Intensive lifestyle intervention through ongoing personal support prevents/significantly delays progression from impaired glucose tolerance (IGT) to type 2 diabetes(Reference Tuomilehto, Lindstrom and Eriksson1–Reference Knowler, Barrett-Connor and Fowler4), reduces cardiovascular risk and improves other components of the metabolic syndrome(Reference Tuomilehto, Lindstrom and Eriksson1, Reference Ratner, Goldberg and Haffner5). Such lifestyle change can be sustained and continue to reduce diabetes incidence after individual counselling has stopped(Reference Lindstrom, Ilanne-Parikka and Peltonen6). However, a strategy to identify and treat only those with IGT will not prevent growth in numbers with pre-diabetes or obesity, and implementation can be costly(Reference Herman, Brandle and Zhang7).
Lesser degrees of weight control (reductions in weight gain), potentially of use for sustaining diabetes prevention, are possible through community-based programmes(Reference Simmons, Voyle, Swinburn and O’Dea8–Reference Simmons, Fleming, Voyle, Fou, Feo and Gatland11), although these are often fraught with difficulties(Reference Simmons, Voyle, Swinburn and O’Dea8, Reference Daniel, Green and Marion9, Reference Voyle and Simmons12, Reference Simmons, Voyle, Fou, Feo and Leakehe13). Interruption of the supply of energy-dense foods in isolated communities and promotion of traditional lifestyles can also have an effect on diabetes risk(Reference Rowley, Daniel, Skinner, Skinner, White and O’Dea10, Reference O’Dea14), although these are unlikely to be practical in most populations and particularly in urban areas.
We hypothesised that the degree of ‘personal trainer’ support required for those with IGT/impaired fasting glucose (IFG)(Reference Tuomilehto, Lindstrom and Eriksson1, Reference Knowler, Barrett-Connor and Fowler4) to adopt and maintain intensive lifestyle change can be reduced through facilitating comparable lifestyle change among others in the family and community. Such an approach could also: (i) reduce the proportion progressing from normal to abnormal glucose tolerance overall (not just those with IGT/IFG); (ii) remove the need for screening (beyond that required clinically); (iii) benefit those without significant risk factors currently (e.g. children); (iv) reduce the prevalence of other metabolic syndrome components; and (v) potentially be more affordable than the current ‘high-risk’ approaches.
We now describe the study design, intervention framework and feasibility/pilot study of the ‘personal trainer’ approach for Te Wai o Rona: Diabetes Prevention Strategy, a randomised cluster-controlled participatory research trial of intensive lifestyle change, established to test our hypothesis among New Zealand Maori, a population at high risk of type 2 diabetes(Reference Joshy and Simmons15). The intervention was built upon our previous work in Polynesian communities(Reference Simmons, Fleming, Voyle, Fou, Feo and Gatland11, Reference Voyle and Simmons12). With such prior experience and as the intervention was expected to evolve through the trial (being action research) and become increasingly tailored to the participating communities, we undertook the pilot as a ‘Vanguard Study’, i.e. at the beginning of the trial. Its purpose was to test the tools used and assess the impact of the intervention within the first study participants.
Subjects and methods
Goals and power
Te Wai o Rona: Diabetes Prevention Strategy was registered in 2005 as a 4-year randomised controlled trial with the Australasian Controlled Trials Registry (ACTRN012605000622606) with the primary research goal of demonstrating a 35 % reduction in incident diabetes among Maori and other adult household members with varying levels of glucose tolerance. This target was agreed upon as it was felt that the intervention was likely to be less effective than either the Diabetes Prevention Program or the Finnish Diabetes Prevention Study (FDPS)(Reference Tuomilehto, Lindstrom and Eriksson1, Reference Knowler, Barrett-Connor and Fowler4), but more effective than expected with minimising weight gain over the study period(Reference Burke, Williams, Narayan, Leibson, Haffner and Stern16). Consistent with the hypothesis, cost-effectiveness was not expected to be calculable until the community support/action activities were fully developed (using action research principles(Reference Israel, Schulz, Parker, Becker, Allen and Guzman17)) after 3–4 years, with a cost goal of NZ$200 per head per annum.
Diabetes, IFG and IGT were diagnosed using 1998 WHO criteria(Reference Alberti and Zimmet18). Participants with a single test indicative of diabetes were excluded from the trial irrespective of the results of any follow-up tests. The trial intervention was undertaken through local District Health Boards (DHB) to allow a seamless roll-out of the intervention if shown to be affordable and effective.
