INTRODUCTION
Measles is an acute respiratory infection that is caused by the measles virus. It was one of the most common infectious diseases in children and millions of children died from measles-related complications each year [Reference Drutz1, Reference Atkinson, Wolfe and Hamborsky2]. Widespread use of measles vaccine has led to a substantial decrease in measles incidence and measles-related mortality [Reference Simons3, Reference Mulholland, Griffith and Biellik4]. Unfortunately, measles remains common in underdeveloped countries and has been estimated to cause more than 100000 deaths each year worldwide [Reference Simons3]. Even in developed countries, substantial outbreaks have occurred in recent years [Reference Poland and Jacobson5]. In 2011, 30567 cases were reported by the 29 European countries [6]. These outbreaks have also affected the USA as a result of importation [7].
Similar to the experience of other countries, the incidence of measles in China decreased markedly following the widespread use of measles vaccine in the 1970s. The measles vaccine (a monovalent measles vaccine) is included in the Chinese National Expanded Programme on Immunization (CNEPI) and is offered to all eligible children free of charge. The first measles vaccine is administered to infants aged >8 months and the second should be given at age 4–6 years before entry into primary school [Reference Lixia8]. By the end of the last century, the incidence of measles in China decreased to 5·7/100 000 [Reference Lixia8]. With the success of the measles vaccine, the WHO and the Chinese government set a goal of measles elimination by 2012 [Reference Ma9]. However, in Wenzhou, we have observed that measles continues to be a major problem in the new century. The aim of this observational study was to examine the epidemiological and clinical characteristics of measles in the new century and to explore the causes of measles persistence in Wenzhou.
MATERIALS AND METHODS
Surveillance and clinical data collection
As a class B reportable disease, suspected measles cases in China are usually reported through the National Notifiable Disease Reporting System (NNDRS). The NNDRS, which was established in the 1950s, reports basic epidemiological data including age, sex, date of disease onset, and residence on all clinically diagnosed measles cases [Reference Lixia8, Reference Ma9]. This system is implemented primarily by local county health departments. The Wenzhou Municipal Center for Disease Control and Prevention (MCDCP) is responsible for data collection in the region.
Wenzhou had a total population of 7·5576 million in 2000, which grew to 9·1221 million by 2010 [10]. We calculated the population data for other years based on the growth rate reported by the government. These calculated populations for each year were used as the denominators for the calculation of disease incidence. The data of hospitalized measles patients were prospectively recorded as part of the measles control programme in the region. When hospitalization was needed for a particular measles patient, the infectious disease ward of Yuying Children's Hospital of Wenzhou Medical College was the designated place where children with measles were admitted for isolation and treatment. Detailed hospitalization data were also retrieved from the medical records and the immunization status of individual patients was obtained from the available immunization card.
Measles diagnosis and serology testing
The WHO and the US Center for Disease Control clinical case definition was used for all reported measles cases, i.e. any person with fever and a generalized, characteristic maculopapular rash lasting ⩾3 day, and with at least one of coryza, cough, or conjunctivitis [11]. Confirmatory serological testing was performed on all hospitalized patients with suspected measles by measuring specific measles IgM antibodies using a WHO-recommended measles-specific enzyme-linked immunosorbent assay (ELISA; Virion-Serion, Germany). To determine if infants in the region were susceptible to measles, random cord blood samples were collected from the hospital delivery room after normal deliveries from 1 January 2011 to 30 June 2011, and in addition, serum samples from normal infants at age 6 months were collected for the same period during their visits to the outpatient clinic for routine evaluation, for which written consent from the parents was obtained. A commercially available ELISA kit (Yanhui Biotechnology Company, China) which has a detection threshold of 0·3 IU/l was used for measurement of measles-specific IgG antibody concentrations according to the manufacturer's instructions. This study was approved by the Ethics Committee of The Second Affiliated Hospital and Yuying Children's Hospital of Wenzhou Medical College.
Statistical analysis
The χ 2 test was used for categorical data. All numerical data are presented as the mean and standard deviation. P < 0·05 was considered statistically significant in all cases. All statistical analysis was performed using SPSS v. 13.0 (SPSS Inc., USA).
RESULTS
Measles cases reported in Wenzhou, 2000–2010
There were 13271 clinically defined measles cases reported to Wenzhou MCDCP from 1 January 2000 to 31 December 2010. As shown in Figure 1, the measles outbreak occurred every 3–4 years in Wenzhou with a peak incidence of 38/100 000 in 2008. The age distribution of those reported cases is shown in Figure 2. Forty-five per cent of the reported measles cases in Wenzhou in the last decade were infants aged <1 year and 27·2% of the cases were individuals aged >14 years. Only 24·2% of the measles cases were children aged 1–7 years.
