Nowadays, we witness an increasing growth of obesity, and 39 % of the world’s population was identified as obese and overweight till 2015. Food addiction or an addictive-like eating behaviour which is defined as the compulsive consumption of palatable (e.g. high-fat and high-sugar) foods despite their adverse consequences has recently been considered as one of the probable factors relevant to obesity(Reference Chooi, Ding and Magkos1–Reference Masheb, Ruser and Min3). The Yale Food Addiction Scale (YFAS) was developed in 2009 by Ashley Gearhardt based on Diagnostic and Statistical Manual of Mental Disorders(Reference Gearhardt, Corbin and Brownell4) as one of the main tools developed for assessing this concept which seems to consider different aspects and provides a comprehensive view of it.
The concept of food addiction is controversial(Reference Fletcher and Kenny5). On the one hand, a body of evidence challenges the concept of food addiction and proposes ‘eating addiction’ instead as a more appropriate term(Reference Hebebrand, Albayrak and Adan6). They have argued that some of the defining characteristics of drug addiction are not observed in eating behaviours(Reference Fletcher and Kenny5). On the other hand, we are faced with a number of studies advocating the term ‘food addiction’ based on some remarkable similarities between food and drug addiction. Palatable and high-energy-dense foods (including high-fat, high-sugar foods and the most recently the combination if these macronutrients), for example, could have addictive effects such as a loss of control in consuming large amounts food through hijacking the reward system(Reference Gearhardt, Boswell and White7–Reference DiFeliceantonio, Coppin and Rigoux10). Some studies have also suggested the overlapped areas of the brain as being responsible for these two types of cravings as well as the similarity in dopamine-releasing pathways activated by both drug and food consumption(Reference Pelchat11,Reference Iozzo, Guiducci and Guzzardi12) . The similarity between diagnostic criteria of substance diagnosis and essential criteria to diagnose binge eating disorder has also been reported by some studies (i.e. an inability to successfully stop or cut down on consumption despite an expressed desire to do so and a loss of control over consumption). This latter view was the main opinion that led to the development of the YFAS(Reference Gearhardt, Corbin and Brownell4).
To date, the prevalence of food addiction has been evaluated by many studies in different countries such as Germany, France and Egypt(Reference Hauck, Weiss and Schulte13–Reference Ahmed and Sayed15). The total prevalence of food addiction based on YFAS has been estimated at 19·9 % and is more prevalent in persons aged 35 years or above, compared with younger adults (22·2 % v. 17 %). The prevalence of food addiction in people with the clinical diagnosis of eating disorder is higher than many other people (57·6 % v. 16·2 %), and women suffer twice as much from this problem than men (12·2 % v. 6·4 %)(Reference Pursey, Stanwell and Gearhardt16).
Persons meeting the criteria for food addiction tend to have hedonic, non-homoeostatic feeding which is most probably related to the high prevalence of obesity worldwide(Reference Leigh and Morris17). Compared with their normal-weight counterparts, obese individuals have a more than two-fold occurrence of food addiction (24·9 % v. 11·1 %). In Iran, as in other countries, obesity is growing at an alarming rate, with a prevalence of 22·3 % in people aged 15–64 years(Reference Esteghamati, Meysamie and Khalilzadeh18); the prevalence of obesity in women is significantly higher than that in men (29·5 % v. 14·4 %)(Reference Rashidi, Mohammadpour-Ahranjani and Vafa19–Reference Mohammadi and Mirzaei21), emphasising the monitoring and controlling of obesity factors in this group as a priority. Evaluating the food addiction prevalence in obese persons raises awareness about the potential contributing factors for obesity and underscores the need for a valid and practical questionnaire for food addiction assessment.
To the best of our knowledge, there is no validated questionnaire in Iran to assess food addiction prevalence. Since both food addiction prevalence and obesity are higher in women than in men, it is reasonable to consider obese women as a high priority. Thus, the present study was conducted to assess the face and construct validity of the Iranian version of the YFAS as well as evaluating convergent validity and test–retest reliability in both the Iranian and original versions of YFAS, along with determining the prevalence of food addiction in Iranian obese women living in Tehran.