To determine sample size, progression rates to diabetes were derived from those found in Mauritius for men and women with IGT (12·0 % and 8·1 % per annum, respectively) and IFG (6·1 % and 7·5 % per annum)(Reference Soderberg, Zimmet and Tuomilehto19). The initial prevalence rates of IGT/IFG were based upon a prior survey among Maori(Reference Simmons, Thompson and Volklander20). Dropout was assumed to be 10 % per annum, intra-cluster correlation to be 0·02, α as 0·05 with a power of 80 %: 4976 participants were required to show a 35 % reduction in incident diabetes from IGT/IFG over 4 years. The study had the power to detect a difference of 0·2 % in glycosylated Hb (HbA1c), but insufficient power to compare progression rates from normal to IGT/IFG.
The population, inclusion and exclusion criteria
Recruitment population was defined by the boundaries of the Waikato DHB and the tribal area of Ngati TuWharetoa in the neighbouring Lakes DHB. This area occupies 28 190 km2, with an estimated total population of 368 811 including 81 991 Maori in 2004(21). District Health Boards are responsible for funding health services in geographically defined areas (twenty-one across New Zealand) and include Maori with both Board and Executive responsibilities.
As a family-based intervention developed around traditional and contemporary Maori culture, all members of any family including at least one Maori within the same household were eligible for entry into the study. The age cut-off for entry was taken as ≥28 years on 30 September 2005. All residents with past gestational diabetes mellitus, and those aged 23 years and over with both parents with known diabetes, were also considered eligible. Those unfit to sign a consent form, with terminal disease or not permanently residing in the study area at the time of the baseline data collection were excluded. Ethical approval was provided by both the Waikato and Bay of Plenty Ethics Committees (which include Maori representatives). All participants gave signed informed consent.
Randomisation to MCHW-supported lifestyle intervention
As a combined community, family and personal intervention within relatively close-knit communities, it was important to choose the best method for maximising collective community and family change in those individuals randomised to intensive lifestyle change, while minimising contamination of the controls. Options included through individuals, extended families (whanau), affiliation with local meeting houses (marae), households and small census areas. The latter was chosen, particularly to take account of the frequent close proximity of Maori households and the large number of Maori from outside the area, away from their tribal area and/or in the urban areas.
A stratified cluster randomisation was undertaken to maximise the chance of comparable numbers and characteristics within each limb. Cluster randomisation within each stratum was done using an electronic randomiser within SPSS (SPSS Inc., Chicago, IL, USA). Randomisation occurred until 50 % of clusters in a stratum were randomised to intensive or control.
Five rural strata, with 106 clusters, were created from the 2001 census data by the number of adult Maori. Some areas with fewer than thirty-five residents were felt to be unlikely to have enough responders and came under a nearby cluster. Urban strata were randomised within the two largest towns creating 106 clusters of 75–150 adult Maori defined by NZ statistics census areas. Randomisation created fifty-two rural and fifty-four urban intensive clusters and fifty-four rural and fifty-two urban ‘additional’ clusters (so called as participants in these latter areas received screening, their results and other information).
Recruitment
Recruitment occurred between May 2004 and March 2006 and involved written invitations from local general practitioners (GP), media releases (television, radio, posters, newspapers) announcing times/venues of screening, personal contact through different health organisations and their staff, and announcements at a number of Maori community activities. Those who attended were asked to inform other family members and friends.
Measurements
Staff were trained and standardised in questionnaire and measurement completion. Sessions were held between 07.00 and 14.00 hours in a variety of community venues across the study area. Transport was provided for participants where possible. Participants were asked to attend after a 10 h overnight fast, although attending non-fasting was acceptable (although an oral glucose tolerance test (OGTT) was not then performed). After registration/consent and ascertainment of fasting status, fasting participants had a finger-prick glucose test (venous plasma equivalent) using a glucose meter (Advantage; Roche, Switzerland). Those who were non-fasting had a single venesection for glucose and HbA1c (Bio-Rad Diamat Variant (upper limit of reference range 6·4 %); Bio-Rad Laboratories, USA). Fasting participants with a finger-prick glucose ≥4·4 mmol/l were invited to undertake a 75 g 2 h OGTT. Questionnaires were completed with assistance and included demographic data, fasting status, stage of change for lifestyle(Reference Simmons and Mesui22), the revised Physical Activity Readiness Questionnaire (rPAR-Q)(Reference Cardinal, Esters and Cardinal23) and a number of health, food and lifestyle-related questions.
