Introduction
Drug use disorders confer a substantial burden of disease globally, afflicting 71.2 million people in 2017 (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). It was the seventh largest contributor to the years lived with disability for 354 diseases and injuries globally in 2017 for men, and the 18th largest contributor for women (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). Drug use disorders can have many adverse social, psychological and physical consequences (Haritavorn, Reference Haritavorn2014; Nogueira et al., Reference Nogueira, Bosch, Valero, Gómez-Barros, Palomar, Richarte, Corrales, Nasillo, Vidal, Casas and Ramos-Quiroga2014; Compton et al., Reference Compton, Jones, Baldwin, Harding, Blanco and Wargo2019), including damage to major life roles, high suicide risk, neuropsychological deficits, decreased quality of life, high rates of risky behaviours (e.g. unsafe sex and drug injection), and increased risk of infectious diseases (e.g. human immunodeficiency virus and hepatitis) (Swendsen and Merikangas, Reference Swendsen and Merikangas2000; Compton et al., Reference Compton, Cottler, Jacobs, Ben-Abdallah and Spitznagel2003; Kessler, Reference Kessler2004; O'Brien et al., Reference O'Brien, Charney, Lewis, Cornish, Post, Woody, Zubieta, Anthony, Blaine, Bowden, Calabrese, Carroll, Kosten, Rounsaville, Childress, Oslin, Pettinati, Davis, Demartino, Drake, Fleming, Fricks, Glassman, Levin, Nunes, Johnson, Jordan, Kessler, Laden, Regier, Renner, Ries, Sklar-Blake and Weisner2004; Degenhardt and Hall, Reference Degenhardt and Hall2012; Ghimire et al., Reference Ghimire, Suguimoto, Zamani, Ono-Kihara and Kihara2013; Monnat et al., Reference Monnat, Peters, Berg and Hochstetler2019; Guo et al., Reference Guo, Luo, Wang, Xiao, Xi, Wang, Zhao, Zhang and Lu2019).
Since 1990 there has been a considerable increase in the number of people affected by drug use disorders globally, which is driven by population growth and population ageing. Although previous study reported that the prevalence of drug use disorders involving opioid, cocaine, cannabis and amphetamine increased by 47.3, 39.7, 25.6 and 22.5%, respectively, from 1990 to 2016 globally (GBD 2016 Alcohol and Drug Use Collaborators, 2018), it mainly studied the regional distribution of drug use disorders. As we all know, to understand the prevalence of a disease, the three distribution of diseases are usually studied, that is, time distribution, geographical distribution and population distribution.
So in this study, we retrieved detailed information on the incidence of drug use disorders (for opioid, cocaine, cannabis and amphetamine) from the GBD 2017 data. We further assessed the disease burden of drug use disorders by determining the temporal trends in their incidence in different times, regions and populations. This study can be helpful when designing more effective policies and methods for preventing drug use disorders that are tailored to different countries.
Methods
Data sources
Previous studies have described in detail the general methods used for the GBD data and the methods for estimating the disease burden of drug use disorders (GBD 2016 Alcohol and Drug Use Collaborators, 2018; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). In brief, the incidences were determined by performing systematic reviews of compiled data using the peer-reviewed literature such as PsycInfo, Embase, PubMed and the China National Knowledge Infrastructure database, the grey literature, and expert consultations performed by GBD Collaborators. Data on the disease burden of drug use disorders can be obtained using an online data source tool, the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool). For example, if we want to get the global age-standardised incidence rate (ASR) of opioid use disorder in 2017, we go to the website of the GHDx query tool and select ‘Global’ in the ‘Location’ drop-down box, ‘2017’ in the ‘Year’ drop-down box, ‘Cause’ in ‘Context’ drop-down box, ‘Age-standardised’ in ‘Age’ drop-down box, ‘Rate’ in ‘Metric’ drop-down box, ‘Incidence’ in ‘Measure’ drop-down box, ‘Both’ in ‘Sex’ drop-down box and ‘Opioid use disorders’ in ‘Cause’ drop-down box, and finally click ‘Search’. By repeating the above data extraction process, we can obtained the annual incident cases and the ASR or age-specific incidence rate of drug use disorders from 1990 to 2017 according to sex, age, regions and countries and territories for four drugs: opioid, cocaine, cannabis and amphetamine. For the data at country and territory level, we extracted the data from the areas which were labelled as the ‘country’ or ‘territory’ in GHDx and excluded the data from the provinces of countries. We extracted the socio-demographic index (SDI) of each country from the GBD 2017 database and categorised countries into the following SDI quintiles: low, low-middle, middle, high-middle and high. Drug use disorders were defined based on the diagnostic criteria of the text revision of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) and the tenth revision of the International Classification of Diseases (ICD-10) (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). The drug use disorders analysed in this study were opioid use disorder, cocaine use disorder, amphetamine use disorder and cannabis use disorder.