Methods
Study design and participants
A total of 450 obese women aged 18–60 years were selected from a weight management clinic in Tehran and assessed in 2016. The BMI was used to categorise women with obesity into different obesity classes (defined by the WHO with the measurement unit (kg/m2)(22). The exclusion criteria were: (1) BMI of < 30 kg/m2, (2) following a weight loss programme over the last 6 months, (3) a history of drug abuse or taking psychiatric medications, hormonal contraceptives, corticosteroids or the use of effective supplements for weight loss such as green tea, pepper, pomegranate, green coffee, dill and celery in the last 3 months, (4) having diabetes, kidney disease or any other disease requiring a particular diet (cancer, CVD, AIDS, multiple sclerosis, Parkinson’s disease, severe injuries or paralysis and psychiatric illnesses) and (5) being pregnant, breast-feeding or menopausal. The inclusion criteria were: (1) provided a signed consent form for participation, (2) aged 18–60 years and (3) BMI ≥ 30 kg/m2 without secondary obesity (obesity because of a medical condition). After obtaining written informed consent, the participants were asked to complete a personal information form (including age and education level), the Persian-translated YFAS and the Iranian version of the Binge Eating Scale (BES)(Reference Dezhkam, Moloodi and Mootabi23).
Translation process
First, we obtained permission from Ashley Gearhardt for the translation and validation of the original YFAS into an Iranian version. For forward translation, three persons (one clinical psychologist and two nutritionists) independently translated the scale into Persian, and after reaching consensus, a finalised version was obtained. Then, two translators, a nutritionist and a physician who had lived in English-speaking countries, conducted a blind-backward translation of the initially translated version of the YFAS. Finally, the English version was revised according to the main author’s suggestions. Since there are some differences in food habits between Western countries and Iran, and some of the Western foods are rarely consumed by Iranian people, a committee of two expert nutritionists applied some changes to fit the scale for the Iranian population; both backward and onward translations can be found in appendix. Finally, the initial version of the scale was pre-tested with a small sample (n 15) of Iranian participants with different educational levels to evaluate the instructions, response format and clarity of the items of the scale.
Measures
The Yale Food Addiction Scale
Gearhardt et al. applied the Diagnostic and Statistical Manual of Mental Disorders criteria for substance dependence to eating behaviours and designed the original YFAS in 2009(Reference Gearhardt, Corbin and Brownell4). The YFAS is a self-reporting questionnaire, containing twenty-five questions with two types of answers (seventeen items: five-point Likert-type format; eight items: dichotomous), and assesses the symptoms of food addiction for palatable foods (high-fat, high-sugar and high-salt food) in the past year. Among twenty-two questions of the scale, seven criteria are assessed according to the Diagnostic and Statistical Manual of Mental Disorders. There are two methods of scoring for YFAS: the symptom count and the diagnostic version. Specific cut-offs are defined for each of the seven diagnostic criteria by Gearhardt et al. In the YFAS symptom count, score 1 is considered for meeting each criterion in the past 12 months and total scores ranged from 0 to 7. In the diagnostic version, food addiction is diagnosed when three or more symptoms have been present during the past 1 year and at least one of the clinical symptom questions has been endorsed. The original validation of the scale has shown adequate internal consistency (Cronbach α = 0·86) and good construct validity with measures of similar satisfaction and measures of related but dissimilar constructs(Reference Gearhardt, Corbin and Brownell4).
The Binge Eating Scale
The BES is a sixteen-item scale designed to assess binge eating severity by using behavioural and cognitive/emotional symptoms(Reference Gormally, Black and Daston24). Each question has three or four options, with a scoring range of 0 to 3, and a higher score reflects more severe binge eating. The Iranian version of the scale used in this study was validated on an obese population and showed an acceptable internal consistency (Cronbach α = 0·85)(Reference Dezhkam, Moloodi and Mootabi23).
