Depression is a highly prevalent disorder with a large impact on quality of life and high economic costs. Reference Munoz, Cuijpers, Smit, Barrera and Leykin1 The 12-month prevalence of a depressive disorder in The Netherlands is estimated at 5.6% for ages 18–64 years. Reference Bijl, Ravelli and Van Zessen2 The most important risk factor for developing major depressive disorder is the presence of clinically relevant depressive symptoms. Reference Cuijpers and Smit3 Public mental health interventions targeting people with such symptoms are a promising strategy to reduce the prevalence of depression. These interventions can be successful, Reference Munoz, Cuijpers, Smit, Barrera and Leykin1 but recruitment is a challenge. Reference Cuijpers, Van Straten, Warmerdam and Van Rooy4 Web-based interventions provide an opportunity to overcome this challenge by tackling the reasons for low participation rates, such as stigma associated with mental disorders or restrictions in time. Reference Cuijpers, Van Straten, Warmerdam and Van Rooy4,Reference Andersson and Cuijpers5 Meta-analyses have shown that web-based interventions based on cognitive–behavioural therapy (CBT) are effective for the prevention of full-blown depression. Reference Arnberg, Linton, Hultcrantz, Heintz and Jonsson6,Reference Richards and Richardson7 One specific CBT intervention is acceptance and commitment therapy (ACT); Reference Hayes, Luoma, Bond, Masuda and Lillis8 this is an evidence-based treatment that focuses on promoting psychological flexibility, defined as the ability to act effectively in accordance with personal values even in the presence of life adversities. Reference Hayes, Strosahl and Wilson9 Despite the efficacy of ACT in various self-help formats, Reference Cavanagh, Strauss, Forder and Jones10 its efficacy as a web-based self-help intervention for adults with depressive symptoms or mild depressive disorder has not been studied. Our aim was to examine the effects of such an intervention in a large randomised controlled trial. This is the first study to compare this therapy not only with a waiting-list control but also with an active control condition based on expressive writing, Reference Pennebaker11 and to evaluate its outcomes up to a year later.
Method
The study was approved by an independent medical ethics committee for research in mental health settings in The Netherlands (METiGG; NL33619.097.100) and recorded in The Netherlands Trial Register (NTR1296). It is a pragmatic, randomised controlled trial with three arms: the ACT intervention, an active control condition (expressive writing) and a waiting-list control condition. Based on previous results randomisation was stratified according to gender, education (low v. middle–high) and age (≤50 v. ≤50 years), Reference Fledderus, Bohlmeijer, Pieterse and Schreurs12,Reference Bohlmeijer, Fledderus, Rokx and Pieterse13 using a computer-generated list that was concealed from the investigators. A sample size of 50 participants per condition was needed to detect an effect size of 0.40 (Cohen's d) for the primary outcome, Reference Fledderus, Bohlmeijer, Pieterse and Schreurs12,Reference Bohlmeijer, Fledderus, Rokx and Pieterse13 with a statistical power of (1−β) = 0.80 in a two-tailed test (P<0.05). Taking into account a drop-out rate of 40% (for web-based interventions), Reference Christensen, Griffiths and Farrer14 235 people were needed for randomisation. At 6 months after baseline those in the waiting-list control group received either the ACT intervention or the expressive writing intervention, which were offered as a choice. The assessment points were at baseline (T 0), post-treatment 3 months after baseline (T 1) and at 6 months (T 2) and 12 months (T 3) after baseline. Only participants in the intervention conditions received a follow-up measurement at T 3, since the waiting-list group received their intervention after T 2 and were excluded from later analyses.
Participants and procedure
Participants were recruited in January and February 2011 through advertisements in Dutch national newspapers and on the internet, asking for participation in research on coping with negative emotions through the use of a free web-based intervention. A webpage created for the purpose of this study included an outline of the study design and an option to register for participation in the trial. Within the webpage candidates filled out a secured computerised informed consent form. After informed consent had been received, initial screening was conducted online for checking the inclusion and exclusion criteria by use of a self-report questionnaire in a fully automated computerised assessment battery. Individuals were invited to participate if they met the following inclusion criteria: an age of 18 years or older with mild to moderate depressive symptoms, defined as a score above 10 on the Dutch version of the Center for Epidemiological Studies – Depression (CES-D) scale, Reference Fledderus, Bohlmeijer, Pieterse and Schreurs12 and completion of the baseline measurement (T 0). Applicants were excluded if they reported few depressive symptoms (≤10 on the CES-D), had received psychological or psychopharmacological treatment for a mental complaint within the past 3 months, had reading or writing problems due to insufficient Dutch language skills or were unable to invest approximately 30 min per day up to 3 h per week in the intervention and daily practice. Furthermore, applicants were excluded if diagnosed with a current severe mental disorder or had a moderate to high suicide risk according to the Dutch version of the Mini International Neuropsychiatric Interview (MINI) and the Sheehan Disability Scale (SDS). Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller15–Reference Leon, Olfson, Portera, Farber and Sheehan17 These individuals were excluded because they would require more intensive treatment, and were advised to consult their general practitioner. After passing the initial screening procedure all participants were contacted by telephone for a semi-structured interview using the MINI and the SDS. Together with the initial screening this constituted the baseline assessment. Five Master's degree students in psychology conducted the telephone interviews. They attended a 1-day workshop and were supervised during the assessments by a licensed clinical psychologist (W.T.M.P.). Decisions on participation in the study, based on the initial screening and the interview, were provided to the candidates at the end of the clinical interview with further information on participation or, when excluded, information on how to obtain adequate care. All approved participants received an email with instructions on how and when to log into the system.
