INTRODUCTION
Sustained monomorphic ventricular tachycardia (VT) can result in hypoperfusion or devolve into more dangerous rhythms such as ventricular fibrillation (VF). In patients with unstable VT, indicated by the presence of shock, syncope, heart failure, or myocardial ischemia, the American Heart Association (AHA) recommends synchronized electrical cardioversion.Reference Zipes, Camm and Borggrefe 1 , Reference Neumar, Otto and Link 2 Standard biphasic waveform energy doses are up to 200 J; however, the AHA notes no evidence of harm up to 360 J.Reference Link, Atkins and Passman 3 If repeated attempts at electrical cardioversion with high energies are unsuccessful, the next recommendation is to administer a parenteral antiarrhythmic, such as amiodarone. However, antiarrhythmics often require more than 20 minutes to achieve VT termination, are frequently unsuccessful, carry risks of side effects, such as hypotension, and can even be pro-arrhythmogenic.Reference Soar, Nolan and Bottiger 4 - Reference Barnes and Hollands 6 Two retrospective cohort studies of patients with stable sustained VT revealed that 10.6% and 17% of patients developed hypotension during treatment,Reference Marill, deSouza and Nishijima 7 , Reference Tomlinson, Cherian, Betts and Bashir 8 findings that are consistent with a study of unstable VT.Reference Scheinman, Levine and Cannom 9 In patients with unstable VT refractory to repeated shocks at standard doses, guidelines do not currently identify a rapid-acting low-risk therapy. Double sequential cardioversion, performed by delivering two shocks through two sets of pads as closely timed as possible, has been described for the management of patients with refractory atrial fibrillation (AF)Reference Bjerregaard, El-Shafei and Janosik 10 - Reference Kabukcu, Demircioglu and Yanik 13 and VF.Reference Leacock 14 - Reference Merlin, Tagore, Bauter and Arshad 18 Here we describe the successful use of double sequential synchronized cardioversion (DSSC) in a patient with unstable VT refractory to standard electrical cardioversion methods.
CASE REPORT