Assessment of anthropometric measures
Weight was measured with digital scales, while the subjects were minimally clothed and were not wearing shoes, and was recorded to the nearest 500 g. Height was determined using a tape measure, while the subjects were standing and were not wearing shoes, and with shoulders in a normal position. BMI was calculated as weight in kg divided by height in m2(Reference Cole, Freeman and Preece25). To reduce the error, all measurements were taken by the same technician.
Statistical analysis
The construct and convergent validity and the test–retest reliability of the Iranian version of the Food Addiction Scale were assessed. Descriptive data are expressed as mean ± sd. The R software and the packages of ‘psych’, ‘polycor’ and ‘sem’ were used for exploratory and confirmatory factor analyses (EFA and CFA), respectively. The SPSS 22 statistical software was used for descriptive statistics, test–retest reliability and the analysis of convergent validity(Reference Field26).
The participants were randomly divided into two groups of 220 and 230 to conduct EFA and CFA, respectively; EFA for dichotomous data was performed by varimax rotation and polychoric correlation coefficients. Given that all the items were dichotomous, Kuder–Richardson-20 coefficients were calculated for factors of the original items and the diagnostic criteria to assess their internal consistency. CFA was conducted with the second randomised sample to determine how well the single-factor structure model fit. A mean- and variance-adjusted weighted least square estimator with a polychoric correlation matrix was used in CFA. Model fit was assessed using the following indices: (1) the root-mean-square error of approximation (RMSEA); (2) the comparative fit index (CFI); (3) standardised root-mean-square residual (SRMR); (4) Tucker Lewis index (TLI) and (5) χ 2 value.
A test–retest examination using intraclass correlation coefficients (ICC) was performed to evaluate reproducibility, by comparing the symptom count and diagnostic versions of both original and Iranian YFAS between the samples of participants (n 41) who had completed the Iranian YFAS twice (a paired sample), with an interval of 15–30 d between the two administrations of the scale. As Item 24 was removed from the original scale in the preliminary validation study due to a low factor loading, the final twenty-one-item YFAS was used in the statistical analysis(Reference Gearhardt, Corbin and Brownell4). The individuals who met the criteria for food addiction in the two studies were also compared in the paired test–retest samples. Analyses were then conducted to establish the convergent validity of the Iranian version of YFAS among the entire sample. Convergent validity was determined by the correlation between both original and Iranian versions of YFAS and the Iranian version of the BES. The Spearman correlation coefficient was used for the symptom count scoring, and the bi-serial correlation coefficient was adopted for the diagnostic scoring. Finally, the characteristics of food addiction for the entire sample were described when the psychometric properties of the Iranian version of YFAS were good or acceptable.
Results
Item analysis, factor structure and internal consistency
The item-total correlation for the original twenty-two dichotomous items indicated that Item 22 did not significantly correlate with the other items (Table 1). This item was excluded in further EFA. In the EFA for the assumed single-factor structure of twenty-one items, all of the factor loadings were >0·50, except for those of Items 21, 24 and 25 (0·43, 0·26 and 0·41, respectively), and the explained variance was 0·51. A parallel factor analysis was performed for the seven diagnostic criteria (all the items were included to construct the seven criteria), and again a single-factor structure was identified. All the diagnostic criteria except for the ‘cut down’ (0·29) had factor loadings >0·5. The explained variance for the single-factor structure of the seven criteria was 0·46. The internal consistency, measured by the Kuder–Richardson-20 coefficient, exceeded the minimum reliability standard of 0·87 for the total twenty-two items. The KR-20 coefficient was above average and acceptable for the seven diagnostic criteria (KR20 = 0·70).