All clinical interviewers were masked to the randomised condition. Participants were randomised after the clinical interview, and at T 2 the contact information needed for the clinical interview was held separately from the results of the randomisation procedure. Additionally, all interviewers were instructed to state explicitly at the start of the interview that they were unaware of which condition the participants were randomised to and that this masking was needed to ensure the interview was conducted in a non-biased manner.
Interventions
Acceptance and commitment therapy
The web-based ACT intervention was based on a self-help intervention, ‘Living to the Full’. Reference Bohlmeijer and Hulsbergen18 This has shown to be effective in promoting psychological flexibility, both as a group course and as a self-help intervention with email support. Reference Fledderus, Bohlmeijer, Pieterse and Schreurs12,Reference Bohlmeijer, Fledderus, Rokx and Pieterse13 People who are psychologically flexible also score highly on acceptance, which is seen as a more effective strategy for regulating negative emotions and thoughts than experiential avoidance, i.e. persistent and generally fruitless attempts to avoid unwanted private experiences such as feelings, thoughts and bodily sensations. Reference Kashdan and Rottenberg19,Reference Aldao and Nolen-Hoeksema20 The web-based intervention comprised nine online modules, divided into three parts. The modules were based on six core processes of ACT that together promote psychological flexibility. These core processes are acceptance (active and aware embracing of aversive internal experiences); cognitive defusion (creating a context in which undesirable functions of thoughts disappear); contact with the present moment (mindfulness); self as context (the sense of oneself as the observer of one's thoughts, feelings and experiences); values (choosing values in different life domains); and committed action (commitment to choices on the basis of these values). Reference Hayes, Strosahl and Wilson9 In the first part of the intervention participants reflect on their avoidance and control strategies and whether these are effective in the long run. In the second part participants learn how to stay in contact with their present experiences without trying to avoid or control them. Cognitive defusion and experiencing self as context are practised. In the third part the focus is on becoming aware of one's most important personal values and making decisions based on these values. An additional focus is relapse prevention, which includes self-management and action plans. Each module uses experiential exercises and metaphors to illustrate the ACT process, as well as text messages, tailored stories for motivation and an option to personalise the homepage. Furthermore, participants were encouraged to practise daily mindfulness exercises, designed to reduce stress. Reference Kabat-Zinn21 These exercises lasted on average 10–15 min and were provided on audio, downloadable within the web-based intervention. For a comprehensive description of the development of the intervention, see Kelders et al. Reference Kelders, Pots, Oskam, Bohlmeijer and Van Gemert-Pijnen22
Active control condition
The active control condition was a web-based intervention based on Pennebaker's expressive writing paradigm, Reference Pennebaker11 which has shown small effects on various mental health outcomes. Reference Frattaroli23 Expressive writing generally involves asking participants to write about a highly stressful experience (particularly their deepest thoughts and feelings), usually in three or four sessions. We extended and adapted Pennebaker's method into a web-based format equivalent to that of the ACT intervention, comprising nine online sessions presented in three parts. Each session started with a psychoeducational paragraph on emotions and emotion regulation, followed by instructions in the expressive writing method. This consisted of writing about emotional experiences for 15–30 min on at least 3 days a week. The first three sessions focused on expressive writing about negative experiences. In sessions four to six participants looked back at their experiences with expressive writing in the first part, and focused on emotion regulation and reappraisal of emotions; these modules were based on Gross's process model of emotion regulation, Reference Gross, Thompson and Gross24 and were added to extend the intervention to 9 weeks. In the last three modules of the intervention participants focused on writing about positive experiences and self-management for preventive purposes.
Waiting-list control
Participants in the waiting-list control group were offered no intervention but were free to access other forms of care (as were all participants once they were eligible). They were instructed that, should they encounter symptomatic deterioration or other difficulties over the course of the study, they were to seek help from their family, general practitioner or other sources, as they normally would. Six months after baseline these participants could start a web-based intervention of their choice. Based on the preliminary results of this study at T 2, the participants were advised to start with ACT.
Counselling
Participants in the web-based ACT and expressive writing interventions were instructed to complete one session per week, and had 12 weeks in total to complete the nine sessions. After completing a session, participants wrote an email to their counsellor reflecting on the process and using the opportunity to ask questions. They could proceed to the next session after receiving personal feedback from their counsellor. The feedback messages of the counsellors contained the key learning points and goals of the completed session, feedback on the key exercises and a preview of the following session. The feedback was accompanied by positive and encouraging support. Participants received automatic email messages when they completed a session, when personal feedback was received, and to remind them to finish a session or to start a new session. A session was fulfilled when all exercises were completed.
Five psychology Master's degree students provided the email support in both the experimental and the active control conditions. They attended a 2-day workshop from licensed doctors of clinical psychology with ample experience in CBT, ACT and expressive writing (K.M.G.S. and W.T.M.P.), in which they studied the web-based interventions and practised writing emails in the roles of both client and counsellor. Each counsellor provided personal feedback to 25–30 participants during the intervention, supervised by a clinical psychologist. The counsellors were given a total of 3 h on the counselling of an individual participant.