Fig. 1. Number of reported measles cases and the incidence of measles in Wenzhou, 2000–2010.
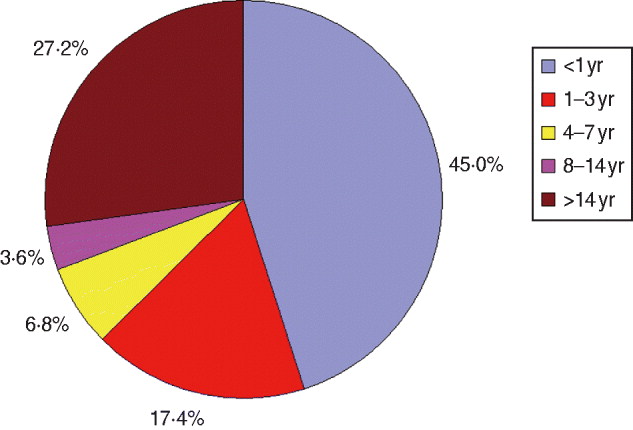
Fig. 2 [colour online]. The age distribution of reported measles cases in Wenzhou, 2000–2010.
Immunization history of the hospitalized measles cases
Of the 13271 reported cases, 2262 were hospitalized and also serologically confirmed. The number of measles cases known to be hospitalized each year from 2000 to 2010 is presented in Figure 3. The age distribution of these hospitalized cases is shown in Figure 4. Half (49·8%) of the known hospitalized cases were aged <1 year, and the youngest infant diagnosed with measles was just 17 days old. The age distribution for the hospitalized measles cases aged <1 year is shown in Figure 5. As can be seen, during the period from 2000 to 2010, the number of measles cases in Wenzhou region requiring hospitalization increased from birth up to age 8 months and declined thereafter. Furthermore, while 27·4% of the population was defined as being migrant population in Wenzhou, 58% of our hospitalized measles cases were from migrant families based on their birthplace record. The measles vaccination status of all hospitalized measles cases in different age groups is presented in Figure 6. Of the hospitalized measles patients aged >8 months (n = 1476 cases), 21·6% had been immunized with at least one dose of measles vaccine, 44·0% (649 cases) had never been immunized with measles vaccine, and 34·4% had an unclear history of measles immunization. The majority of those immunized received one measles vaccination while only six patients received two doses of immunization as documented on their immunization card. Of the 649 cases who had never been immunized with measles vaccine, the migrant population accounted for 76·0% (493/649) of cases.
Fig. 3. Number of hospitalized measles cases in Wenzhou, 2000–2010.
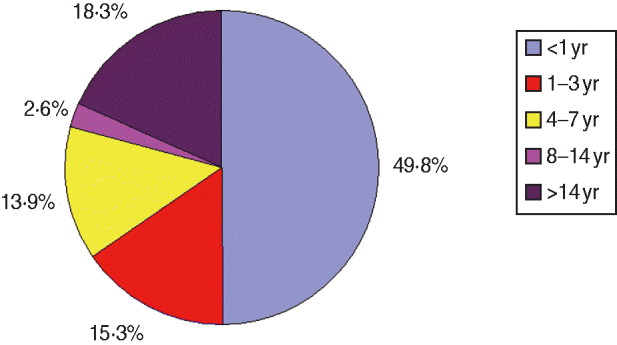
Fig. 4 [colour online]. The age distribution of hospitalized measles cases in Wenzhou, 2000–2010.
Fig. 5. The age distribution of hospitalized measles cases aged <1 year.
Fig. 6. The measles vaccination status of all hospitalized measles cases in different age groups.
Measles complications
Patients with measles were hospitalized primarily for acute complications. The most common indication for hospitalization was pneumonia (66·3% of the hospitalizations). Of these, three cases died from respiratory failure due to acute respiratory distress syndrome (ARDS) despite maximal supportive care in hospital. Other common causes for hospitalization included hepatitis (8·7%), encephalitis (5·2%), laryngitis (5·3%), diarrhoea/enteritis (2·2%), and other causes such as dehydration due to high fever.