Table 1 Mean (sd) scores of the Iranian-corrected YFAS items and their correlations with the total score*
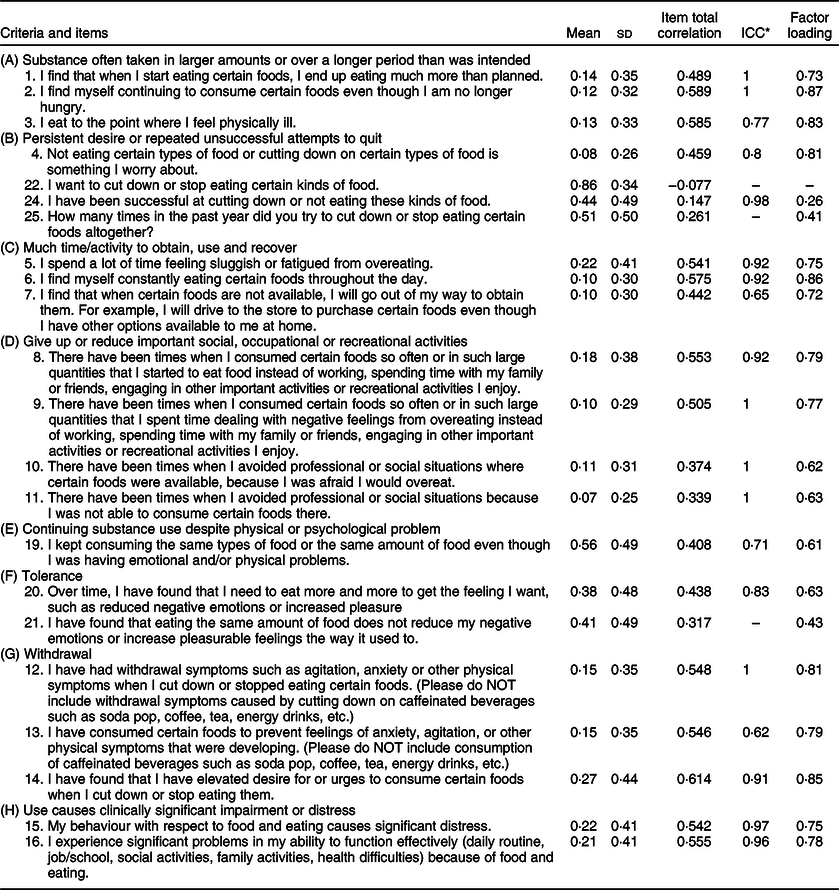
ICC, Intraclass correlation coefficient.
* Explained proportion variance = 51 %.
Confirmatory factor analysis
The fit statistics of the single-factor model for the original items and the diagnostic criteria are reported in Table 2. The single-factor model of the original twenty-two items did not have an acceptable fit (χ 2 (209) = 493·10; P < 0·01; RMSEA = 0·08; 90 % CI: 0·070, 0·088; CFI = 0·73; SRMR = 0·076; TLI = 0·75). Corresponding to the original model, Item 22 had a non-significant loading value on the common factor (R 2 = 0·001, P = 0·80). Despite Item 24 having a low factor loading in the EFA analysis, its factor loading was significant in the CFA (R 2 = 0·07, P < 0·01). Item 22 was excluded from the CFA of the single-factor model. However, the fit statistics did not improve when we deleted this item (χ 2 (189) = 453·89; P < 0·01; RMSEA = 0·08; 5 % CI 0·070, 0·089; CFI = 0·74; SRMR = 0·075; TLI = 0·71). Although the R 2 of Items 21 (R 2 = 0·015) and 25 (R 2 = 0·017) was significant, they were <0·020. Thus, we excluded Items 21 and 25 in the following analysis, and the single-factor model had a better fit to the data (χ 2 (152) = 363·66, P < 0·01, RMSEA = 0·08; 90 % CI 0·069, 0·090; CFI = 0·78; SRMR = 0·07; TLI = 0·75).
