the formal IHR notification or in the first situation report released by the affected WHO Member State.
Data were analysed using R version 3.5.2 [14] for statistical analysis and using ESRI 2017 ArcGIS Pro 2.1.0 [15] for geospatial analysis.
Results
Distribution and types of outbreaks of infectious diseases notified to the WHO in 2018
In 2018, a total of 96 new infectious disease outbreaks were reported across 36 (76.6%) out of the 47 Member States of the WHO African region. Uganda reported the highest number of events (n = 9, 9.4%) followed by the Central African Republic (CAR) (n = 6, 6.3%), the Democratic Republic of the Congo (DRC) and South Sudan (n = 5, 5.2% for each country). Figures 1 and 2 present, respectively, the number of new events of infectious disease outbreaks in 2018 and the geographical distribution of events per country. Eleven countries (top 11) reported at least four events: Uganda (9), CAR (6), DRC (5), South Sudan (5), Angola (4), Congo (4), Kenya (4), Liberia (4), Namibia (4), Niger (4) and Zimbabwe. Eleven other countries did not report any new outbreak of infectious diseases during the year 2018: Burkina Faso, Comoros, Cote d'Ivoire, Equatorial Guinea, Eritrea, Eswatini, Gabon, Lesotho, Sao Tome and Principe, Seychelles and Togo. During media monitoring no signals of potential outbreaks were captured from these 11 countries with zero event reported.
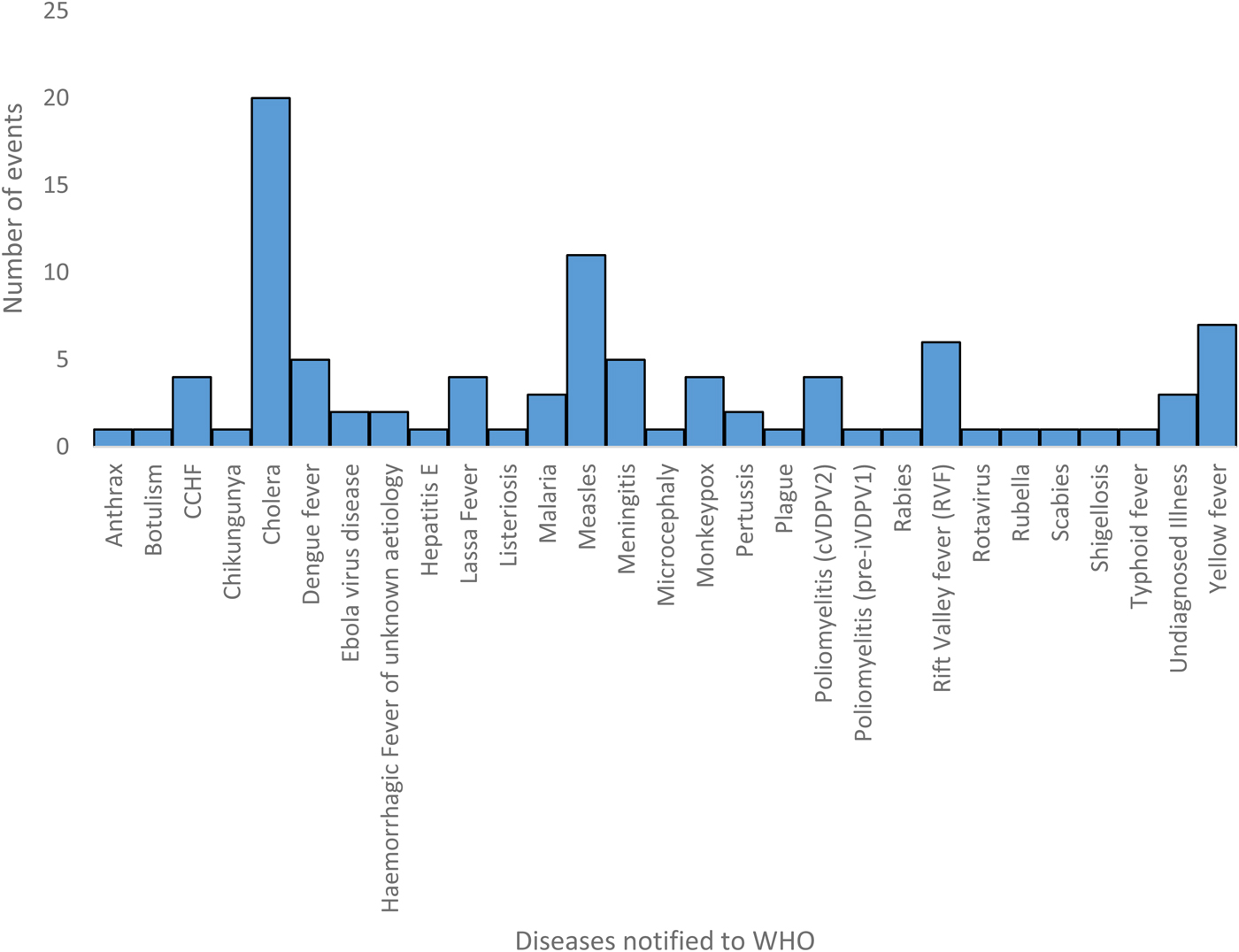
Fig. 1. Events of infectious disease outbreaks reported to the WHO by African's Member States (WHO African Region, 2018).