Statistical analysis
This study used the ASR and estimated annual percentage change (EAPC) to quantify and evaluate the trends in the incidence of drug use disorders. In epidemiology, it is necessary to use a standardised indicator when comparing multiple populations with different age structures, or in the same population with an age distribution that changes over time. In addition, ASR trends could reveal current patterns in a population-based study and might usefully reflect the relationship between risk factors and disease trends. Thus, analysis based on ASR can reveal the effectiveness of current policies and disease prevention strategies and be useful when developing new policies and strategies for improving health. The EAPC, which is approximately equal to the annual change over a specified time period, is calculated on a linear scale to assess trends in the ASR. From the linear regression model y = b 0 + b 1x + c, where y = ln(ASR) and x = calendar year, EAPC can be calculated as 100 × (exp(b 1) − 1), as well as its 95% confidence interval (CI). The ASR trend can be quantified as the EAPC. If EAPC estimates and their lower bound of 95% CI are positive, then ASR is considered to be in an increasing trend. On the contrary, if both EAPC estimation and the upper limit of 95% CI are negative, ASR shows a downward trend. Otherwise, ASR is considered stable. If the EAPC is statistically significant but the 95% uncertainty intervals (UIs) of the ASRs overlap, ASR is still considered to be stable.
Gaussian process regression and the Pearson's correlation coefficient were used to establish the average relationship between the ASR and SDI in 2017. Statistical analyses were performed using R software (version 3.4.3). Statistical significance was considered to be present when p ≤ 0.05.
Results
Drug use disorders
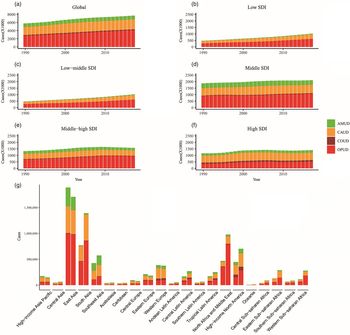
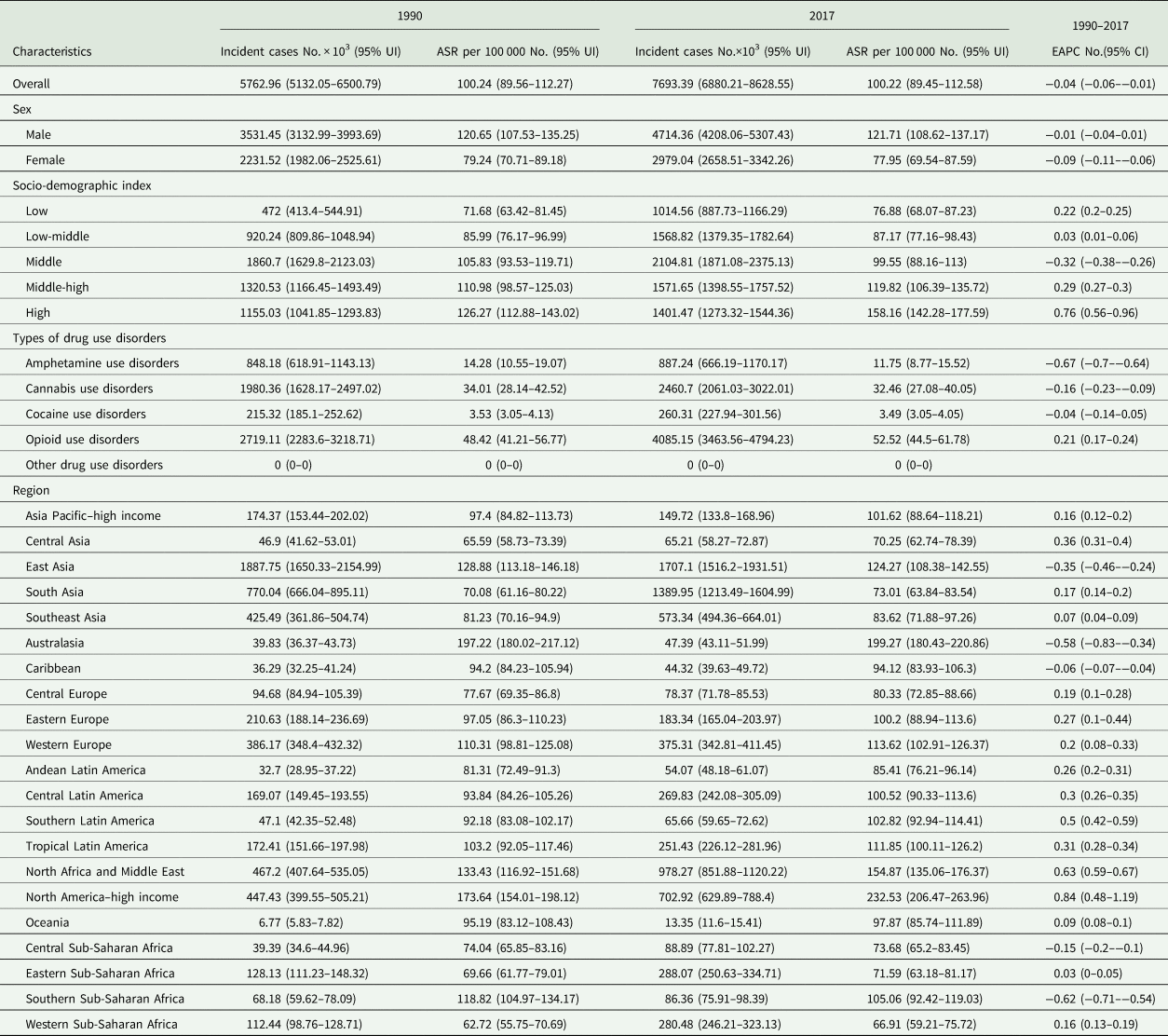
The number of cases of drug use disorder reached an estimated 7.7 million globally in 2017, which increased by 33.5% than that in 1990 (Fig. 1a, Table 1). The ASR exhibited a stable trend from 100.24 per 100 000 in 1990 to 100.22 per 100 000 in 