Table 2 Fit statistics for the single-factor model of the original items and diagnostic criteria
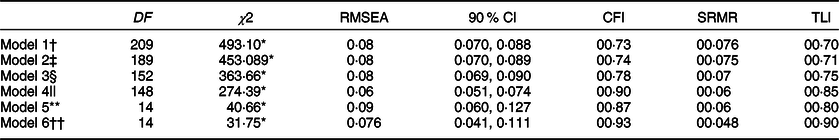
Note: Estimator: mean- and variance-adjusted weighted least square (WLSMV).
* Significant for P < 0·001.
† Model 1: Single-factor model of the original twenty-two items.
‡ Model 2: Single-factor model after excluding Item 22, for the residual twenty-one items.
§ Model 3: Single-factor model after excluding Items 21, 22 and 25, for the residual nineteen items.
|| Model 4: Modified model 3.
** Model 5: Single-factor model of the original seven diagnostic criteria.
†† Model 6: Single-factor model of the corrected diagnostic criteria.
Based on the decrease in the χ 2 value and the improvement seen in fit indices, beneficial modifications were conducted on model 3. Following the covariance structures, all of the remaining items were significant (P < 0·01). The modifications were added in the CFA model 3. r (Item 1, Item 2) = 0·31, r (Item 10, Item 11) = 0·41, r (Item 12, Item 13) = 0·27, r (Item 19, Item 20) = 0·27. (χ 2 (14) = 274·39, P < 0·01, RMSEA = 0·06; 90 % CI 0·051, 0·074; CFI = 0·90; SRMR = 0·06; TLI = 0·85. For the seven diagnostic criteria, the single-factor model had a weak fit to the data (χ 2 (14) = 40·66, P < 0·01, RMSEA = 0·09; 90 % CI 0·060, 0·127; CFI = 0·87; SRMR = 0·06; TLI = 0·80). After excluding Item 21 from the computation of ‘tolerance’ criteria, and Items 22 and 25 from the computation of the ‘cut-down’ criteria, the corrected single-factor model for the seven criteria (based on nineteen items) displayed acceptable fit indices (χ 2 (14) = 31·75, P < 0·01, RMSEA = 0·076; 90 % CI 0·041, 0·111; CFI = 0·93; SRMR = 0·048; TLI = 0·90).
Test–retest reliability
The ICC for the original twenty-one items and eight diagnostic criteria equalled 0·92 and 0·86, respectively, and both correlations were significant (P < 0·001). Based on the corrected scale, twelve out of forty-one randomly selected participants (29·3 %) met the criteria for food addiction in the preliminary study, and eleven of them (26·8 %) still met the food addiction criteria in the retest study. Surprisingly, the reliability measured for the Iranian nineteen-item scale was very close to the results for the original YFAS (ICC = 0·92 and 0·87 for questionnaire score and eight diagnosis criteria, respectively (P < 0·001)), and similar to the original scale, one participant was diagnosed with food addiction in the preliminary study but not in the second study.
Convergent validity
Correlations of the symptom count and diagnostic versions of the original YFAS with the Iranian version of BES were statistically significant (P < 0·001) and were, respectively, 0·61 and 0·44. Moreover, upon assessing this correlation between the Iranian version of YFAS and the Iranian version of BES, significant correlation coefficients for both symptom (r = 0·58) and diagnostic (r = 48) versions were achieved (P < 0·001) (Table 3).
Table 3 Correlation between Yale Food Addiction Scale (YFAS) and basic characteristics of participants (n 450)
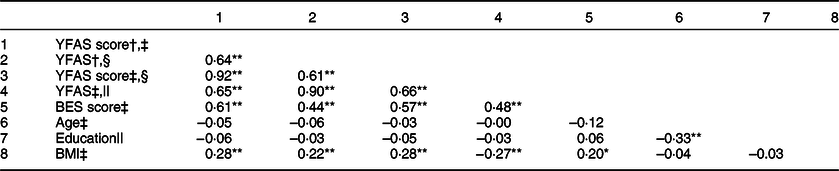
BES, Binge Eating Scale.