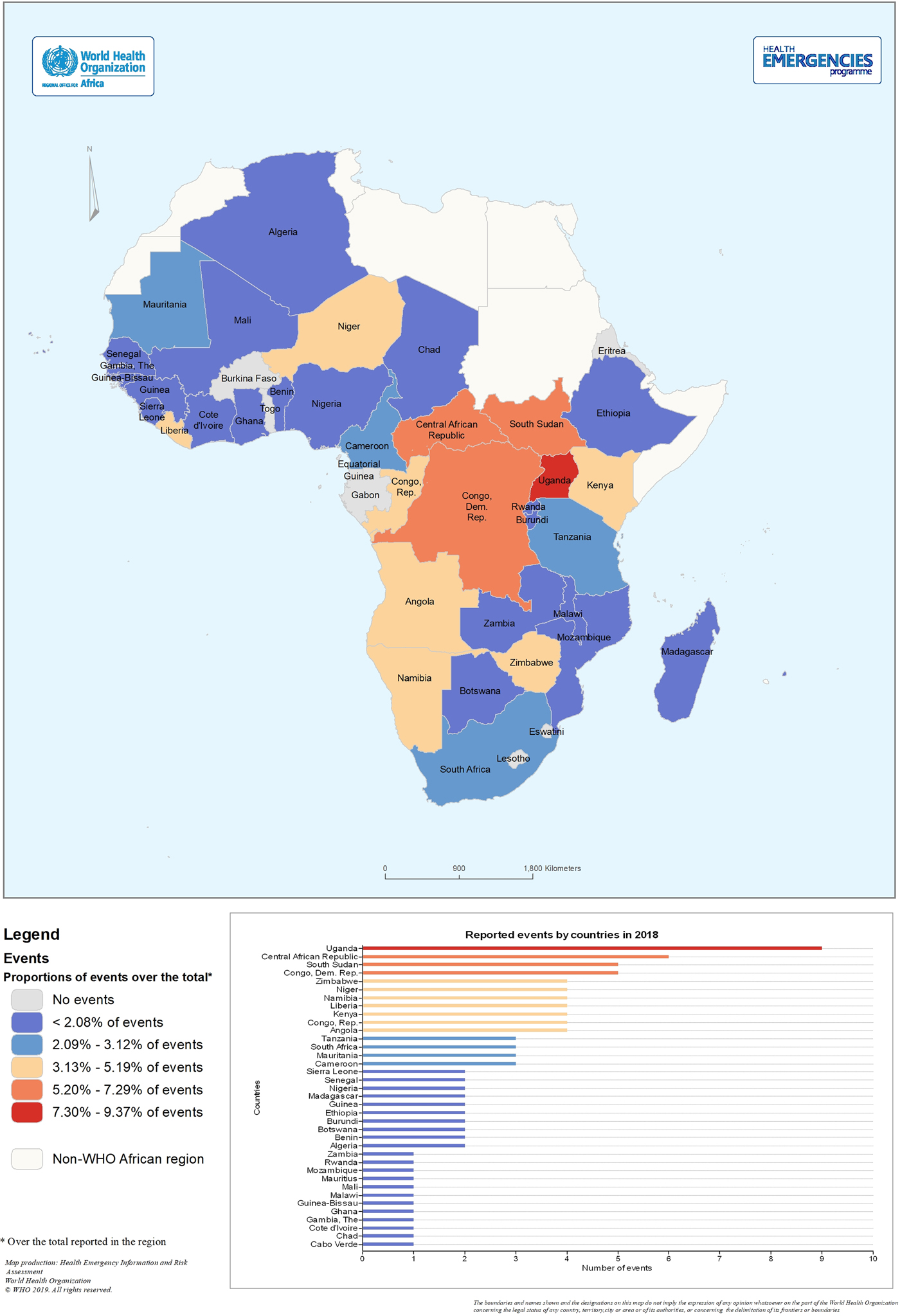
Fig. 2. Geographical distribution of outbreaks of infectious disease notified to per country (WHO African region, 2018).