2017 (Table 1). The ASR in men was higher than in women. The proportions of the four-drug use disorders (for opioid, cocaine, cannabis and amphetamine) in 1990 and 2017 are presented in Fig. 2. The figure shows that opioid use disorder accounted for most of the cases, with its proportion increasing from 47.18% in 1990 to 53.1% in 2017.
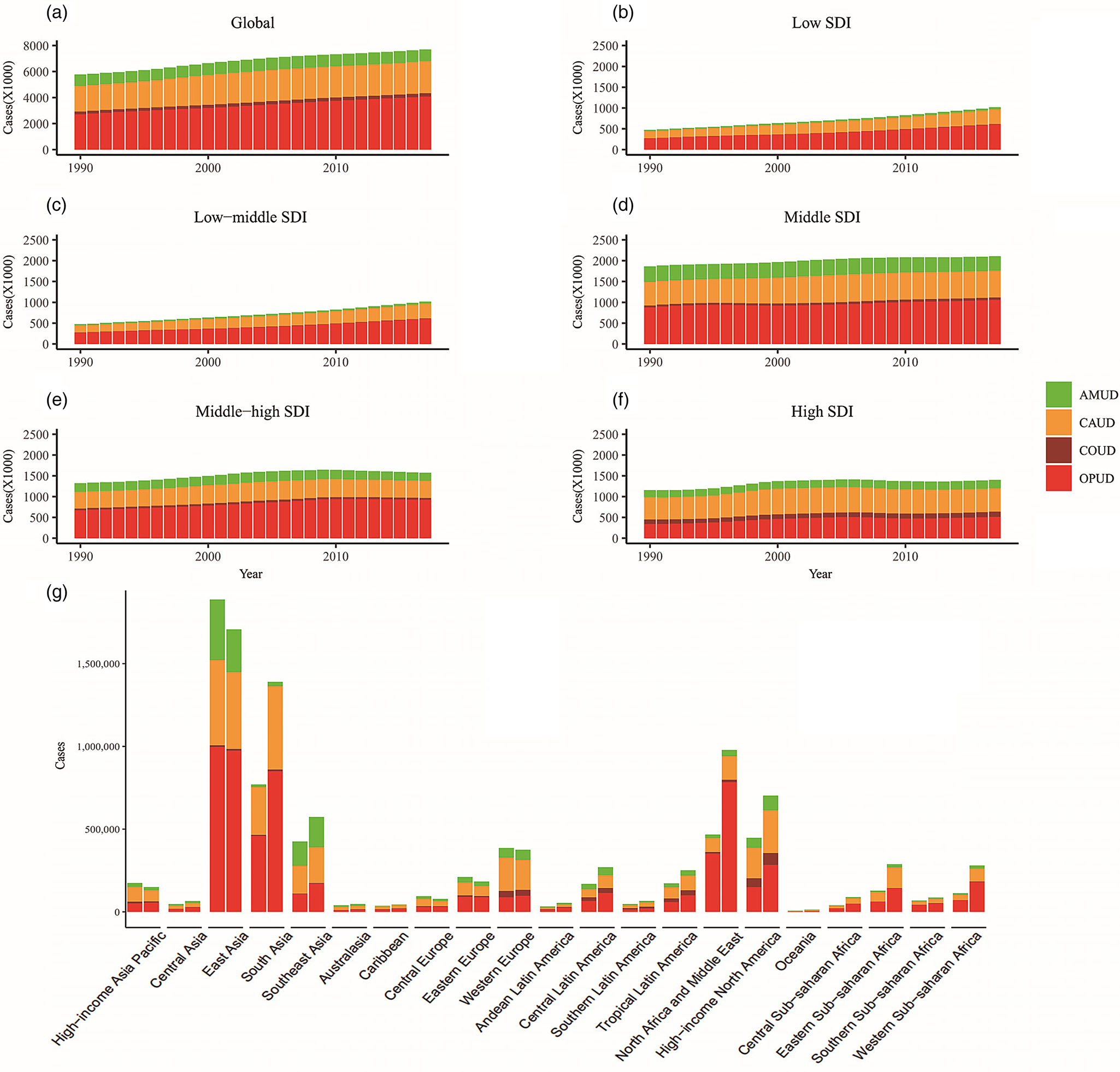
Fig. 1. The cases of different types of drug use disorders from 1990 to 2017. (a) Global, (b) low SDI regions, (c) low-middle SDI regions, (d) middle SDI regions, (e) high-middle SDI regions and (f) high SDI regions. (g) The incident cases of drug use disorders at a regional level (the left column in each group is case data in 1990 and the right column in 2017). Note: OPUD, opioid use disorder; COUD, cocaine use disorder; CAUD, cannabis use disorder; AMUD, amphetamine use disorder.
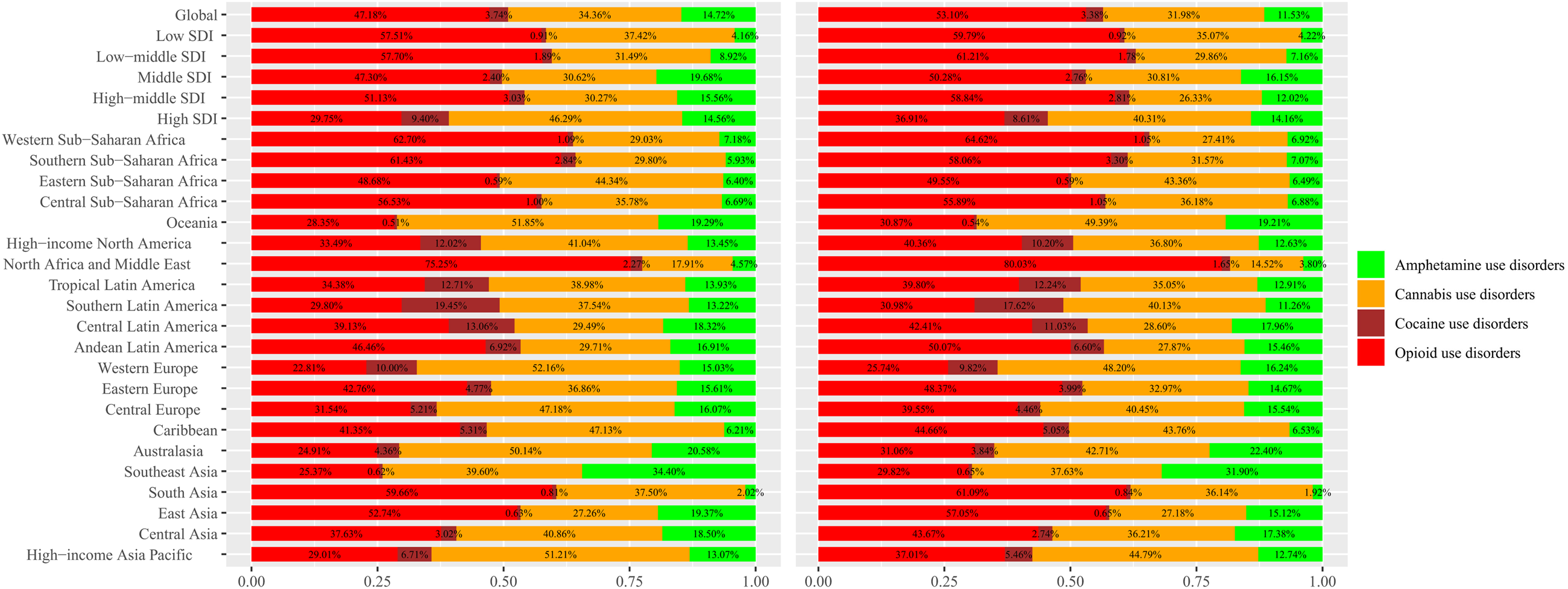
Fig. 2. Percentage of incident case of different drug use disorders by region in 1990 and 2017. The left column in each group is case data in 1990 and the right column in 2017.