** P-value < 0·01.
* P-value < 0·05.
† Original twenty-one-item scale.
‡ Pearson correlation.
§ Iranian nineteen-item scale.
|| Spearman correlation.
Sample characteristics of food addiction
The participants had a mean age of 39·52 years (sd = 10·21 years; 95 % CI 18, 60 years). The average BMI was 38·10 kg/m2 (sd = 6·63 kg/m2; 95 % CI 30·06, 70·31 kg/m2); in the entire sample, 184 (40·9 %) had grade 1 obesity, 127 (28·2 %) had grade 2 obesity, and 139 (30·9 %) had morbid obesity.
Based on the original YFAS, 136 individuals (30·2 %) in the sample met the criteria for food addiction using the diagnostic method. However, using the Iranian-corrected YFAS including nineteen items, 118 persons (26·2 %) in the sample met the food addiction criteria. The KAPPA agreement value indicates a strong agreement between the two diagnostic criteria (KAPPA = 0·90, t = 19·22, P < 0·001). The correlation coefficient between the score and diagnostic versions of YFAS calculated from the original and the corrected scale was r = 0·91 (P < 0·001) and r = 0·90, respectively (P < 0·001) (Table 3).
Endorsement rates for the seven-symptom criteria were between 22·7 % for ‘substance taken in larger amounts and for a longer period than intended’ and 91·1 % for the ‘persistent desire or repeated unsuccessful attempts to quit’ according to the original YFAS. Since the main modification in the Iranian YFAS contributed to ‘cut down’, the endorsement rate of this criterion was affected more than that of the other criteria, reaching 98 %; the correlations between BMI (kg/m2) and the original YFAS symptom and diagnostic versions were poor but significant (r = 0·27 and r = 0·22, respectively). These figures were very similar for the corrected Iranian version of the scale: r = 0·25 (symptom count); r = 0·27 (diagnosis) (P < 0·001) (Table 3).
Discussion
This study assessed the face and construct validity of the Iranian version of the YFAS as well as the convergent validity and test–retest reliability of both Iranian and original versions of YFAS for obese women. To the best of our knowledge, this was the first study conducted to evaluate the psychometric properties of the Iranian version of the YFAS based on the original YFAS in obese women. Item 22 did not significantly correlate with the other items and was thus removed from further analysis, and the factor analysis identified a single-factor structure for the scale that explained 51 % of the variance after excluding Items 21, 24 and 25 which did not significantly correlate with the other items. Moreover, the results indicated the good internal consistency of the nineteen-item Iranian version of YFAS (KR-20 = 0·87). Although the factor loading of one criterion, the ‘cut down’, was low, the total internal consistency of seven criteria of the questionnaire was above average and met the minimum acceptable value (KR-20 = 0·7)(Reference Mohamad, Sulaiman and Sern27). Our analysis of the test–retest reliability also indicated that the symptom count and diagnostic versions of both original (ICC = 0·72 and 0·69, respectively) and Iranian YFAS (ICC = 0·92 and 0·87, respectively) are stable over a time interval of 14–30 d, and only one person with a food addiction diagnosis in the first study did not meet the criteria for food addiction again. The convergent validity achieved through the Pearson coefficient between the scores obtained in both original and Iranian YFAS and BES suggested a positive linear relationship. Furthermore, the correlation between BMI (kg/m2) and the score and diagnostic version of the original YFAS was 0·28 and 0·22, respectively, and these figures for the corrected Iranian YFAS equalled 0·28 and 0·27, in that order. The prevalence rate for food addiction was 30·2 % and 26·2 %, by using the original and Iranian versions of YFAS, respectively.