Among the 96 infectious disease outbreaks reported, 82 were caused by epidemic prone diseases (85.4%), 6 by diseases targeted for eradication or elimination (6.3%) and 8 by other major diseases of public health importance (8.3%). Overall, 29 different diseases accounted for these outbreaks.
The most commonly reported disease outbreak was cholera which accounted for 20.8% of all events (n = 20 out of 96), followed by measles (n = 11, 11.5%) and Yellow fever (n = 7, 7.3%). Two EVD outbreaks were reported by the same country, the DRC. Table 1 shows the distribution of the number of events reported by type of infectious disease outbreak, grouped by event category.
Table 1. Diseases reported to the WHO by the African's Member States distributed by event category (WHO African Region, 2018)
Detection, notification and grading of outbreaks
Seventy-six percent of outbreaks (n = 73) were reported to the WHO following detection through routine surveillance activities conducted at the national level. About a quarter of events (n = 23), from 17 countries (including four from the top 11), were reported following signal detection through media monitoring conducted at the WHO regional office for Africa using either the EIOS or the HDRAS platforms, and subsequent verification of these signals by the country. The average number of events reported to the WHO per month was eight. Figure 3 shows the distribution of events notified to the WHO per month and event category.
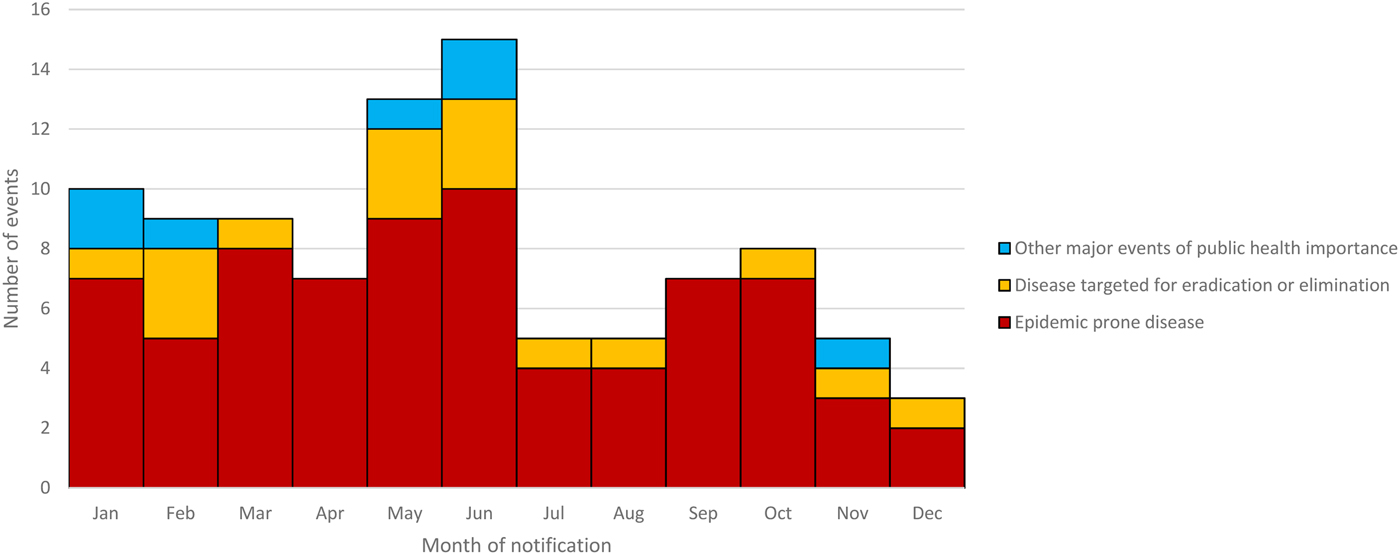
Fig. 3. Distribution of outbreaks of infection diseases notified to the WHO by African Member States by month of report and event category (WHO African Region, 2018).