Table 1. The incident cases and ASR of drug use disorders in 1990 and 2017, and the temporal trends of ASR from 1990 to 2017
ASR, age-standardised incidence rate; CI, confidence interval; EAPC, estimated annual percentage change; UI, uncertainty interval.
Regarding the SDI regions, the number of drug-use-disorder cases increased monotonically in the low-, low-middle- and middle-SDI regions (Figs. 1b–d). The ASRs were stable in five SDI regions (Table 1).
Regarding the geographical regions, the number of drug-use-disorder cases decreased in five regions: high-income Asia Pacific, East Asia, Central Europe, Eastern Europe and Western Europe (Table 1, Fig. 1g); it increased in the remaining 16 regions. As indicated in Table 1, high-income North America had the highest ASR (232.53 per 100 000) and it is the only one in 21 regions in which the ASR increased significantly with an EAPC of 0.84 (95% CI, 0.48–1.19). The ASRs in the remaining 20 regions were stable. (Table 1).
Regarding the countries and territories, the incidence of drug use disorders varies (Table S1).
Opioid use disorder
The incidence of opioid use disorder was the highest globally, representing 53.1% of drug use disorders in 2017 (Fig. 2, Table S2). The ASR of opioid use disorder displayed a stable trend from 48.42 per 100 000 in 1990 to 52.52 per 100 000 in 2017 (Table S2). Regarding the SDI regions, the ASR exhibited a increasing trend (EAPC = 1.31, 95% CI, 0.93–1.7) in high-SDI regions, while it was stable in four other SDI regions (Table S2). Regarding the geographical regions, the ASR was stable in most regions (20 out of 21) and the ASR in only high-income North America shows a significant increase (EAPC = 1.3, 95% CI, 0.65–1.96) (Table S2).
Cannabis use disorder
Cannabis accounted for 31.98% of drug use disorders in 2017, being second only to opioid (Fig. 2, Table S3). The ASR of cannabis use disorder showed a stable trend globally with 34.01 per 100 000 in 1990 to 32.46 per 100 000 in 2017 (Table S3). Regarding the SDI regions, high-SDI regions had the highest ASR (67.69 per 100 000) and all SDI regions had stable trend in ASR (Table S3). The ASR was also stable from 1990 to 2017 in all 21 geographical regions (Table S3). High-income North America had the higher ASR (88.92 per 100 000), followed by Australasia (88.74 per 100 000).
Amphetamine use disorder
Amphetamine use disorder (11.53%) represented the third-most-common drug use disorder in 2017 (Fig. 2, Table S4). There was a stable trend in ASR of amphetamine use disorder globally (Table S4). Regarding SDI and geographical regions level analysis, the trend in ASR was still stable in all regions (Table S4).
Cocaine use disorder
Cocaine use disorder accounted for the smallest proportion of the four analysed drug use disorders, at 3.74% in 1990 and 3.38% in 2017 (Fig. 2, Table S5). The ASR of cocaine use disorder showed a stable trend at global, SDI regions and geographical regions, which was similar to cannabis and amphetamine use disorder (Table S5).
Correlation between ASR and SDI
As Fig. 3 shows, a significant positive association (ρ=0.35, p < 0.001) was found between ASR and SDI in 2017 as a whole. However, when the SDI at the level of countries and territories exceeded 0.8, there appeared to be a negative association between ASR and SDI.