Assessment
The primary outcome measure was depressive symptoms measured by the Dutch version of the CES-D (20 items, total score 0–60). Higher scores mean more depressive symptoms. Reference Radloff25,Reference Haringsma, Engels, Beekman and Spinhoven26 Secondary outcome measures were diagnostic classification, anxiety symptoms, positive mental health, psychological flexibility and mindfulness. The diagnostic classification was assessed with the MINI, Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller15,Reference Van Vliet and De Beurs16 supplemented with the SDS to measure the severity of the disorder. Reference Leon, Olfson, Portera, Farber and Sheehan17 Severity was defined as at least two areas of functioning with severe role impairment due to the disorder according to the SDS. The MINI and SDS assessments were conducted by telephone at T 0 and T 2. Anxiety was measured with the Hospital Anxiety and Depression Scale – Anxiety subscale (HADS-A; 7 items, total score 0–21). Higher scores mean more anxiety symptoms. Reference Spinhoven, Ormel, Sloekers, Kempen, Speckens and Van Hemert27,Reference Zigmond and Snaith28 Positive mental health was measured with the Mental Health Continuum – Short Form (MHC-SF; 14 items, each scored 0–5), which measures three dimensions of positive mental health: emotional, social and psychological well-being. Reference Lamers, Westerhof, Bohlmeijer, Ten Klooster and Keyes29 In this study the total MHC-SF score was used, with higher scores indicating greater emotional, social and psychological well-being. Reference Lamers, Westerhof, Bohlmeijer, Ten Klooster and Keyes29,Reference Keyes, Wissing, Potgieter, Temane, Kruger and van Rooy30 The Acceptance and Action Questionnaire II (AAQ-II; 10 items, total score 10–70) was used to measure the participants' willingness to be in contact with negative private events, their acceptance of these events and the ability to live according to their values. Higher scores indicate greater psychological flexibility. Reference Fledderus, Oude Voshaar, ten Klooster and Bohlmeijer31,Reference Bond, Hayes, Baer, Carpenter, Guenole and Orcutt32 The Five Facet Mindfulness Questionnaire – Short Form (FFMQ-SF; 24 items, total score 24–120) was used to measure mindfulness in five dimensions: observing, describing, acting with awareness, non-judging and non-reactivity. Facet scores range from 5 to 25 (except for observing, which ranges from 4 to 20), with higher scores indicating greater mindfulness. Reference Baer, Smith, Hopkins, Krietemeyer and Toney33,Reference Bohlmeijer, Klooster, Fledderus, Veehof and Baer34
Statistical analysis
The Consolidated Standards of Reporting Trials (CONSORT) guidelines for randomised trials were followed, Reference Moher, Schulz and Altman35 and the analyses were done using SPSS version 20 for Windows. Intention-to-treat (ITT) analyses were performed using the SPSS Missing Value Analysis to impute all missing data on the continuous measures with the expectation–maximisation method. This method estimates the unmeasured data based on maximum likelihood estimates using observed data on all continuous outcome measures in an iterative process. Reference Dempster, Laird and Rubin36 To provide a comprehensive picture of the effects of the intervention, the outcomes were analysed based on ITT as well as for those completing treatment only. The completers group was defined as participants who completed at least the first six sessions, as these sessions of the ACT intervention dealt with each of the six ACT processes. One-way analysis of variance (ANOVA) and chi-squared tests were conducted to examine baseline differences between the ACT intervention and the two control conditions. To examine the differences between the conditions on all the outcome measures, a 3(group)×3(time) repeated measures ANOVA was used. In the case of significant timegroup interactions, post hoc analysis of covariance (ANCOVA) was used on the change scores of the outcome measures with baseline scores as covariates. To examine the change from T 2 to T 3 in the two intervention groups, a 2(group)×2(time) repeated measures ANOVA and paired t-tests were used. Differences in non-study treatment (participants receiving other forms of care during the trial) were analysed using chi-squared tests on the proportions of non-study treatment between the three conditions.
Effect sizes at post-intervention were calculated with Cohen's d using the means and the standard deviations of the measurements of the conditions. Cohen's d is calculated as
where

To interpret Cohen's d, effect sizes up to 0.49 were considered small, 0.50–0.79 moderate, 0.80–1.29 large and above 1.30 very large. Reference Cohen37 For the changes within the groups (T 2 v. T 3) Cohen's d was corrected for dependence among means by using the correlation between the two means. Reference Morris and DeShon38 Comparisons were two-tailed and interpreted with a significance of P<0.05.
Using the Jacobson & Truax method we determined the proportion of participants who made a clinically significant change on the CES-D from baseline to post-treatment. Reference Jacobson and Truax39 First, the reliable change was calculated with the reliable change index, calculated as
where x
1 and x
2 are the individual's post-test and pre-test scores and
S
diff is the standard error of difference between the two test
scores; S
diff can be computed directly from the standard error of
measurement S
E as
![]() , where
, where
![]() and rxx
is the test–retest reliability of the measure. Second, the
recovery criterion was defined as a post-treatment score below the cut-off
value of 16 for clinically relevant depressive symptoms. The score of 16 has
been established in previous research as the cut-off indicating the presence
of clinically relevant depressive symptoms.
Reference Beekman, Deeg, Van Limbeek, Braam, De Vries and Van Tilburg40,Reference Smit, Ederveen, Cuijpers, Deeg and Beekman41
A clinically significant change on the CES-D is thus defined as a
reliable change between the measurements and a post-treatment score below
16. Participants who had a clinically relevant change were coded 1 (implying
favourable treatment response, ‘success’) or 0 (‘failure’). The binary
outcome was used to calculate the odds ratio (OR) using logistic regression.
Based on the clinically significant change proportions, the number needed to
treat (NNT) was calculated.
Reference Cook and Sackett42
and rxx
is the test–retest reliability of the measure. Second, the
recovery criterion was defined as a post-treatment score below the cut-off
value of 16 for clinically relevant depressive symptoms. The score of 16 has
been established in previous research as the cut-off indicating the presence
of clinically relevant depressive symptoms.
Reference Beekman, Deeg, Van Limbeek, Braam, De Vries and Van Tilburg40,Reference Smit, Ederveen, Cuijpers, Deeg and Beekman41
A clinically significant change on the CES-D is thus defined as a
reliable change between the measurements and a post-treatment score below
16. Participants who had a clinically relevant change were coded 1 (implying
favourable treatment response, ‘success’) or 0 (‘failure’). The binary
outcome was used to calculate the odds ratio (OR) using logistic regression.