Participants were measured in six private booths with a set of equipment at each booth. Measurements included height without shoes using a stadiometer (to the nearest 0·5 cm) and weight in light clothing and without shoes to the nearest 0·1 kg (Wedderburn TITH316 Personal scales), using Wedderburn TI-BWB800 Personal scales (up to 200 kg) for oversize participants. Waist was measured on standing participants, at the lateral midpoint between the lower rib and the iliac crest. All measurements were taken in duplicate, and repeated if beyond a specified tolerance level.
Based upon previous research including Maori(Reference Simmons, Thompson and Engelgau24), if no OGTT had been completed and the fasting glucose was ≥5·3 mmol/l or a random glucose ≥5·3 mmol/l or the HbA1c ≥5·3 %, participants were asked to attend the local community laboratory for an OGTT. Samples for HbA1c were sent to the same laboratory for analysis.
The intervention
All participants received a copy of their results with relevant comments regarding abnormal results and were advised to visit their GP where necessary. The ‘intensive’ intervention included personal support delivered by a MCHW (built upon previous experience(Reference Tregonning, Simmons and Fleming25)) employed across eleven Maori Health Providers. In the intensive areas, social mobilisation to maximise support for lifestyle change was planned based upon previous experience(Reference Simmons, Voyle, Swinburn and O’Dea8, Reference Simmons, Fleming, Voyle, Fou, Feo and Gatland11–Reference Simmons, Voyle, Fou, Feo and Leakehe13). The MCHW was trained to deliver the intervention using principles based upon social cognitive theory(Reference Bandura26) and tailored to the stage of change for any individual lifestyle behaviour(Reference Simmons, Voyle, Fou, Feo and Leakehe13, Reference Simmons and Mesui22, Reference Prochaska27). Participants with significant risk from physical activity on rPAR-Q(Reference Cardinal, Esters and Cardinal23) in the intensive group were provided with a subsidised visit to see their GP for consideration for a ‘Green Prescription’(Reference Elley, Kerse, Arroll and Robinson28), to advise on the intensity of physical activity considered safe, and referral for a single counselling session with a Maori exercise coach.
The FDPS showed that those adopting at least four of their five ‘lifestyle goals’ did not progress to diabetes over the initial study period(Reference Tuomilehto, Lindstrom and Eriksson1). These ‘lifestyle goals’ were mapped onto lifestyle changes (themselves expressed as ‘messages’), expected to be required and potentially achievable through small changes. Lifestyle changes were based upon existing Maori dietary and physical activity behaviours(Reference Cambie and Ferguson29, 30) and through a series of working groups including local Maori elders, Maori and non-Maori health workers and researchers. During this process, a set of goals emerged emphasising a reduction in total energy consumption including from simple carbohydrate consumption, and dropping the ‘<30 % of energy intake from fat’ goal of the FDPS. Table 1 shows the messages, goals and their linkages.
Table 1 Te Wai o Rona: Diabetes Prevention Strategy – twelve messages, eleven goals and their linkages

No emphasis on alcohol was made.
MCHW training was provided in modular form covering basic anatomy and physiology, communication skills, motivational interviewing(Reference West, DiLillo, Bursac, Gore and Greene31), broader health issues and the content and background to the twelve messages of the lifestyle intervention. A desk file (including safety and engagement principles and intervention approach) and toolkit supporting the twelve messages were created from existing materials or developed de novo and distributed in a case to each MCHW. Part of this toolkit was a personal digital assistant (PDA) (QTek; Vodafone, HTC, Taiwan) with a program including a register of participants allocated to the MCHW, providing information from the screening and a detailed, structured approach to the interview. Each MCHW was allocated a set of scales (Bathroom scales 62813, 0–150 kg; Soehnle, Germany) and weight was measured when agreed; however, the focus was on achieving the lifestyle changes, not weight change. Information was recorded into the PDA interface forms with structured fields throughout each interaction. The PDA was synchronised at the end of each encounter (by phone or face to face) and information merged with the rest of the participant data, based on the unique participant ID. The first encounter (at the very least) was for familiarisation (known as whakawhanaungatanga) at which the PDA was usually not used, although purpose and perhaps some materials were provided. This was at the discretion of the MCHW. MCHW were advised to prioritise those with IGT/IFG. Caseloads were expected to vary according to rurality and recruitment, but on average were expected to be between 160 and 250. Group sessions (but not class-based education as in the Diabetes Prevention Programme (DPP)(Reference Pan, Li and Hu2)) as in our previous programmes(Reference Simmons, Fleming, Voyle, Fou, Feo and Gatland11, Reference Voyle and Simmons12) were expected to develop through the local communities, through the participatory research approach(Reference Israel, Schulz, Parker, Becker, Allen and Guzman17) and were not a significant part of the pilot study.