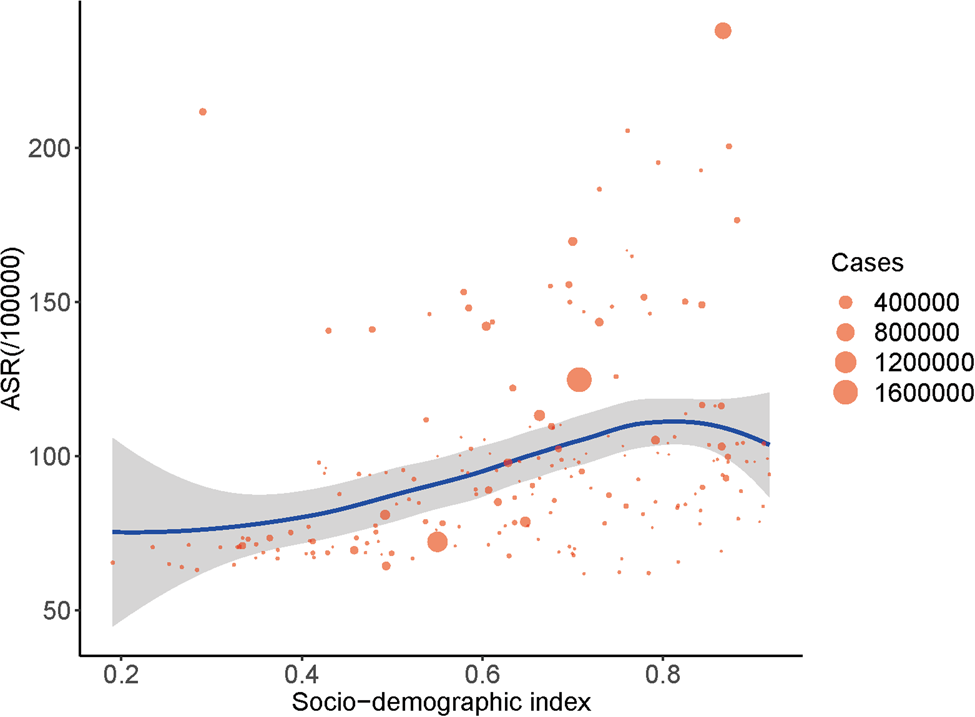
Fig. 3. The correlation between ASR and SDI in 2017. Note: ASR, age-standardised incidence rate; SDI, socio-demographic index.
Age characteristics of the incidence rate of drug use disorders
In both sexes, the incidence rate of drug use disorders was the highest among teenagers aged 15–19 years, and was dominated by cannabis, followed by opioid, amphetamine and cocaine. The incidence rate of drug use disorders decreased overall among those aged 20–70 years, with opioid constituting to the largest proportion of drug use disorders. In children aged 10–14 years, cannabis was the predominant contributor to drug use disorders (Fig. 4a).
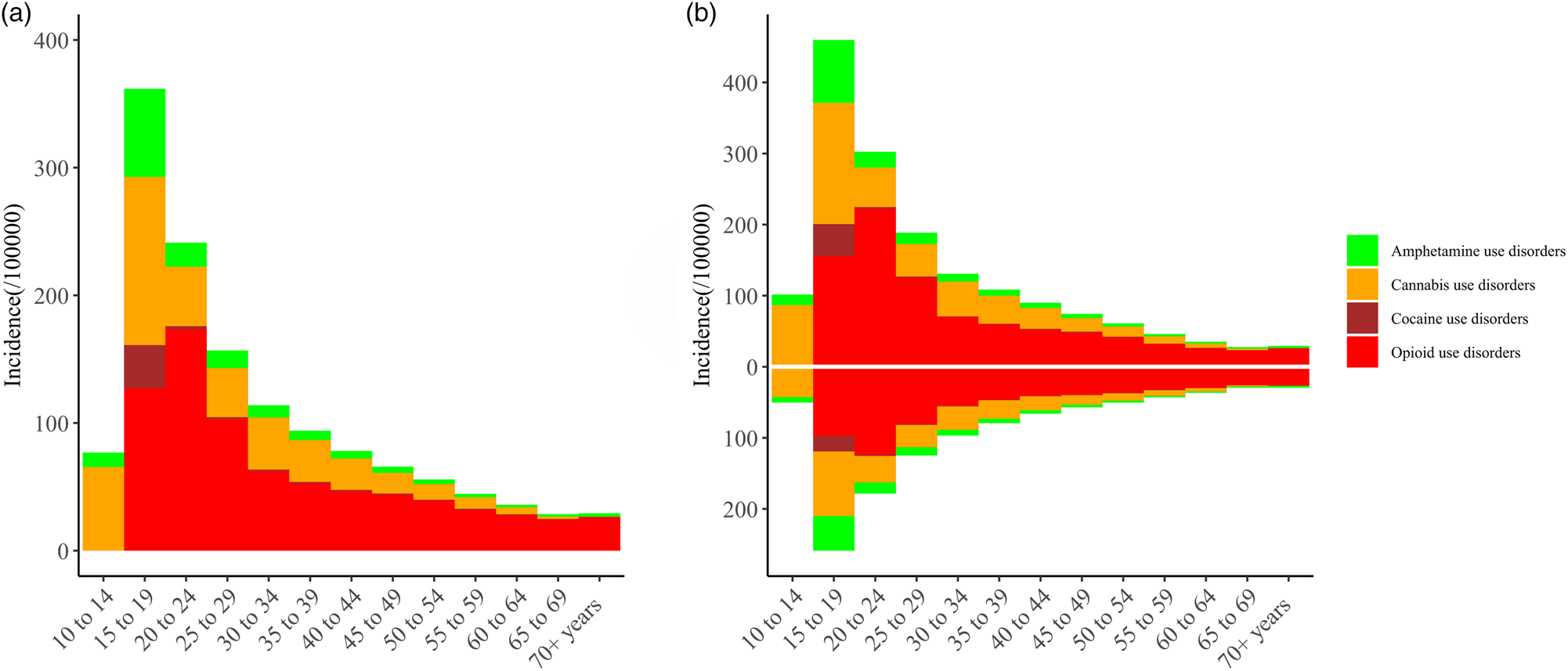
Fig. 4. Distribution of different ages in the incidence rate of drug use disorders. (a) Both sexes, (b) men and women.