Based on the clinically significant change proportions, the number needed to
treat (NNT) was calculated.
Reference Cook and Sackett42
In addition to the clinically significant change, the effect on diagnosis assessed with the MINI and the SDS was analysed using logistic regression. We calculated favourable treatment response when a participant was free from depression or did not develop a diagnosed depression at T 2 (‘success’). This yields a binary outcome with failure coded as 0 and success as 1. This binary outcome was then used to obtain odds ratios and the NNT. Differences between the proportions of change within the diagnosis group were analysed using chi-squared tests for comparisons between the two intervention conditions and the waiting-list control.
Results
A total of 436 persons were assessed for eligibility, of whom 93 were excluded based on initial screening criteria (Fig. 1). Owing to a computer error, data concerning 43 of those excluded were not stored. Reasons for exclusion based on data for the other 50 persons were insufficient time to participate (34%, n = 17), few depression symptoms (28%, n = 14), current psychological or medication treatment (20%, n = 10), problems with the Dutch language (16%, n = 8) and age less than 18 years (2%, n = 1). A total of 343 participants met the initial screening criteria for inclusion and were contacted by telephone for a structured interview. On the basis of this interview 58 participants were excluded because of the seriousness of their disorder (n = 24), a high suicide risk (n = 23), current psychopharmacological treatment (n = 1) or refusal to participate (n = 10). A further 29 respondents could not be reached by telephone at the agreed time. Of the 256 included participants, 20 did not complete the baseline measurement. Hence a total of 236 participants were randomised.

Fig. 1 Study profile.
After randomisation two participants (one in each intervention group) did not start the intervention for unknown reasons. Twelve participants in the ACT group did not complete the intervention (attended fewer than six sessions), compared with 17 in the expressive writing group. The main reasons given for non-completion were personal problems and that the intervention was too time-consuming. Adherence was 84% for the ACT group, compared with 76% for the expressive writing group. In the ACT group 73% of the participants completed all nine sessions, compared with 63% in the expressive writing group; the difference was not significant (χ2(1,n = 149) = 1.87, P>0.05). Analyses of non-study treatment revealed no significant difference between the conditions: at T 1 χ2(2,n = 175) = 1.36, P>0.05; at T 2 χ2(2,n = 202) = 2.01, P>0.05. Treatment-completer analyses revealed similar results between completer and non-completer groups with regard to demographic variables and outcome measures. Also, per protocol analysis revealed similar outcomes. Therefore, only the results for the total sample on the imputed data are reported (with exception of the logistic regression of the diagnostic classification).
At T 1 (post-treatment for the intervention conditions) data were available for 199 participants (drop-out rates: ACT 13%, expressive writing 25%, waiting list 10%) and at T 2 (6-month follow-up for the intervention conditions and pre-intervention for the waiting-list condition) data were available for 205 participants (drop-out rates: ACT 11%, expressive writing 21%, waiting list 9%). At T 3 (12-month follow-up for the intervention conditions) data were available for 118 of the 149 participants (drop-out rates: ACT 13%, expressive writing 30%).
Baseline characteristics
Table 1 gives an overview of the participants' characteristics. Eligible participants had a mean age of 46.8 years (s.d. = 12.1, range 20–73), most were women (76%), and two-thirds (66%) had a high level of education. Mean baseline score on the CES-D was 26.73 (s.d. = 8.38). Of the 236 participants, 95 (40%) were diagnosed with a mood disorder. Owing to a programming error in the randomisation procedure the number of participants in each condition differed. There was no significant difference at baseline between the conditions for any of the demographic variables or outcome measures, indicating a successful randomisation, except for gender: χ2(2,n = 236) = 22.78, P<0.001. A comparison of the results based on the analyses with v. without gender as a covariate revealed similar results. Therefore, only the results without gender as covariate are reported (additional analyses with gender as covariate are available from the authors on request).
Table 1 Baseline characteristics of the participants
| Total (n = 236) |
ACT (n = 82) |
EW (n = 67) |
WLC (n = 87) |
|
|---|---|---|---|---|
| Age, years: mean (s.d.) a | 46.85 (12.06) | 45.15 (10.78) | 46.73 (12.65) | 48.54 (12.63) |
| Range | 20–73 | 21–69 | 20–69 | 21–73 |
| Gender, n (%) b | ||||
| Female | 179 (75.8) | 76 (92.7) | 40 (59.7) | 63 (72.4) |
| Male | 57 (24.2) | 6 (7.3) | 27 (40.3) | 24 (27.6) |
| Marital status, n (%) a,c | ||||
| Single | 81 (35.5) | 28 (36.4) | 21 (32.8) | 32 (36.8) |
| Living with partner | 147 (64.5) | 49 (63.6) | 43 (67.2) | 55 (63.2) |
| Nationality, n (%) a,c | ||||
| Dutch | 204 (89.5) | 68 (88.3) | 59 (92.2) | 77 (88.5) |
| Other | 24 (10.5) | 9 (11.7) | 5 (7.8) | 10 (11.5) |
| Education level, n (%) | ||||
| High a | 157 (66.5) | 55 (67.1) | 45 (67.2) | 57 (65.5) |
| Middle a | 75 (31.8) | 24 (29.3) | 22 (32.8) | 29 (33.3) |
| Low | 4 (1.7) | 3 (3.7) | 0 (0.0) | 1 (1.1) |
| Daily activities, n (%) a,c | ||||
| Paid job | 150 (65.8) | 57 (74.0) | 41 (64.1) | 52 (59.8) |
| No job | 78 (34.2) | 20 (26.0) | 23 (35.9) | 35 (40.2) |
| Primary diagnosis, n (%) | ||||
| No diagnosis a | 97 (41.1) | 36 (43.9) | 22 (32.8) | 39 (44.8) |
| Major depressive episode | 18 (7.6) | 7 (8.6) | 6 (9.0) | 5 (5.8) |
| Recurrent depression a | 61 (25.9) | 21 (25.6) | 21 (31.3) | 19 (21.8) |
| Dysthymic disorder | 5 (2.1) | 0 (0.0) | 3 (4.5) | 2 (2.3) |
| Other mood disorder | 11 (4.7) | 2 (2.4) | 4 (6.0) | 5 (5.8) |
| Anxiety disorder a | 44 (18.6) | 16 (19.5) | 11 (16.4) | 17 (19.5) |
| Comorbidity, n (%) | ||||
| Mood disorder a | 54 (22.9) | 22 (26.8) | 17 (25.4) | 15 (17.2) |
| Anxiety disorder | 3 (1.3) | 0 (0.0) | 3 (4.5) | 0 (0.0) |
| History of diagnostic classification, n (%) a | 55 (23.3) | 19 (23.2) | 11 (16.4) | 25 (28.7) |
ACT, acceptance and commitment therapy; EW, expressive writing; WLC, waiting-list control.