The Vanguard pilot/feasibility study
Overall, 5240 non-pregnant Maori family members, without known diabetes, were recruited into Te Wai Rona: Diabetes Prevention Strategy across the Waikato and Lakes DHB catchment areas. The Vanguard Study, nested within the overall study, tested the MCHW coaching and associated tools in the intensive clusters in four geographical areas (three rural and one urban) chosen by the readiness of their allocated MCHW. All participants who had entered the trial and received their results at the time of the pilot were invited to participate. Figure 1 shows the source of the sample. The Vanguard Study was completed on 3 March 2006. Those in the Vanguard Study were not different from the complete cohort by age, sex or socio-economic status. In February 2006, measurements were obtained before intervention among participants in the initial area who had been recruited too late to enter the pilot (‘controls’). The baseline data for all remaining participants (‘additional subjects’ and those who had not been seen by a MCHW) in the four geographic areas were also analysed to show how well these ‘controls’ reflected the wider cohort who did not receive the intervention or additional weight measures. Acceptability of the tools (including PDA) to MCHW and participants was assessed through discussions with the MCHW. Comparisons between the Vanguard cohort and controls were made using the χ 2 test for categorical variables and t test for continuous variables. Changes over time were compared using the paired t test and changes between groups compared by analysis of variance. All tests were two-tailed with P = 0·05 taken as significant. As this was a pilot study for a fully powered trial, incident diabetes was not systematically identified during this time period, awaiting a second round of screening at the trial midpoint.

Fig. 1 Source of sample in the Vanguard Study
Results
Table 2 shows the baseline characteristics of the Vanguard Study cohort, the fifty-two ‘controls’ and 1143 other participants from the four geographical areas. Those in the Vanguard Study included more participants with IGT/IFG than others in the area and were heavier.
Table 2 Te Wai o Rona: Diabetes Prevention Strategy – Vanguard Study cohort and controls, baseline data
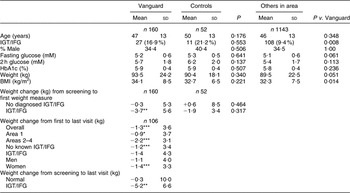
IGT, impaired glucose tolerance; IFG, impaired fasting glucose; HbA1C, glycosylated Hb.
*P < 0·05, **P < 0·01, ***P < 0·001 (paired t test within group or χ 2 test).
The first PDA-recorded visit took place 351 (sd 110) (range 95–623) days after screening in the Vanguard Study cohort and 422 (sd 223) (range 161–665) days in the ‘control’ group. The intervention occurred (as per PDA) over 189 (sd 128) (range 6–485) days during the Vanguard Study period. Between one and seventeen (mean 3 (sd 2)) contacts were recorded with each participant during this time, although this would have excluded the initial visit(s) and incidental meetings (e.g. in the supermarket). MCHW reports indicated that the messages, toolkit and delivery approach were acceptable to both MCHW and participants. The PDA were shown to be easy to use among MCHW, and allowed them to record weight reliably; a small number of areas for upgrade of the software program were identified. No changes to the other toolkit components were required. One participant was excluded due to PDA data entry error.
Those with IGT/IFG, but not other participants, lost weight by the time of the first weighing. Significant weight loss also occurred between the first and last MCHW visits, independent of area (and therefore MCHW), gender (although significantly only among women) and initial glucose tolerance (although significantly only among those without known IGT/IFG). This translated into an overall weight loss from screening to last visit of 5·2 (sd 6·6) kg (P < 0·01) among those with IGT/IFG.
Discussion
The major additional strategy in Te Wai o Rona: Diabetes Prevention Strategy beyond our past approaches(Reference Simmons, Voyle, Swinburn and O’Dea8, Reference Simmons, Fleming, Voyle, Fou, Feo and Gatland11–Reference Simmons, Voyle, Fou, Feo and Leakehe13) was the addition of the MCHW trainer, expected to be of most use in the first year and to be supplemented by group sessions, improvements in access to healthy food and physical activity options, and shifts in community attitude. The MCHW intervention was seen as the key to the downstream intervention activities. The Vanguard Study strongly suggests that our intervention was associated with weight loss, the major component in diabetes prevention(Reference Ratner, Goldberg and Haffner5). Although only a small fraction of the whole Te Wai o Rona: Diabetes Prevention Strategy cohort, this Vanguard Study is the largest intervention among Maori so far reported(Reference Murphy, McAuley and Bell32), and confirms that weight management can be successfully achieved if undertaken in the appropriate manner.
