To the editor:
In a recently published article, StahlReference Stahl 1 has expanded on the therapeutic potential of bupropion/dextromethorphan combination both for depression and agitation in Alzheimer’s disease as well. Dextromethorphan is NMDA glutamate antagonist, sigma-1 agonist, and serotonin reuptake inhibitors (SRI), and bupropion by inhibiting CYP 2D6 (for which dextromethorphan is a substrate) can prolong these actions besides norepinephrine–dopamine reuptake inhibitor (NDRI) mechanisms. With renewed interest in bupropion, some long upheld beliefs among prescribers might need to be demystified.
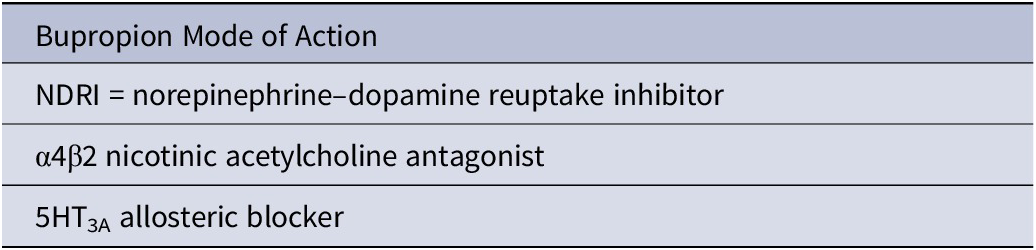
Bupropion, aminoketone, is an antidepressant with a unique composite mechanism of action (nonserotonergic)—an NDRI (Table 1). Only solriamfetol (FDA approved for narcolepsy and OSA) shares this mechanism.Reference Naguy, El-Sheshaie, Elsori and Alamiri 2 It is an alerting antidepressant (vs sedating, eg, mirtazapine), which can help melancholic depressed patients with anergia and adynamia. Due to demonstrated anti-inflammatory actions (anti-TNF-α), some data favor bupropion for depressed patients who are overweight with elevated CRP at baseline. It is procognitive- boosting nor-epinephrine (NE) and dopamine (DA) tone in prefrontal cortex, hence the use for comorbid ADHD in adolescents. These procognitive actions are comparable to vortioxetine, duloxetine, and escitalopram. It has nACh antagonistic actions, hence the use for smoking cessation (branded as Zyban), although inferior to valenicline but comparable to nicotine replacement therapy. Since DA is tied to hedonism, bupropion has been successfully used in patients with dual diagnosis (ie, major depressive disorder (MDD) and substance use disorder (SUD)). It is the only antidepressant approved for seasonal affective disorder (barring light therapy). It causes weight loss. In the same vein, it has been combined with naltrexone (branded as Contrave) and zonisamide (branded as Empatic) for obesity. Apart from occasional hypertension, bupropion has been shown to shorten QTc interval (akin to antipsychotic aripiprazole). WeReference Naguy and Alamiri 3 reported bupropion-induced QTc prolongation, however. It is less likely to induce manic shifts or rapid cyclicity (cf. TCA or SNRIs) and thus can be used in bipolar depression. It improves sexual functioning and is commonly used as SSRIs’ adjuventia for sexual dysfunction (related to 5-HT2A agonism). Moreover, bupropion is one of only few antidepressants that is unlikely to induce syndrome of inappropriate secretion of anti-diuretic hormone (SIADH) and hyponatraemia (particularly of concern in psychogeriatrics).Reference Teo and Mok 4
Table 1. Bupropion Mechanisms of Action.
Bupropion and Anxiety
Bupropion is believed to exacerbate anxiety and should not be prescribed in anxious depression. This is a myth. Truth is that in a meta-analysis,Reference Papakostas, Stahl and Krishen 5 with pooled individual patient data from 10 randomized, double-blind, placebo-controlled trials, to compare the efficacy of bupropion to SSRIs in treating anxious depression. No difference in timing or degree of improvement in anxiety symptoms between groups based on Hamilton Anxiety Scale or Hamilton Depression Rating Scale—Anxiety-Somatization (HDRS-AS) scores, was found. Moreover, in a pilot-controlled trial of bupropion XL vs escitalopram in GAD, bupropion demonstrated comparable anxiolytic efficacy to escitalopram and was well tolerated.
Bupropion and Psychosis
Since bupropion is structurally related to amphetamines and enhances dopamine neurotransmission, bupropion may, theoretically, induce or unmask psychosis. Such cases abound in literature. But close scrutiny reveals that bupropion-induced psychosis appears to be dose-dependent and that it occurs primarily in patients with certain risk factors—namely old age, overdose, SR formulation, substance use, using other dopaminomimetic drugs, and pre-existing psychotic symptoms. A systematic review of literature casted doubt on bupropion’s psychotomimetic potential. Interestingly, bupropion has been used to address clozapine-induced sialorrhea without psychotic decompensation.
Bupropion and Abuse Potential
Bupropion, originally designated as amfebutamone (note the prefix), is amphetamine-like in structure and can test false positive in Utox screen for amphetamines. An older, but closely related antidepressant, a DRI, amineptine (branded as Survector), was suspended from market for abuse potential (and also hepatotoxicity). Although this could be in part true for bupropion, given reports of crushed and snorted tablets among prisoners (referred colloquially to as poor man’s cocaine), bupropion increases DA in prefrontal cortex (PFC) and not in nucleus accumbans, hence no addiction potential. Moreover, for this reason, bupropion is commonly prescribed for dual diagnoses (vide supra).
Bupropion and Seizures
A common contraindication to use bupropion is history of seizures and eating disorders. There is a 10-fold increase in seizure with immediate release (IR) formulation at higher doses. Eating disorders are commonly complicated by dyselectrolytaemia, which further increases risk. With slow-release (SR)/extended-release (XL) formulations and newly introduced bromide-salt bupropion (branded as Aplenzin vs hydrochloride-salt Wellbutrin), this is no longer the case. That said, bupropion can exacerbate tics.
Disclosure
The authors have no competing interests or financial affiliations.