a. No significant difference between intervention and control condition (P>0.05).
b. Significant difference between intervention and control condition (P<0.05).
c. Owing to a computer error data on marital status, nationality and daily activities of 5 participants in the ACT group and 3 participants in the EW group were mistakenly deleted.
Outcomes
Means and standard deviations for all outcome measures at baseline, post-treatment and follow-up and the results of the repeated measures are presented in Table 2. Figure 2 shows the repeated measure ANOVA for the primary outcome measure, the CES-D score. For all outcome measures significant interactions were found, except for the mindfulness facets observing (F (2,233) = 2.38, P = 0.05) and acting with awareness (F (2,233) = 1.16, P = 0.33). Post hoc ANCOVA revealed that participants in the ACT intervention improved significantly more from T 0 to T 1 on all outcome measures compared with the waiting-list control group (all P<0.01), except for the mindfulness facet acting with awareness (P = 0.62). Compared with the expressive writing intervention post hoc ANCOVA revealed that participants in the ACT group improved significantly more from T 0 to T 1 on all outcome measures (all P<0.05), except for the mindfulness facets observing (P = 0.85), describing (P = 0.12) and acting with awareness (P = 0.63). No significant improvement was found from T 1 to T 2 for any of the conditions on any outcome measure.
Table 2 Outcome measure scores and repeated measures analysis of variance
| Score, mean (s.d.) | |||||
|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | Follow-up 1 | Follow-up 2 | F a | |
| CES-D | |||||
| ACT | 26.70 (8.02) | 14.68 (8.05) | 14.42 (9.78) | 15.07 (8.66) | 3.07* |
| EW | 27.07 (9.17) | 17.51 (7.87) | 16.06 (8.78) | 14.96 (9.59) | |
| WLC | 26.51 (8.16) | 19.34 (8.55) | 17.71 (10.72) | ||
| HADS-A | |||||
| ACT | 8.73 (3.01) | 6.15 (3.25) | 6.49 (3.57) | 6.28 (3.50) | 3.50** |
| EW | 9.20 (2.86) | 7.47 (3.23) | 7.22 (3.60) | 6.78 (3.44) | |
| WLC | 8.70 (2.99) | 7.82 (3.62) | 7.45 (3.76) | ||
| MHC-SF | |||||
| ACT | 2.47 (0.76) | 3.03 (0.89) | 3.05 (0.95) | 3.13 (0.94) | 2.70* |
| EW | 2.36 (0.75) | 2.74 (0.75) | 2.83 (0.83) | 2.90 (0.86) | |
| WLC | 2.45 (0.80) | 2.69 (0.86) | 2.84 (0.93) | ||
| AAQ-II | |||||
| ACT | 40.66 (8.07) | 47.74 (9.24) | 47.97 (10.28) | 48.86 (10.28) | 4.95*** |
| EW | 38.93 (6.88) | 44.15 (7.24) | 45.40 (8.11) | 45.72 (8.54) | |
| WLC | 40.37 (9.37) | 43.04 (9.60) | 43.82 (10.11) | ||
| FFMQ-obs | |||||
| ACT | 14.66 (2.96) | 15.80 (3.00) | 15.63 (2.88) | 18.86 (3.58) | 2.38 |
| EW | 14.14 (2.83) | 15.37 (2.54) | 15.37 (2.38) | 18.30 (2.87) | |
| WLC | 14.61 (3.18) | 14.99 (3.10) | 15.33 (3.01) | ||
| FFMQ-des | |||||
| ACT | 17.28 (3.68) | 18.67 (3.33) | 18.51 (3.80) | 15.73 (3.00) | 3.76** |
| EW | 16.81 (3.46) | 17.69 (3.47) | 18.16 (3.25) | 15.21 (2.47) | |
| WLC | 17.70 (3.22) | 17.69 (3.85) | 17.84 (3.90) | ||
| FFMQ-act | |||||
| ACT | 15.44 (3.74) | 15.66 (2.60) | 16.64 (3.49) | 16.49 (3.59) | 1.16 |
| EW | 14.67 (3.25) | 15.41 (2.85) | 15.80 (3.07) | 15.84 (3.56) | |
| WLC | 15.14 (3.69) | 15.30 (3.81) | 15.70 (3.80) | ||
| FFMQ-nj | |||||
| ACT | 13.84 (3.41) | 16.21 (3.41) | 16.21 (3.51) | 16.63 (3.73) | 3.80** |
| EW | 13.71 (3.13) | 15.14 (2.82) | 15.30 (2.85) | 15.53 (3.25) | |
| WLC | 13.84 (3.72) | 14.77 (4.29) | 14.44 (3.79) | ||
| FFMQ-nr | |||||
| ACT | 13.94 (3.41) | 16.83 (2.57) | 16.72 (3.16) | 16.80 (3.02) | 8.94*** |
| EW | 14.37 (3.06) | 15.90 (2.59) | 15.98 (2.55) | 16.15 (2.65) | |
| WLC | 14.38 (2.78) | 14.69 (3.39) | 15.11 (3.26) | ||
AAQ-II, Acceptance and Action Questionnaire II; ACT, acceptance and commitment therapy; CES-D, Center for Epidemiologic Studies - Depression scale; EW, expressive writing; FFMQ, Five Facet Mindfulness Questionnaire (obs, observing; des, describing; act, acting with awareness; nj, non-judging of inner experience; nr, non-reactivity to inner experience); HADS-A, Hospital Anxiety and Depression Scale – Anxiety subscale; MHC-SF, Mental Health Continuum – Short Form; WLC, waiting-list control.