A 79-year-old man was brought to the emergency department (ED) by ambulance after complaining of presyncope, shortness of breath, and nausea for 4 hours. His past medical history included hypertension and dyslipidemia, but no prior cardiac disease. He was tachycardic at 180 beats per minute (bpm) and hypotensive with a blood pressure that was undetectable with an automated blood pressure monitor. His rhythm strip showed a wide complex tachycardia. Cardioversion was attempted twice by paramedics en route to the ED, each with 200 J on a biphasic defibrillator and anterolateral (AL) pad placement, yet this was unsuccessful. On arrival to the ED, he continued to have a heart rate of 180 bpm, and his systolic pressure was estimated to be 60 mm Hg by palpation of the radial artery using a manual blood pressure cuff. An oxygen saturation could not be obtained given his low blood pressure and rapid heart rate. He was mentating, appeared drowsy, and had a Glasgow Coma Scale (GCS) score of 13. His weight was estimated to be approximately 90 kg. His electrocardiogram (ECG) in the ED demonstrated monomorphic VT (Figure 1).
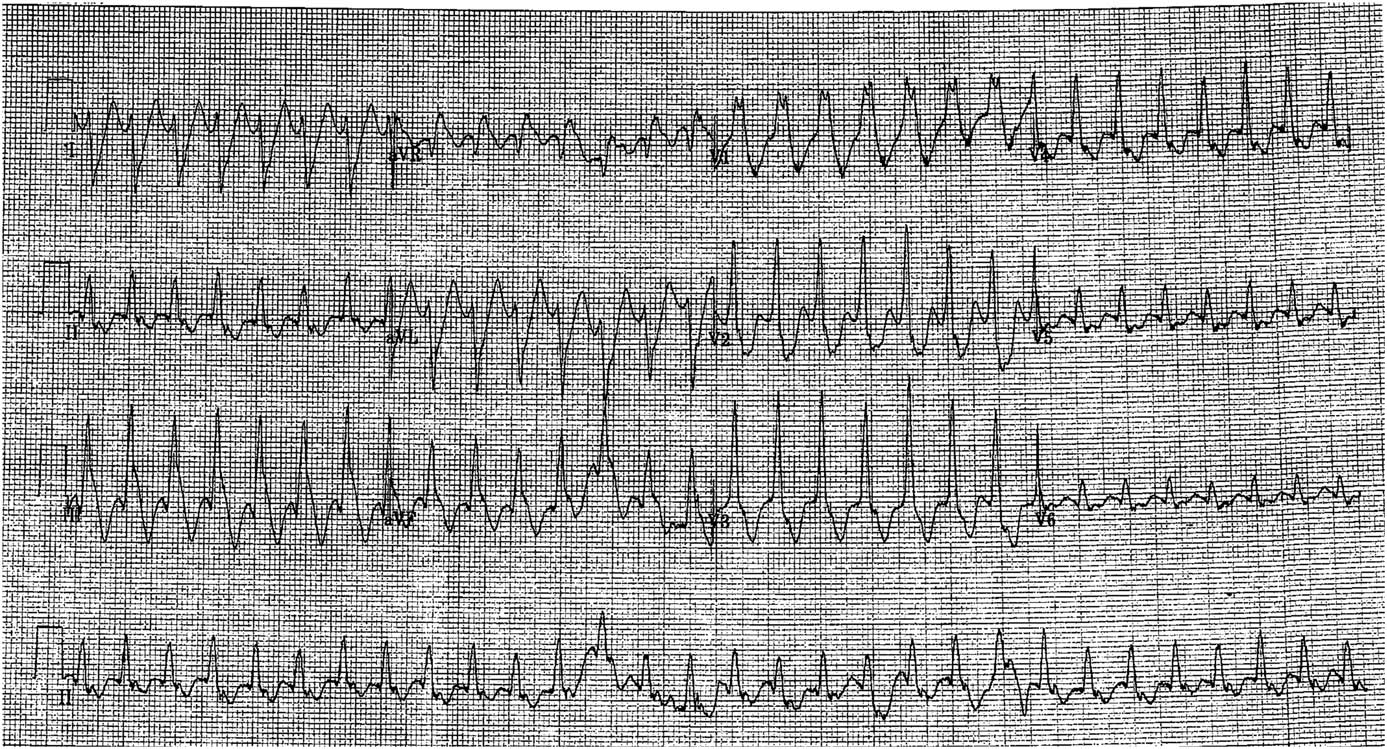
Figure 1 Initial ECG: monomorphic ventricular tachycardia.
The defibrillator pads were replaced; two new pads were placed AL and two additional pads were placed anteroposterior (AP) (Figure 2). Each set of pads was connected to a separate biphasic defibrillator (Philips HeartStart MRx). He received oxygen by a non-rebreather mask and was given phenylephrine (200 mcg) and propofol (30 mg) for hypotension and sedation, respectively. Because the paramedics had attempted cardioversion through the AL pad placement, a single shock at 200 J was delivered through the AP pads. There was no change in rhythm. After 30 seconds, two closely timed synchronized 200 J shocks were delivered through AP and AL pads attached to two separate defibrillators by two operators coordinating by verbal count. The patient converted to sinus rhythm (Figure 3) with a heart rate of 85 and a blood pressure of 140/65. A post-cardioversion ECG confirmed sinus rhythm. He was started on an amiodarone infusion and admitted to the cardiology service. After 10 minutes, his mental status returned to his baseline, and his GCS score was 15. Erythema of the skin over the AL pad areas was noted, which did not require further treatment.
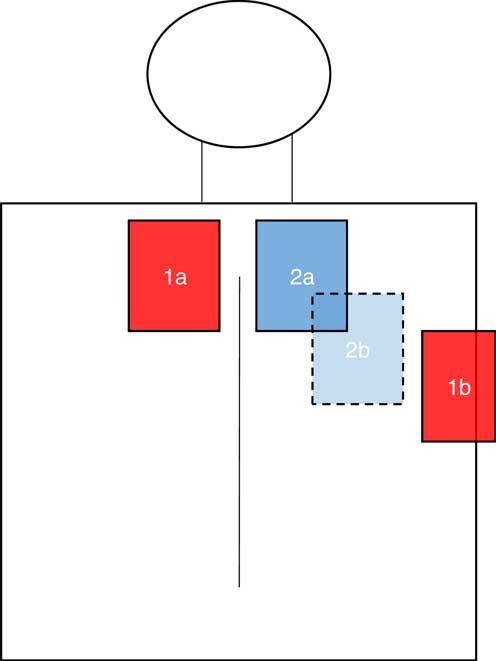
Figure 2 Schematic showing pad placement for double sequential synchronized cardioversion. Pad 1a placed inferior to the right clavicle and to the right of the sternum. Pad 1b placed lateral to the normal cardiac apex in the anterior or mid-axillary line (V5-6 area). Pad 2a placed inferior to the left clavicle and to the left of the sternum. Pad 2b is placed posteriorly, to the left of the patient’s spine.