The weakly loaded Item 22 (I want to cut down or stop eating certain kinds of food) was excluded upon evaluating the internal consistency. Nevertheless, the high endorsement rate of this item by the participants (86 %) implied that many Iranian obese women, even without meeting the food addiction criteria, believe that they need to cut down or stop eating certain foods, a finding consistent with the original study which showed a similar result for a different item (Item 24: I have been successful at cutting down or not eating high-fat/high-sugar foods) but in the same construct ‘Persistent desire or repeated unsuccessful quitting attempts to quit’. In our study, the factor loading of Item 24 along with Items 25 (along with Item 22 referring to the persistent desire or repeated unsuccessful quitting attempts to quit) and 21 (along with Item 20 categorised as a tolerance criterion) was < 0·5. Compared with YFAS 2.0, which is a revised version of the original YFAS, two out of these three items had been changed (Item 25 of YFAS 2.0: I really wanted to cut down on or stop eating certain kinds of foods, but I just couldn’t was substituted for Item 22 of YFAS: I want to cut down or stop eating certain kinds of food) or eliminated (Item 25 of YFAS), and Item 24 had entirely been discarded(Reference Gearhardt, Corbin and Brownell28). Furthermore, the ‘cut-down’ criterion in the present study did not make a proper distinction between individuals with and without food addiction, which is in line with previous observations(Reference Brunault, Ballon and Gaillard14,Reference Meule, Heckel and Kubler29) .
According to the results of this study for CFA, the last model with the exclusion of Items 21 (I have found that eating the same amount of food does not reduce my negative emotions or increase pleasurable feelings the way it used to), 22 and 25 (How many times in the past year did you try to cut down or stop eating certain foods altogether?) obtained a better fit to the data in comparison with the previous models of our study (χ 2 (148) = 274·39, P < 0·01, RMSEA = 0·06; 90 % CI 0·051, 0·074; CFI = 0·9)(Reference Revelle30). Despite Item 24 having a low factor loading in the EFA analysis, its factor loading was significant in CFA and it was, therefore, retained in the model. This result was in accordance with the Chinese validation study of the YFAS, which conducted CFA along with EFA similar to our study and reported that Item 24 did not significantly correlate with the other items, while the exclusion of this item did not improve the fit statistics. Moreover, in the Chinese version of YFAS, the R 2 of Items 22 and 25 was < 0·02, and their deletion-led factorial model had a better fit to the data, results which support ours(Reference Chen, Tang and Guo31). In an Italian study, the model with sixteen items had a better fit (without Items 10,11, 22, 24 and 25) to the data, supporting the findings of our study, although it conducted only CFA to evaluate the construct validity of the scale (without EFA)(Reference Ceccarini, Manzoni and Castelnuovo32).
In the present study, the results of the test–retest reliability for both original and Iranian versions of YFAS were in accordance with those of the Chinese study for the twenty-one-item YFAS and eight diagnostic criteria(Reference Chen, Tang and Guo33). Among the previous studies on YFAS validation, the Chinese (r = 0·53–0·36 for symptom count and diagnostic versions, respectively), French (r = 0·58 between the scores of the two scales) and Spanish (r = 0·58 between the scores of the two scales) studies assessed the convergent validity of the scale and are all in agreement with our findings for symptom count and diagnostic versions of both original (r = 0·61–0·44, respectively) and Iranian (r = 0·57 and 0·48, respectively) YFAS, revealing a significant correlation between both symptom count and diagnostic version of YFAS with BES(Reference Brunault, Ballon and Gaillard14,Reference Chen, Tang and Guo33,Reference Valdés-Moreno, Rodríguez-Márquez and Cervantes-Navarrete34) .