a. Time × group analysis of variance.
* P<0.05,
** P<0.01,
*** P<0.001.
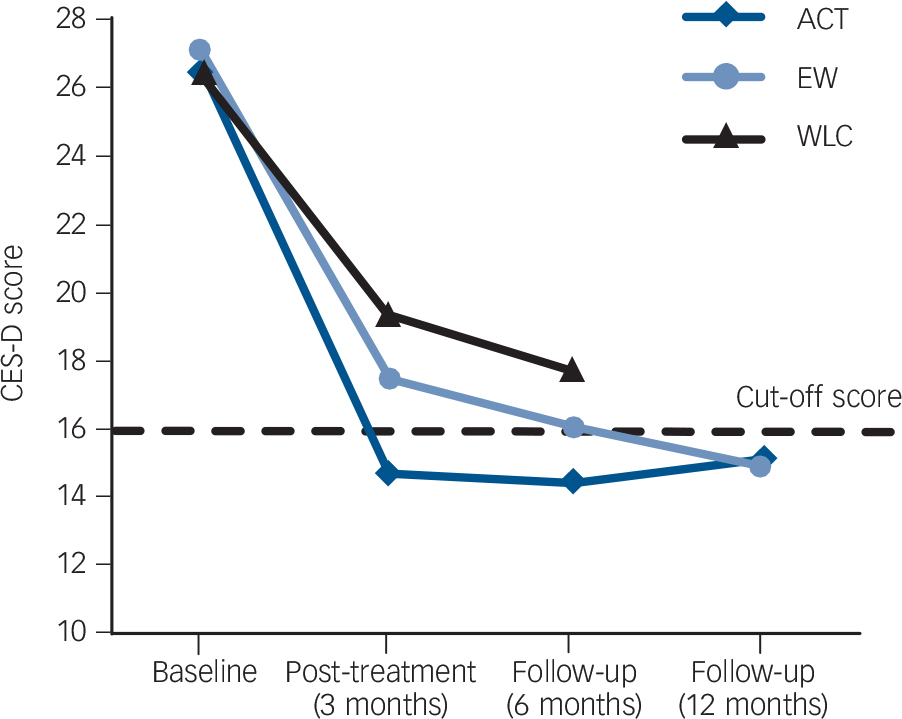
Fig. 2 Time×group repeated measures analysis of variance on Center for Epidemiologic Studies – Depression (CES-D) scores. ACT, acceptance and commitment therapy; EW, expressive writing; WLC, waiting-list control.
Additional analyses from T 0 to T 2 showed that the ACT intervention group improved significantly more on all outcome measures compared with the waiting-list condition (all P<0.05) except for positive mental health (P = 0.06) and the mindfulness facets observing (P = 0.34) and acting with awareness (P = 0.06). This indicates that the ACT intervention shows a significant improvement over time compared with the waiting-list condition. The expressive writing intervention group only showed a significant improvement from baseline to follow-up compared with the waiting-list condition for psychological flexibility and the mindfulness facets describing, non-judging of inner experience and non-reactivity to inner experience (all P<0.05).
In Table 3 the effect sizes between the conditions at post-intervention (T 1) and 6-month follow-up (T 2) are presented. At T 1 moderate and small effect sizes were found on all the outcome measures for the ACT intervention compared with the waiting-list condition, and small effect sizes compared with the expressive writing intervention. For the latter intervention small effect sizes were found compared with the waiting-list condition. At T 2 small effect sizes were found on all the outcome measures for the ACT intervention compared with the other two conditions. The expressive writing intervention also showed small effect sizes compared with the waiting-list condition.
Table 3 Effect sizes (Cohen's d) between conditions post-treatment and at 6-month follow-up
| Effect size | ||||||
|---|---|---|---|---|---|---|
| Post-treatment | 6-month follow-up | |||||
| ACT-WLC | ACT-EW | EW-WLC | ACT-WLC | ACT-EW | EW-WLC | |
| Primary outcome | ||||||
| CES-D | 0.56 | 0.36 | 0.22 | 0.32 | 0.18 | 0.17 |
| Secondary outcomes | ||||||
| HADS-A | 0.49 | 0.41 | 0.10 | 0.26 | 0.20 | 0.06 |
| MHC-SF | 0.39 | 0.35 | 0.06 | 0.22 | 0.25 | 0.01 |
| AAQ-II | 0.50 | 0.43 | 0.13 | 0.41 | 0.28 | 0.17 |
| FFMQ-SF | 0.50 | 0.38 | 0.19 | 0.43 | 0.29 | 0.20 |
AAQ-II, Acceptance and Action Questionnaire II; ACT, acceptance and commitment therapy; CES-D, Center for Epidemiologic Studies – Depression scale; EW, expressive writing; FFMQ-SF, Five Facet Mindfulness Questionnaire – Short Form; HADS-A, Hospital Anxiety and Depression Scale – Anxiety subscale; MHC-SF, Mental Health Continuum – Short Form; WLC, waiting-list control.