Information on disease onset of the first/index case of each outbreak and the notification to the WHO was available for 86 out of 96 outbreaks. The median delay between the disease onset and the WHO reporting was 16 days (range: 0–184). Measles and poliomyelitis accounted for 29% (9/31) of disease outbreaks reported to the WHO more than 30 days after the symptoms onset of the index case. Figure 4 represents the distribution of delayed reporting to the WHO by event category.
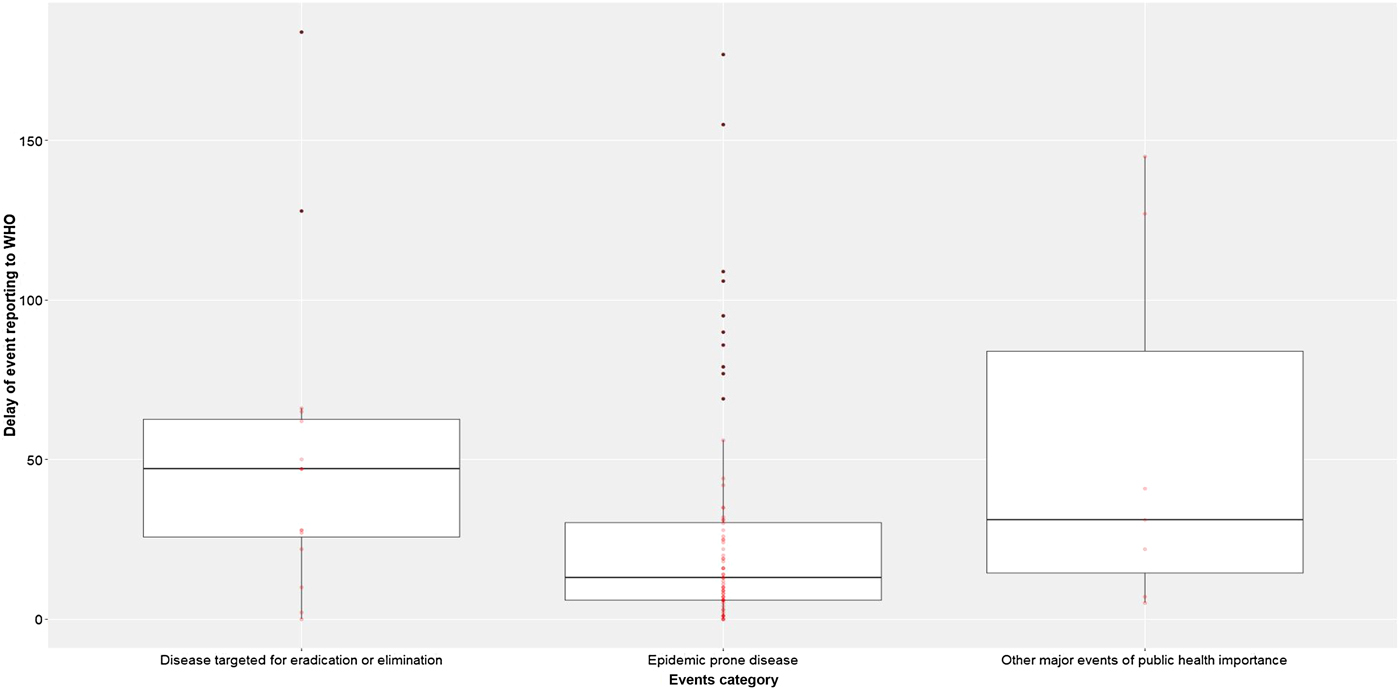
Fig. 4. Distribution of delay of event reported to the WHO by event category (WHO African Region, 2018).
The majority of the outbreaks of infectious diseases reported to the WHO were ungraded (n = 86, 89.6%) vs. 3.1% graded 1 (n = 3), 5.21% graded 2 (n = 5) and 2.1% graded 3 (n = 2). The two EVD outbreaks in the DRC were the only events graded 3 in 2018. Cholera accounted for 40% (n = 4) of graded events, including two grade 1 and two grade 2 events.