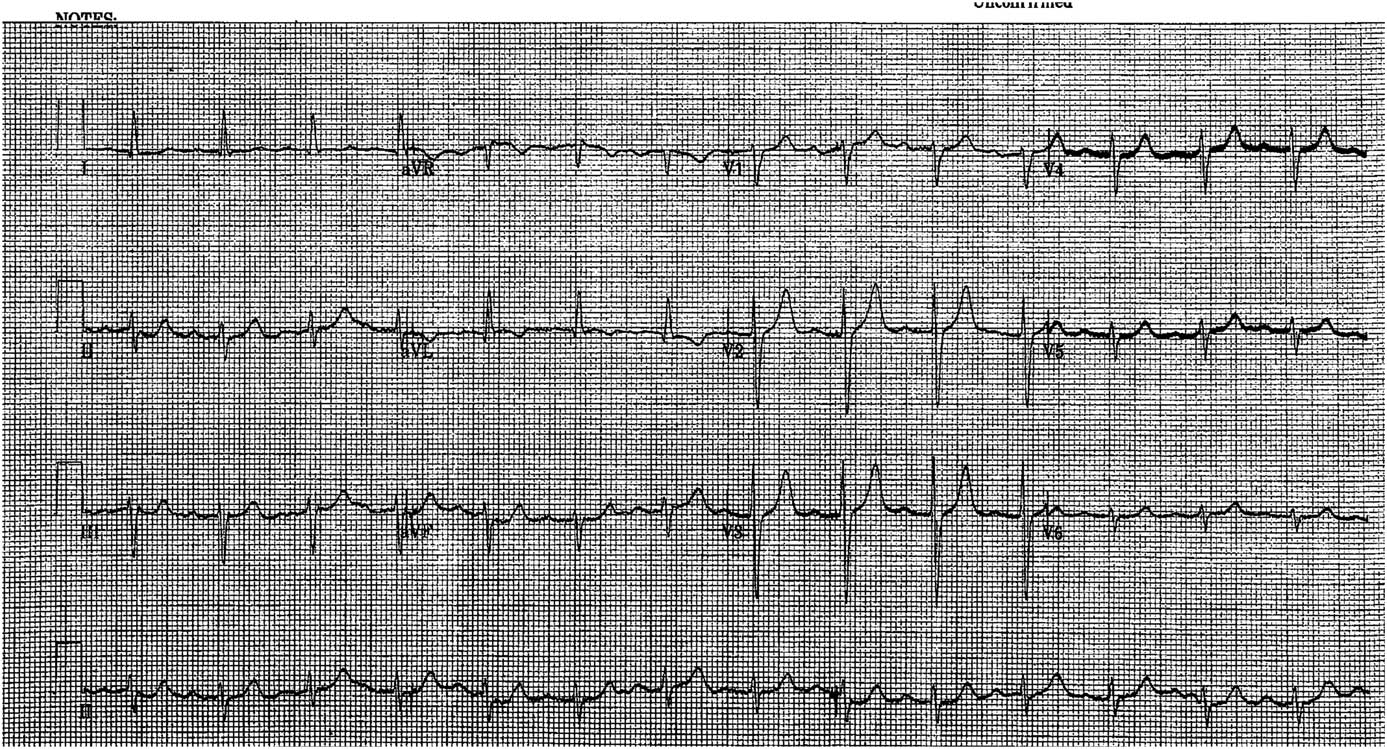
Figure 3 Post cardioversion ECG: sinus rhythm
The patient’s initial troponin level, drawn prior to cardioversion attempts in the ED, was 1300 ng/L and peaked at 2416 ng/L (normal<26 ng/L). A stress echocardiogram revealed Grade 1 hypokinesis, and an angiogram revealed critical stenosis in the mid to distal circumflex artery. The cardiology service believed that a myocardial infarction was the underlying etiology of the VT. He underwent percutaneous coronary intervention and a stent placement. A cardiac magnetic resonance imaging (MRI) confirmed a circumflex territory infarct. He had a VT stimulation test during his admission, which resulted in recurrent unstable VT, and the decision was made to place an automatic implantable cardioverter-defibrillator.