Effect maintenance
Repeated measures ANOVA revealed no significant difference between the ACT and expressive writing interventions on the change in outcome measures from T 1 to T 3. Also, within-group analyses showed no significant change for both interventions on all outcome measures. Overall, both interventions showed maintenance of the effects on the primary and secondary measures from 6 months to 12 months of follow-up.
Clinically significant change
The reliable change on the CES-D turned out to be a pre-treatment to post-treatment difference of at least 7 scale points. The proportion of participants who reached a clinically significant change post-treatment on the CES-D in the ACT intervention was 54% (n = 44) v. 26% (n = 23) in the waiting-list control group (OR = 3.22, 95% CI 1.69–6.14, P<0.001; NNT = 3.7). In the expressive writing intervention 21 (31%) reached a clinically significant change, resulting in a non-significant difference compared with the waiting-list control (P = 0.50). Comparison of the two interventions on clinically significant change post-treatment on the CES-D resulted in a significant difference in favour of ACT (OR = 2.54, 95% CI 1.29–4.98, P<0.01; NNT = 4.5). At 6-month follow-up no significant difference was found for the proportion of participants who reached a clinically significant change on the CES-D in the ACT (52%, n= 43) and expressive writing interventions (36%, n= 24) v. the waiting-list group (44%, n= 38). Comparison of the two interventions on clinically significant change at follow-up resulted in a significant difference in favour of ACT (OR = 1.98, 95% CI 1.02–3.83, P<0.05; NNT = 6.0).
Effects on diagnostic classification
Table 4 presents the results of the proportions of success for the MINI diagnoses (n = 204). Logistic regressions on the proportions of success were all non-significant, showing similar results of favourable outcome on the MINI. Chi-squared tests revealed significant proportional improvement in the diagnosis of recurrent depression for both ACT (χ2(1,n = 152) = 6.03, P<0.01) and the expressive writing intervention (χ2(1,n = 132) = 15.9, P<0.001) compared with the waiting-list condition. Comparison of the two interventions on proportions of improvement in the diagnosis of recurrent depression was non-significant (χ2(1,n = 124) = 2.83, P = 0.09).
Table 4 Improvement according to diagnostic category a
| Participants improved, n | ||||||
|---|---|---|---|---|---|---|
| ACT (n = 72) | EW (n = 52) | WLC (n = 80) | ||||
| Diagnosis | T 0 | T 2 | T 0 | T 2 | T 0 | T 2 |
| No diagnosis | 36 | 51 | 22 | 40 | 39 | 49 |
| Major depressive episode | 7 | 2 | 6 | 0 | 5 | 1 |
| Recurrent depression | 21 | 7 | 21 | 4 | 19 | 14 |
| Dysthymic disorder | 0 | 1 | 3 | 0 | 2 | 0 |
| Other mood disorder | 2 | 2 | 4 | 1 | 5 | 2 |
| Anxiety disorder | 16 | 9 | 11 | 7 | 17 | 14 |
ACT, acceptance and commitment therapy; EW, expressive writing; T 0, baseline; T 2, 6-month follow-up; WLC, waiting-list control.
a. As measured by the Mini International Neuropsychiatric Interview and the Sheehan Disability Scale at T 0 and T 2 based on per protocol analysis (n = 204; 86%).
Discussion
This is the first study to investigate the effects of a web-based ACT intervention for adults with mild to moderate depressive symptoms in a randomised controlled trial. The effects of the intervention were compared with a waiting list and an active control condition and were measured at post-treatment and at 6-month and 12-month follow-up. Overall, the results show that in the short term the ACT intervention was significantly more effective on the primary outcome measure and most of the secondary outcome measures than both the waiting-list control and the expressive writing intervention, but that both interventions had similar effects on depressive symptoms and secondary measures after 6 months and 12 months.
In comparison with the waiting-list control, participants receiving ACT showed significantly larger reductions of depressive symptoms post-treatment. The effect size at that point was moderate and at the 6-month follow-up it was small. The likelihood of a clinically significant change in depressive symptoms at the post-treatment assessment was substantially higher in the ACT group, compared with both the waiting-list (NNT = 3.7) and the expressive writing groups (NNT = 4.5). Moreover, comparison of the expressive writing and waiting-list control groups resulted in a non-significant difference. This outcome suggests that ACT was superior to both the active intervention and the waiting-list control in directly decreasing clinically relevant depressive symptoms. This is relevant, as the presence of such symptoms is the most important risk factor for major depressive disorder and is associated with considerable economic costs. Reference Cuijpers, Smit, Oostenbrink, De Graaf, Ten Have and Beekman43 Moreover, the ACT intervention resulted in significantly larger post-treatment reductions in anxiety and improvements in positive mental health in comparison with the waiting-list condition. The effect sizes were in the small range at post-treatment and in the small (non-significant) range at 6-month follow-up.