Morbidity and mortality due to outbreaks
Based on the final update of the PHE database on 31 December 2018, a total of 107 167 cases were directly affected by the 96 outbreaks, including 23 967 laboratory confirmed cases (37%). Epidemic prone diseases accounted for 89.7% of cases (n = 96 138). The mean CFR was 1.14% (95% CI 1.07%–1.20%) (n = 1221 deaths). The highest CFR was observed for diseases targeted for eradication or elimination: 3.45% (95% CI 0.89%–10.45%) compared to 1.23% (95% CI 1.16%–1.29%) for epidemic prone diseases and 0.36% (95% CI 0.26%–0.49%) for other major diseases of public health importance. Out of the 20 cholera outbreaks, 55% (n = 11) had a CFR which was above the tolerable threshold of <1%.
Discussion
In 2018, 29 different diseases accounting for 96 outbreaks were reported to the WHO by 36 out of 47 countries in the WHO African region. A review of outbreaks reported to the WHO from 2003 to 2007 identified only 16 different major diseases linked to outbreaks reported to the WHO by African Member States [Reference Kebede2]. This increase in the number and range of reported diseases might be linked to the revision, and subsequent implementation of IDSR guidelines in 2010 which included 43 diseases and conditions under surveillance [13].
Indeed, following the 2014–2016 West-Africa EVD outbreak, several African Member States have strengthened the implementation of the new IDSR strategy in order to improve early detection through routine surveillance [Reference Wu16–Reference Tambo, Ugwu and Ngogang18]. Several studies have reported improvements in disease surveillance in the African countries as a result of lessons learned from the 2014–2016 West Africa EVD outbreak [Reference McNamara17–Reference Ravi, Snyder and Rivers20]. Oppenheim et al. [Reference Oppenheim21] noted that West and Central African countries still have the lowest epidemic preparedness index. The latter assesses the capacity of institutions to detect, report and respond to outbreaks. In our study, we noted that most of the top 11 countries that reported outbreaks of infectious diseases in 2018 were classified as fragile states by the World Bank [22]. Previous studies have shown that epidemic surveillance and control appear to be insufficiently timely in fragile states and require strengthening [Reference Bruckner and Checchi23]. The World Bank describes a fragile state as a country ‘facing particularly severe development challenges such as weak institutional capacity, poor governance, political instability and frequently ongoing violence or the legacy effects of past severe conflicts’ [22]. According to Bornemisza O et al. [Reference Bornemisza24], the populations of fragile states are also highly vulnerable to infectious disease outbreaks, a reflection of inadequate government services and armed conflict-related phenomena such as forced displacement.
Among the top 11 countries having reported the most outbreaks in 2018, 10 had already conducted a voluntary joint external evaluation of IHR core capacities including eight assessed with developed or demonstrated capacities to detect public health threats as part of the IHR 2005 monitoring and evaluation framework [Reference Talisuna, Yahaya and Rajatonirina25] and two countries with limited capacities (Congo and Central African Republic). Our results have also shown that four countries among the top 11 reported events to the WHO following initial detection via media monitoring. Thus, suggesting the need to consider the implementation of a functional media monitoring mechanism, in addition to IBS and community based surveillance, among the criteria for assessing countries' capacity to rapidly detect outbreaks of infectious diseases.
Under the IHR (2005) WHO Member States have the obligation to immediately notify all events that may constitute public health emergencies of international concern, including outbreaks of infectious diseases [4]. In this study, the median number of days between the onset of the first case and the notification to the WHO was 16 days, indicating delays in the notification of events to the WHO. This delay was particularly noted among diseases targeted for elimination or eradication such as measles and poliomyelitis. We did not have complete or accurate data on the time between the onset of the first case and outbreak detection by the Member States. However, considering that, under the IHR, Member States are obligated to immediately report any PHE of international concern to the WHO [4], we considered the delays in reporting as a suitable proxy for the delays in detection. Therefore, our results indicate a need to strengthen the capacities for timely detection of outbreaks in the region. According to Morse SS [Reference Morse26], early detection requires robust surveillance and effective outbreak investigation capabilities in order to rapidly identify, characterise and monitor emerging infectious diseases. The WHO regional office for Africa must intensify its efforts to support Members States to develop more effective disease surveillance mechanisms. This is critical in order to achieve one of the targets of the WHO's 13 general programme of work (GPW13) [Reference Horton27]: one billion more people protected from health emergencies by 2023.