The age characteristics of the incidence rate of drug use disorders were the same for men separately as for both sexes overall, while there were some minor differences for women separately (Fig. 4b). The main difference was that the incidence of drug use disorders was mainly caused by opioid rather than cannabis in girls aged 10–14 years (Fig. 4b). The incidence rate of drug use disorders was higher in men than in women in most of the age groups, but the incidence rates for the two sexes tended to become closer with increasing age.
Discussion
This study revealed the latest trends and patterns in the worldwide incidence of drug use disorders, the relationship between the ASR and SDI, and the age distribution of drug use disorders based on the GBD 2017 data. It showed that the number of drug-use-disorder cases had increased substantially since 1990, which might be due to population growth and ageing. Nevertheless, the trend in the ASR of drug use disorders showed stable, which was different from the previous study (GBD 2016 Alcohol and Drug Use Collaborators, 2018). The previous study (GBD 2016 Alcohol and Drug Use Collaborators, 2018) reported that age-standardised prevalence decreased for drug use disorders at global. This difference is mainly due to the fact that previous studies (GBD 2016 Alcohol and Drug Use Collaborators, 2018) ignored the 95% UI of age-standardised rate. Our study considered that when the 95% UI overlaps, the age-standardised rate cannot be considered as significantly changed, which makes our results more conservative and credible. The incidence of drug use disorders varied between regions, countries and types of drug use disorders in our study. Geographically, high-income North America deserves special attention because it was the only geographical region where the trend of the ASR was increasing. Regardless of gender, the incidence of drug use disorders is the highest among teenagers aged 15–19 years and it declined with age.
Special attention needs to be paid to the finding that opioid constituted more than 50% of the incidence of drug use disorders, and was the only one of the four analysed drugs that showed an increasing trend for ASR in few regions (high-SDI regions and high-income North America). Opioid use disorder tended to be more prevalent in North Africa and Middle East, including Afghanistan, Libya, United Arab Emirates, Lebanon, Qatar and Iran. A world drug report from the United Nations Office on Drugs and Crime (UNODC) supported and explained these findings, which showed that the illicit opioid (heroin and opium) produced in Afghanistan accounted for an estimated 80% of the world's total supply and most of the opium and illicit morphine seized in 2013 were concentrated around poppy cultivation areas in Afghanistan and its neighbouring countries (UNODC, 2014a; UNODC, 2015). The incidence of opioid use disorder in high-income North America was second only to that in North Africa and Middle East. And high-income North America was the only one in 21 regions where the ASR was increasing, which was mainly due to the increasing trend in opioid use disorder. The current situation of opioid use disorder in high-income North America might be related to the illicit opioid mainly coming from Afghanistan according to the UNODC report (UNODC, 2014a). For example, according to the Royal Canadian Mounted Police National Intelligence Coordination Center, at least 90% of the heroin seized in Canada between 2009 and 2012 originated from Afghanistan (UNODC, 2014b). This means that education on drug use prevention is immediately required and preventive measures should be implemented to decrease the incidence of opioid use disorder in that region. This could be achieved through specifically designed development measures in the context of sustained national growth and sustainable development efforts that recognise the particular socio-cultural characteristics of the target communities and groups. Applying such measures in the countries producing illicit opioid might reduce the incidence of opioid use disorder not only in those countries but also in other countries (UN, 1998).