Interpretation of the findings
The findings at post-treatment are in line with findings from other studies of web-based interventions for adult depression. Reference Arnberg, Linton, Hultcrantz, Heintz and Jonsson6,Reference Richards and Richardson7 The smaller effects at 6-month follow-up appear to be largely due to further recovery in the waiting-list condition. An explanation could be that the waiting-list group anticipated starting the intervention directly after filling in the questionnaire at follow-up. The maintenance of the effect in the ACT intervention is similar to findings in earlier studies about the effect of ACT on depression. Reference Fledderus, Bohlmeijer, Pieterse and Schreurs12,Reference Bohlmeijer, Fledderus, Rokx and Pieterse13 Furthermore, this study shows that the effects of ACT were maintained at 12-month follow-up. Our results from the diagnostic classification analysis showed no significant difference in the proportions of success, meaning that in all conditions fewer participants were diagnosed with a mood disorder post-treatment. However, additional analyses showed a significant difference for both interventions on the diagnosis of recurrent depression compared with the waiting-list control. This finding suggests that both interventions may be especially effective for people with recurrent depression, but this needs to be interpreted with caution as our study was not powered for this. For the ACT intervention a possible explanation could be that mindfulness is a substantial component of the therapy. In all lessons participants are invited to meditate in order to increase awareness and acceptance of negative emotions and thoughts. It has been shown that meta-cognitive awareness, i.e. seeing thoughts as mental events that come and go, is an important process contributing to the prevention of the recurrence of depression in people with a history of depression. Reference Teasdale, Moore, Hayhurst, Pope, Williams and Segal44 As the participants in the ACT intervention showed a larger increase in mindfulness in comparison with the waiting list condition, this could explain the differential effects on recurrent depression at 6-month follow-up. However, these results must be interpreted with care and need to be supported by more research.
Effectiveness of expressive writing
Although it was found that the ACT intervention had larger post-treatment effects for depressive symptoms than the expressive writing intervention, no difference was found at follow-up. This was contrary to our hypothesis, in which we expected ACT to have a larger treatment effect both post-treatment and at follow-up. One explanation could be that the attention and emotional support through email contact in both interventions contributed to the effects. Another explanation is that expressive writing is also an effective treatment. Expressive writing has often been applied as an intervention, in which people write about emotional events on at least 3 days a week for 15–30 min for 3 or 4 consecutive days. Reference Pennebaker11 However, to make the format more equal to the ACT intervention the intervention was extended to 9 weeks. To enhance adherence to this longer intervention many components were added, one of which was psychoeducation on emotion regulation based on Gross's model. We found significant improvements from baseline to 6-month follow-up for the expressive writing group in psychological flexibility and the mindfulness facets describing, non-judging of inner experience and non-reactivity to inner experience compared with the waiting-list control. Writing about negative emotions for many weeks and writing about positive events may help people to regulate emotions in a way that is similar to ACT, i.e. diminishing avoidance and increasing acceptance of emotions. Some authors have suggested that emotional writing may yield larger effects, Reference Niles, Haltom, Mulvenna, Lieberman and Stanton45,Reference Nazarian and Smyth46 but there is no consensus on the mechanisms of change. Our findings suggest that a comprehensive expressive writing intervention could be an effective web-based intervention, but more research is needed to support this.
Adherence
Adherence to treatment was high, with only 13 out of 82 (16%) participants in the ACT group attending fewer than six sessions and 73% completing all nine sessions. The web-based intervention was designed using the Center for eHealth Research and Disease Management road map to achieve a user-friendly application that fits the values of the stakeholders and to evaluate the process of development. Reference Kelders, Pots, Oskam, Bohlmeijer and Van Gemert-Pijnen22 The high level of adherence in our study may indicate feasibility and compatibility with the wishes of our participants. Furthermore, effort was made to include persuasive technology in the design of the web-based interventions, as persuasive design has been shown to be positively related to adherence. Reference Kelders, Kok, Ossebaard and Van Gemert-Pijnen47
Strengths and limitations
A strength of our study is that the ACT intervention was compared not only with a waiting-list condition but also with an active control condition in the form of a web-based expressive writing intervention. Non-specific treatment factors such as attention and emotional support are generally recognised to be important for therapeutic effect. Reference Martin, Garske and Davis48 Also, inclusion criteria were kept broad to enhance generalisability with respect to the general population and the external validity of the study. Moreover, adding semi-structured interviews as diagnostic measures enhanced the reliability of the outcome measures. Finally, high attrition rates are common in studies of web-based interventions. Reference Eysenbach49 In our study treatment adherence was as high as 84%, in contrast to many previous internet studies that showed lower adherence rates. Reference Christensen, Griffiths and Farrer14
Some limitations also apply. The first and most important is that the recruitment strategy raises the possibility of self-selection bias (i.e. self-referral and motivation for time investment). This, and the fact that our participants tended to have high levels of education relative to the general public, raise questions on generalisability. It is a common finding in internet studies that highly educated women are especially prone to apply for guided web-based self-help interventions. Reference Eysenbach49 Second, there was no assessment of interrater reliability of the diagnostic classification in this study. However, previous studies have provided justification for this method of assessing psychiatric disorders. Reference Evans, Kessler, Lewis, Peters and Sharp50 A third limitation is the absence of competence measures of the counsellors because of the risk of not following the treatment protocol. However, all counsellors were supervised and the treatment protocol was highly standardised. Fourth, although we standardised the interventions to make them equivalent, the format of the interventions differed somewhat between treatments. The expressive writing intervention relied almost exclusively on text-based material, whereas the ACT used more experiential exercises (mindfulness exercises and interactive material) and relied more on a mix of text-based and picture-based material, which is in line with the theoretical underpinnings of the ACT model. Reference Hayes, Luoma, Bond, Masuda and Lillis8,Reference Hayes, Strosahl and Wilson9
Study implications
The clinical implications of this trial are that ACT can be effective as a web-based public mental health intervention for people with mild to moderate depressive symptoms, at least for women with medium to high levels of education. Although ACT was found to have larger effects than expressive writing in the short term, our findings also suggest that a comprehensive web-based expressive writing therapy might be a promising public mental health intervention. This needs to be corroborated in future studies.
Acknowledgements
We acknowledge with many thanks the therapists and participants who took part in this study.









eLetters
No eLetters have been published for this article.