DISCUSSION
We present a case of a patient with unstable monomorphic VT, refractory to multiple attempts at synchronized electrical cardioversion with single shocks, who was successfully cardioverted using double sequential 200 J synchronized shocks.
The current AHA guidelines do not specifically define when VT is considered refractory to electrical cardioversion.Reference Zipes, Camm and Borggrefe 1 This will be an important step going forward to reduce variation in clinical practice. In our patient’s case, we considered him refractory after the delivery of three shocks, one of which involved a change in vector.
AHA guidelines recommend antiarrhythmic treatment with amiodarone in patients with monomorphic VT for which electrical cardioversion has been unsuccessful. Amiodarone is not a benign medication. Hypotension with intravenous administration is estimated to occur in 26% of patients.Reference Scheinman, Levine and Cannom 9 A retrospective case series found that out of 28 patients with stable VT who were given amiodarone, only 8 (29%) had a termination of VT. Of concern, two patients became unstable with hypotension or presyncope, thereby necessitating electrical cardioversion.Reference Marill, deSouza and Nishijima 19 Other side effects with amiodarone are rare, but pro-arrhythmic effects have been described, including precipitating VF and torsades de pointes.Reference Scheinman, Levine and Cannom 9
First described in 1993, dual sequential defibrillation has been used as a last resort for cases of VF and pulseless VT, refractory to multiple shocks and medications, including epinephrine and antiarrhythmics.Reference Leacock 14 - Reference Gerstein, Shah and Jorgensen 16 In these case reports, two 200-J (biphasic models) or two 360-J (monophasic models) doses of electricity have resulted in a return to a perfusing rhythm.Reference Leacock 14 - Reference Gerstein, Shah and Jorgensen 16
In patients with a pulse, DSSC has been used with success in patients with AF. One case series found that 13 of 15 patients with AF refractory to standard cardioversion converted with DSSC. In this series, there were no reported adverse events related to electrical cardioversion, including hypotension, heart failure, atrioventricular block, and stroke. No patients had an elevation of their creatine kinase (CK-MB) post-cardioversion.Reference Kabukcu, Demircioglu and Yanik 13 In a second case series of 21 patients with AF, not responding to two standard shocks, 19 of 21 converted with no adverse events related to electrical cardioversion and no elevation of troponin T.Reference Velázquez, Martínez and Cancino 20 In the largest case series reported, DSSC with two monophasic shocks at 360 J each converted 67% (66 of 99 patients) of patients with persistent AF after the first double shock, with an additional 14 patients converting after a second double shock. Only 3 patients reported minor skin erythema at the site of pad placement, and 16 patients had transient sinus bradycardia with no intervention required. No thromboembolic, serious hypotension, or congestive heart failure events were reported.Reference Alaeddini, Feng and Feghali 12 To our knowledge, there have been no studies on the use of DSSC in VT patients with a pulse.
The exact mechanism behind the effectiveness of double sequential cardioversion and defibrillation is unknown, but multiple mechanisms have been proposed. These include multiple vectors of electricity resulting in a greater amount of myocardium depolarizing, increasing the duration of cardioversion because there will not be precise synchronization of the shocks, and a higher total dose of energy, especially in the context of patients with larger body habitus.Reference Leacock 14 - Reference Gerstein, Shah and Jorgensen 16
In our patient’s case, he presented with significant hypotension and mental status changes. DSSC resulted in a rapid resolution of his VT and hypotension, which was unlikely to resolve as quickly with an amiodarone infusion. His cardiac enzymes were elevated after cardioversion; however, we believe that this is due to an underlying ischemic event that triggered the VT and not the cardioversion itself.
Prior to trying novel cardioversion methods, the practitioner should ensure that standard techniques have been optimized.Reference Soar, Nolan and Bottiger 4 , Reference Ramirez, Fiset and Cleland 21 , Reference Sado and Deakin 22 Moreover, devices may not be designed or tested to withstand DSSC, and damage has been reported to occur.Reference Gerstein, McLean, Stecker and Schulman 23
CONCLUSION
We describe a case of successful cardioversion by DSSC in a patient with an unstable VT with a pulse that was refractory to repeated single shocks. Although further research is needed to assess the safety of double sequential cardioversion, consideration may be given to using this method in patients with unstable VT when single shocks using optimal techniques are ineffective. Demonstrated safety and effectiveness of this technique could reduce the need for a bolus infusion of medications, such as amiodarone, that may worsen hypotension in already unstable patients.
Competing interests: None declared.