The extent of the weight loss, particularly among those with IGT/IFG, was unexpected and at the same level as in the DPP(Reference Knowler, Barrett-Connor and Fowler4), although the bulk occurred in the period between screening and the first recorded encounter with the MCHW. During this time, participants were advised of their risk in the letter, advised to see their GP if any clinical reason arose (e.g. IGT/IFG) or for prior assessment for physical activity, and these could have contributed to this weight loss. Furthermore, the recruitment, and indeed the whole study process, was actively promoted in the media and at cultural events and was a major talking point in the community, and this also could have stimulated some individuals to adopt lifestyle change. However, intensively treated participants would have had one or more unrecorded MCHW encounters and these may have had a significant effect. These visits were not recorded as it was felt that the PDA could be intrusive at such a session, where the family and community ties, study and intervention process and overall trust building were more of a focus than the messages. Having said this, many participants were keen to commence and advice would have been given. In two of the Vanguard Study areas, the MCHW established walking groups, which although ultimately intended to be run by local leaders, would have been another unrecorded intervention activity.
Interpretation of the Vanguard Study findings is complex. The reproducibility by geographical, demographic and glucose tolerance group all suggest that among these individuals, the intervention was associated with weight loss. On the other hand, this was a small non-randomised group with the potentially more interested participants involved: this may not reflect what would happen over the wider population or over a longer period of time (although on average the intervention had been in place for at least 6 months). We were particularly encouraged by the impact across different MCHW, suggesting that the intervention effect was likely to be greater than the MCHW personalities. Ultimately, over twenty MCHW have been trained. Unfortunately, the Te Wai o Rona: Diabetes Prevention Strategy could not be completed within the first 3 years and no new funding was made available for the research to continue.
At the heart of the intervention was the ‘message’ approach, designed to create small successes and thereby promote recognition of the ability to succeed in changing lifestyle(Reference Bandura26). The intervention also included identification and the development of strategies to deal with obstacles to lifestyle change, while promoting positive aspects of healthy choices(Reference Prochaska27). In the intervention development stage, preferred forms of physical activity (e.g. walking) were identified and the toolkit was built around these preferences. One area of conflict between contemporary lifestyle advice and Maori preferences was over the protein, fat and carbohydrate content of the diet. The pre-colonial diet(Reference Cambie and Ferguson29) varied according to area (e.g. those living by the sea ate more seafood, those by rivers, eel and so forth), but contemporary preferences relate more to a higher fat and protein content than recommended(33). Furthermore, there is good evidence that low carbohydrate diets are associated with significant weight loss (albeit with adverse metabolic consequences)(Reference Foster, Wyatt and Hill34). In view of this, a higher proportion of protein (with low saturated fat content) was actively promoted in the messages, although the differences with the Atkins diet were also emphasised. Further analysis is currently underway on the lifestyle choices at baseline.
In conclusion, we have recruited a large cohort of Maori and their family members into a randomised cluster-controlled trial of the impact of personal lifestyle change supported by changes in the surrounding social and physical environment. The study is powered to show a 35 % reduction in incident diabetes and improvements in diabetes risk factors. The Vanguard Study confirmed the effectiveness of the approach, allowed modification to the tools and suggested that the study goals would have been likely to be achieved.
Acknowledgements
Source of funding:Funding was provided by Health Research Council, Waikato District Health Board, Lakes District Health Board, Ministry of Health, Sport and Recreation New Zealand, Southern Trust, Waikato Local Diabetes Team and Merck Sharp and Dohme. Support in kind was provided by Roche Diagnostics, Pathlab, Medlab, University of Auckland, Auckland University of Technology, Wintec, Te Hotu Manawa Maori, Eggs Inc., Vodafone, Rivermill Bakers, Sun Fruit.
Conflict of interest:There was no conflict of interest.
Author contributions:All authors substantially contributed to the design of the experiment, collection of data, analysis of data, writing of the manuscript and provision of significant advice and consultation in its preparation. The project was led by Professor David Simmons with Elaine Rush in the Waikato and Dr Nic Crook in the Lakes District.
Acknowledgements:We thank the investigator group, Kaitiaki, Maori community health workers, Te Wai o Rona: Diabetes Prevention Strategy Project team and local health service staff for their varied contributions to the study.