In the present study, the correlation between BMI and both symptom count and diagnostic versions of the original and Iranian YFAS was poor but statistically significant, which is in line with several previous studies. For example, although the Chinese study (on underweight, normal and overweight populations; mean BMI: 19·87 kg/m2) and the Spanish study (on normal-weight, overweight and obese populations) were conducted on different populations compared with ours in terms of obesity categories, both of them reported a significant but poor correlation between BMI and YFAS score (r = 0·13–0·28, respectively) using the same method as ours. These weak correlations between BMI and YFAS scores suggest that the food addiction behaviour might manifest itself even in normal-weight individuals; however, it is required to conduct a study on different obesity classes in order to prove this matter in the Iranian population. Additionally, some other articles such as Arab (using YFAS 2.0) and German (using YFAS 2.0) studies by a different method found that participants who met the criteria for YFAS 2.0 diagnosis had a higher BMI than those who did not meet these criteria (using the Mann–Whitney U test)(Reference Hauck, Weiss and Schulte13,Reference Chen, Tang and Guo31,Reference Valdés-Moreno, Rodríguez-Márquez and Cervantes-Navarrete34,Reference Fawzi and Fawzi35) . By contrast, an Egyptian study conducted on adolescences did not observe a different food addiction diagnosis among different categories of BMI, which is probably related to the participants’ age group. This study did not give any hint about the method of YFAS validation. However, it demonstrated significant differences between various classes of BMI and all of the food addiction symptoms, except for ‘tolerance’(Reference Ahmed and Sayed15). Additionally, in the present study conducted on obese women (mean BMI: 38·10 kg/m2), we found that the prevalence rate for food addiction was more than the rates reported by studies on normal-weight population such as the French study (8·7 %; mean BMI: 22·5 kg/m2)(Reference Brunault, Ballon and Gaillard14) and less than that of the Turkish study (57·8 %; mean BMI: 47 kg/m2)(Reference Sevinçer, Konuk and Bozkurt36) which was conducted on individuals with morbid obesity.
This was the first study evaluating the psychometric properties of the Iranian version of YFAS in a vulnerable group; still, it has certain limitations. First, since both food addiction prevalence and obesity are more common among women, and due to resource limitations, we did not include men and normal-weight participants in our study and considered obese women as the first priority, which may be a limitation(Reference Mitchell and Shaw37). Using YFAS instead of YFAS 2.0 could also be considered as a limitation; however, YFAS 2.0 had not been published at the beginning of our study. Besides, we did not use another questionnaire developed for food addiction measurement called the Addiction-Like Eating Behavior Scale owing to the same reason(Reference Ruddock, Christiansen and Halford38). Moreover, we only employed the Iranian version of BES for assessing convergent validity on account of the lack of other potential validated scales in Iran such as the Eating Attitude Test and Emotional Eating Scale(Reference Gearhardt, Corbin and Brownell4). Weighing with minimal clothing is additionally bound to be another limitation of this study; hence, further research needs to be conducted to determine the validity of the scale for both men and women with different body weights using YFAS 2.0 for producing a scale usable for a general adult population.
Understanding the possible important causes of poor weight loss management can lead to finding a better solution for overcoming this epidemic problem. A validated food addiction questionnaire can be a very useful tool for assessing food addiction in obese individuals. These results demonstrate that both original and Iranian versions of the YFAS to be valid and useful instruments for assessing food addiction in obese women.
Acknowledgements
Acknowledgements: We would like to thank Soudeh Razeghi, Setaiesh Salavatian, Azadeh Nemati and Mahsan Nourzad for their help in the translation process of the scale. We would also like to acknowledge Ms. Niloofar Shiva for the critical editing of the English grammar of the manuscript. Financial support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Conflict of interest: The authors declare no conflicts of interest. Authorship: This article was developed based on a master’s thesis with the supervision of A.S. and P.A. S.A.P.M. had full access to all of the data in the study and took responsibility for the integrity of the data. Preparation of the primary manuscript of the article was performed by A.P. and P.A. Statistical analysis was conducted by H.E.Z. All the authors cooperated in the preparation of the final manuscript, which was approved by all of them. Ethics of human subject participation: Current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Ethics Committee of the National Nutrition and Food Technology Research Institute of Iran in 2/27/2016 (Code of ethics:IR.SBMU.NNFTRI.REC.1394.34). Written informed consent was obtained from all subjects/patients.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020003560