In contrast to opioid use disorder, cannabis use disorder was more prevalent in high-SDI regions, including high-income North America, Australasia and Western Europe. The incidence of cannabis use disorder was the second highest after opioid use disorder worldwide, and it was the highest in high-SDI regions such as Australasia and Western Europe. However, the changing trends in the incidence of cannabis use disorder were stable at the global and regional levels. These findings were similar to the UNODC report, which indicated high cannabis use in Western and Central Europe, Oceania and North America (UNODC, 2015). Our research shows that the drug use disorders exhibited by teenagers involve cannabis more than opioid. In view of the result and the potential harm of cannabis to teenagers (Gibbs et al., Reference Gibbs, Winsper, Marwaha, Gilbert, Broome and Singh2015; Camchong et al., Reference Camchong, Lim and Kumra2017; Scott et al., Reference Scott, Rosen, Moore, Roalf, Satterthwaite, Calkins, Ruparel, Gur and Gur2019), effective preventive measures should be implemented for juvenile cannabis use. Studies have shown that preschool development programs can reduce the rate of cannabis use in teenagers (Campbell et al., Reference Campbell, Ramey, Pungello, Sparling and Miller-Johnson2002; O'Brien et al. Reference O'Brien, Charney, Lewis, Cornish, Post, Woody, Zubieta, Anthony, Blaine, Bowden, Calabrese, Carroll, Kosten, Rounsaville, Childress, Oslin, Pettinati, Davis, Demartino, Drake, Fleming, Fricks, Glassman, Levin, Nunes, Johnson, Jordan, Kessler, Laden, Regier, Renner, Ries, Sklar-Blake and Weisner2004).
The literature on sex differences published over the past three decades has shown that women typically begin to use substances later than men and that women overall may be less likely than men to develop drug use disorders (Brady and Randall, Reference Brady and Randall1999). For example, men in the United States were reported to be 2.33 and 2.25 times more likely to have had drug use disorders and drug dependence, respectively, than women during the previous year (Compton et al. Reference Compton, Thomas, Stinson and Grant2007; Hecksher and Hesse, Reference Hecksher and Hesse2009). This is similar to our finding that drug use disorders were more common among men than women in most age groups. In addition, our study found that the incidence rate of drug use disorders peaked among teenagers aged 15–19 years and tended to decrease with age in both men and women. These findings may be helpful when formulating specific policies for preventing or decreasing the incidence of drug use disorders.
Limitations
Our study was based on the GBD 2017 data. Although the limitations of the GBD approach have been reported previously (GBD 2016 Disease and Injury Incidence and Prevalence Collaborators, 2017; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018), several major limitations related to our study should be noted here. First, although this study modelled results where data were not available, the gaps in data for many countries resulted in uncertainty around the modelled estimates, which can only be reduced by obtaining improved epidemiological evidence. Secondly, four drug use disorders (opioid, cocaine, cannabis and amphetamine) were defined according to DSM-IV-TR and ICD-10 diagnostic criteria. There are some differences between the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and DSM-IV-TR, and so estimates of drug use disorder burden might change if DSM-5 was used. Thirdly, in addition to the four analysed drug use disorders (opioid, cocaine, cannabis and amphetamine), other drug use disorders include hallucinogen dependence, inhalant or solvent dependence, sedative dependence, tranquilliser dependence and dependence on other medicines, drugs and substances. Because data on the other drug use disorders were obtained from the Australian National Survey of Mental Health and Wellbeing and the United States National Epidemiological Survey on Alcohol and Related Conditions, the GBD study could not estimate their incidence. However, according to previous studies, the other drug use disorders are far less prevalent than the four-drug use disorders that we analysed (GBD 2016 Alcohol and Drug Use Collaborators, 2018).
Conclusions
The incident cases of drug use disorders are increasing from 1990 to 2017. Although the trend of the incidence rate is stable, it remains high and in particular, there is an increasing trend in high-income North America. These observations suggest that current preventive measures and policies for drug use disorders have not been fully effective. Our results also suggest that opioid is major contribution to the incidence of drug use disorders and that they tend to be more common in men, teenagers and regions with a high SDI. The information obtained by this study illustrates the global disease burden of drug use disorders and should help in the establishment of more effective and targeted prevention strategies for drug use disorders.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796020000657.
Data
As described in the methods, the raw data for this study were from the GBD online data source tool, which is located at http://ghdx.healthdata.org/gbd-results-tool.
Acknowledgements
The authors would like to thank the Institute for Health Metrics and Evaluation for the data of the GBD database.
Financial support
This study was supported by the National Social Science Foundation of China (No. 16BGL183) and the Natural Science Basic Research Program of Shaanxi (No. 2020JQ-929).
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical standards
This study was performed in accordance with the Declaration of Helsinki and was approved by the institutional review board of the First Affiliated Hospital of Xi'an Jiaotong University. For this study, the data came from the Global Burden of Disease 2017 database, so consent was not required.