Infant maternal measles antibody concentrations
To determine measles immunity in infants, we obtained 50 random cord blood samples from healthy full-term newborn infants delivered in the hospital and an additional 50 random serum samples from healthy infants aged 6 months. The mothers of all these infants had been immunized with measles vaccine and none had a documented history of measles. The measles-specific IgG antibody levels were quantified by using a commercially available ELISA kit. A level of ⩾125 IU/l is usually assumed to be protective [Reference Samb12]. The individual and mean serum measles-specific IgG levels in the neonatal group and the 6 months age group are shown in Figure 7. By using ⩾125 IU/l as the cut-off, 94% [95% confidence interval (CI) 87–100] neonates at birth had protective measles IgG antibody levels, while only 18% (95% CI 7–29) of infants at age 6 months had protective measles IgG antibody levels in their serum (χ 2 = 55·6, P < 0·01). These data suggest that, when born to a mother who was immunized with measles vaccine and without a natural history of measles, over 80% of infants may be susceptible to measles by age 6 months.
Fig. 7. The individual and the mean serum measles-specific IgG levels in normal newborns and 6-month-old infants.
DISCUSSION
We have demonstrated, in the current study, that during the last decade measles outbreaks continued to occur in the Wenzhou region every 3-4 years, mainly affecting infants aged <1 year and those aged >14 years. A similar phenomenon has been reported in recent measles outbreaks in other localities, including European countries, with a significant number of infants aged <1 year and older individuals being infected [Reference Goodson13–Reference Cottrell and Roberts17].
The patients requiring hospitalization were more often aged <1 year. It is known that measles in young infants has severe consequences and a much higher mortality rate, especially in resource-poor developing countries [Reference Aaby18, Reference Aaby19]. The measles virus weakens the immune system and results in a greatly increased susceptibility to opportunistic infections [Reference Slifka20]. Pneumonia was found to be the most common lethal complication of measles [Reference Beckford, Kaschula and Stephen21]. Indeed, the leading cause for measles hospitalization in the Wenzhou region was pneumonia complicating measles in infants aged <1 year. Almost two thirds of the hospitalized measles patients had pneumonia, of whom three cases died from ARDS.
Despite a relatively high reported vaccine uptake in Wenzhou region, a sufficient pool of local and migrant children who did not receive scheduled measles immunization remained to maintain measles persistence. Almost half of the hospitalized measles cases who should have been immunized had not received their first measles vaccination. The measles vaccine is offered to all eligible children free of charge in China. The first measles vaccine is administered to infants aged >8 months and the second given at age 4–6 years before entry into primary school [Reference Lixia8]. When a child is born in China, the parent of the child is required to register the child at the local immunization centre within the first month of life for scheduled immunizations. The children's immunization status is reinforced by periodic province-specific supplementary immunization activities (SIAs) [Reference Ma9, Reference Guo22]. However, this system is facing a major challenge as an increasing number of families move to other places for socioeconomic reasons [Reference Guo22]. For those families, if parents fail to re-register their children at the new local immunization centre, the children drop out of the system and usually do not receive the appropriate scheduled immunization. Indeed, 58% of our hospitalized measles patients were defined as being migrant, based on their birthplace record. Furthermore, in the hospitalized measles patients aged >8 months who had never been immunized with measles vaccine, 76% were from the migrant population. In December 2007, a survey of 1543 children of the migrant population in Wenzhou region demonstrated that only 80·2% of the children aged 1-7 years had received measles vaccine [Reference Lin23]. More recently, a small-scale survey on 450 children (225 children of local residents, 225 migrant children) demonstrated that the low measles vaccination rate in the migrant children population had improved overall by 2011, compared to that reported in 2007. The vaccination rate for measles was 91·56% for migrant children compared to 97·33% for local children [Reference Huang24]. The low coverage rate of measles vaccine in the migrant population during that period was probably one of the major causes of persistent measles outbreaks in the Wenzhou region. This is in agreement with a report that low vaccine coverage and the movement of unvaccinated children into a specific area were the main risk factors for measles after a mass vaccination campaign in Burkina Faso [Reference Yameogo25].
Of those hospitalized for measles, some had been immunized previously with measles vaccine, indicating vaccination failure. The majority of those had only received one dose of vaccine presumably before age 1 year. It is well known that the presence of maternal antibodies and the immaturity of the infant immune system for adequate humoral immune reaction to life vaccines can have an influence on the success rate of measles vaccination [Reference Albrecht26]. A previous study demonstrated that immunization with measles vaccine in infants born to vaccine-immune mothers at age 6 months induced measles neutralizing antibodies in only 74% of infants. Primary seroconversion rates were 100% for 15-month-old infants [Reference Johnson27]. In the post-vaccine era, between 74% and 80% of infants vaccinated between ages 6 and 9 months respond to vaccine, and around 67% have clinical protection from measles vaccination [Reference Manikkavasagan and Ramsay28]. It was therefore recommended by the American Academy of Pediatrics that if a child receives a dose of measles vaccine before age 12 months, two additional doses are required beginning at age 12–15 months and again at age 4–6 years [29]. This strategy should be implemented in China with two doses of measles vaccine being administered to every child, and the dose given before the age of 12 months should not be counted. In fact, a revision of the current Chinese National Immunization Programme has been made and the second dose of measles vaccine has been offered to children at age 15 months in Wenzhou in recent years [Reference Huang24].