Apart from the IDSR weekly reporting established between the Member States and WHO, there is no monthly system for zero-reporting of PHE of international concern that may have been captured outside the formal IDSR reporting channels. Therefore, it was not possible to identify the reason why 11 countries of the WHO African region did not report any outbreak during the year 2018. Possible causes may include under-reporting, insufficient capacities to detect outbreaks of infectious diseases, or actual absence of outbreaks. There is a need for the WHO regional office for Africa, to not only continue to systematically conduct thresholds analyses of weekly IDSR data shared by Member States, but also to conduct an in-depth assessment of IHR core capacities in countries that are not reporting events, in order to ensure that adequate systems are in place for early detection of and rapid response to any PHE of international concern [Reference Suthar28]. In this study, most of the events reported by Member States (89.6%) were ungraded according to the WHO internal grading system [10], thus reflecting the existence of IHR core capacities within these countries and reinforcing the need, with WHO support, to continue to develop and maintain these capacities.
Nearly a quarter of events notified to the WHO in 2018 were reported by Member States following feedback on signals detected through media monitoring conducted at the WHO AFRO. This supports the fact that media monitoring may be utilised effectively as a mean to strengthen disease outbreak detection, notification and monitoring in this region.
Our results show that in 2018, cholera was the most prevalent cause of outbreaks in the region and accounted for the majority of graded events in the WHO African region. Furthermore, a significant proportion of cholera outbreaks had a CFR above 1%, which indicates either poor case management or lack of access to care. Our findings are in line with previous studies showing that cholera outbreaks represent a high morbidity and mortality burden in the African region [Reference Mengel29, Reference Ali30]. The high burden of cholera across the WHO African region Member States is explained by the fact that a significant proportion of the population in these countries is vulnerable due to conflict, food insecurity, poor socio-economic status, environmental conditions, inadequate access to safe water and sanitation, and limited access to health services [Reference Bwire31]. Furthermore, the ongoing and prolonged humanitarian crises in these countries drive population movements, thus facilitating the spread of the disease within and between countries as well as causing extensive deterioration of health, transport, shelter and water, sanitation and hygiene services [Reference Bwire32, Reference Kalipeni and Oppong33]. In this humanitarian context, country capacities to effectively implement cholera control measures are often limited. This is reflected in our results, showing that 20% (n = 4) of cholera outbreaks reported in 2018 required WHO and/or external support. While national cholera control strategies specific to each Member States' context may be useful, they are not sufficient to eliminate cholera on their own. For this purpose, the Global Task Force on Cholera Control (GTFCC) partners has launched, in October 2017, a global strategy to eliminate cholera by 2030 [34]. It is anticipated that the implementation of this strategy, which targets 47 cholera-affected countries, could result in the elimination of cholera as a public health threat from at least 20 countries as well as a 90% decline in the number of cholera-attributed deaths by 2030. Ensuring early detection and prompt comprehensive control measures to cholera outbreaks is crucial to achieving this goal.
The current study did not include outbreaks that were possibly not reported to the WHO in 2018. The threshold review of weekly IDSR reports submitted by Member States, has shown under-porting of some outbreaks, especially for endemic diseases such as malaria for most the African countries and Monkeypox in certain part of the DRC, Central African Republic and Nigeria. Therefore, the interpretation of the results of the current study should take this limitation into account.
Conclusion
The WHO African region remains prone to outbreaks of infectious diseases. Following the 2014–2016 West Africa EVD outbreak, several of the countries of the region have strengthened their disease surveillance systems. However, the IHR core capacities remain insufficient. It is therefore critical for the WHO regional office to intensify its support to Member States in improving capacities to rapidly detect and respond to PHE of international concern including outbreaks of infectious diseases. For this purpose, regional initiatives such as regularly assessing countries IHR core capacities and implementing a monthly zero-reporting mechanism for events of international concern, are essential. It is also important to integrate EBS activities such as media monitoring in the disease surveillance process, in addition to the IBS, as recommended by the IDSR strategy. The fact that cholera was the most prevalent cause of outbreaks in the region in 2018 recalls the need to accelerate the implementation of the global strategy to eliminate cholera.
Acknowledgements
The authors acknowledge the following groups and individuals for their contributions to this study: Ministries of Health and WHO Country Offices of the African Region which reported public health events in 2018, and the WHO Health Emergencies staff at the WHO regional office for Africa.