In the current study, a large proportion of reported measles cases were in infants aged <1 year, and significant numbers of those hospitalized were aged <8 months. The number of measles cases in Wenzhou region requiring hospitalization increased from birth to 8 months when infants started to be immunized with measles vaccine. Prior to the measles vaccine era, infants were usually protected from the disease by passively transferred maternal antibodies against measles. The waning of maternally derived protection in the current vaccine era may explain an increasing proportion of infants being susceptible to measles before the age of measles vaccination [Reference Manikkavasagan and Ramsay28, Reference Leuridan30]. Indeed, our serological data from normal infants strongly suggest that by age 6 months, a large proportion of infants born to mothers who were immunized with measles vaccine may be susceptible to measles based on measles-specific IgG antibody levels.
Measles is thought by many experts to meet biological criteria deemed necessary for eradication of an infectious disease [Reference Moss and Strebel31]. The WHO has set 2020 as a measles elimination target for the world by developing a strategy to deliver two doses of measles-containing vaccine to all children through routine services and SIAs [32, Reference Moss and Griffin33]. However, after 8 years of decline, the number of reported measles cases has increased in recent years with large outbreaks occurring not only in the developing countries but also in Europe [Reference Cottrell and Roberts17] and even in Canada where the eradication of measles was believed to have been achieved [Reference De34]. These measles outbreaks highlight the current challenges of sustaining measles elimination. The mass measles vaccination campaign with SIAs may be effective in significantly reducing the incidence of measles in a region where measles epidemics are continuing, but it has limited success in terms of eliminating the disease from a region with a large migrant population [Reference Peng35, Reference Zhang36]. The highly contagious nature of the disease, waning of immunity, suboptimal level of overall vaccine coverage rate for all eligible children, ease of international travel, and some parents’ reluctance to get their children immunized with vaccine in some developed countries may all contribute to the recent resurgence of measles. Measles elimination may be particularly difficult for densely populated countries such as China and India, since measles incidence and epidemics appear to correlate with population density [Reference Yoshikura37].
There are several limitations to our study. The majority of the reported measles cases in Wenzhou were based on clinical diagnosis and a proportion of those reported measles cases may have been misclassified, which may overestimate the incidence. On the other hand, our data probably suffer from substantial underdiagnosis/underreporting in children aged >1 year. The proportion of cases aged <1 year was substantially greater than that reported nationally (45% vs. ∼10–30%) during the same decade [Reference Ma9]. As the age of cases reflects the distribution of the vulnerability in the population, the sustained transmission in Wenzhou could not have happened if half the vulnerability in the population was confined to infants. The critical susceptible proportion necessary to maintain the population below the epidemic threshold has been estimated to be ∼5% for the whole population [Reference Gay38]. As infants represent <2% of the population and many are protected by maternal antibodies, much of the transmission in older children has probably been missed by our surveillance.
In summary, measles remains a significant problem in Wenzhou. A large proportion of measles cases are infants aged <1 year and individuals aged >14 years. The infant measles cases requiring hospitalization increased from birth to age 8 months and declined thereafter. Pneumonia remains the leading cause of measles-related hospitalization and mortality. The existence of a sufficient pool of measles-susceptible children who have missed scheduled measles immunization and the decreased level of passively transferred measles antibodies in infants from vaccinated mothers contribute to the sustained transmission observed in Wenzhou. New strategies and innovations for measles control are needed in order to meet the target of complete elimination of measles in China, which has the largest population in the world.
ACKNOWLEDGEMENTS
We thank Dr Jiang Xian-Gao for help with data collection and Dr Robert Green of the Mount Sinai School of Medicine for comments and critical review of the manuscript. This study was supported, in part, by the Pediatric Academic Development Fund of Wenzhou Medical College and the special fund for the development of key clinical subspecialities from the Ministry of Health of the People's Republic of China.
DECLARATION OF INTEREST
None.









