CVD and cancer represent major causes of mortality in high-income countries( Reference Lozano, Naghavi and Foreman 1 ). In the USA, it was estimated that CVD and cancer combined account for more than 50 % of the overall mortality burden among adults and represent the first and second cause of mortality, respectively( Reference Kenneth, Kochanek and Jiaquan 2 ). It is widely acknowledged that, among others, unhealthy diet and poor lifestyle represent major preventable risk factors for all-cause and cardiovascular mortality in the USA, with unhealthy diet and intake of specific dietary fat in particular, representing a considerable part of the risk( Reference Danaei, Ding and Mozaffarian 3 ). Notably, in 2010 it was estimated that saturated and trans-unsaturated fat consumption was higher in the USA (11·8 and 2·8 % of the overall energy intake, respectively) when compared with global consumption (9·4 and 1·4 % of the overall energy intake, respectively). On the other hand, consumption of poly-unsaturated fat consumption was comparable between the USA and all of the other countries combined, representing about 5·9 % of the overall energy intake( Reference Micha, Khatibzadeh and Shi 4 ).
Population-based studies showed that high intake of poly-unsaturated fat is associated with reduced cardiovascular risk and related mortality( Reference Abdelhamid, Martin and Bridges 5 , Reference Yamagishi, Iso and Date 6 ). In contrast, the relationship between saturated fat intake and CVD incidence and mortality remains a controversial topic. Previous systematic reviews and meta-analyses reported no significant association between saturated fat intake and increased risk of CVD or mortality( Reference Chowdhury, Warnakula and Kunutsor 7 – Reference Siri-Tarino, Sun and Hu 9 ). Recent evidence from large prospective US cohorts, however, consistently showed that replacement of dietary saturated fat with monounsaturated and polyunsaturated fat is associated with a lower risk of CVD, as well as all-cause and cause-specific mortality( Reference Li, Hruby and Bernstein 10 , Reference Wang, Li and Chiuve 11 ). In contrast, when replacing dietary saturated fat with refined carbohydrates, saturated fat intake was not associated with CVD incidence, which highlights the importance of studying this relationship in the context of the replacement macronutrient( Reference Li, Hruby and Bernstein 10 ). Moreover, scientific evidence showing the relation between dietary fat intake and cancer risk is currently accumulating. In a recent meta-analysis of observational studies, significantly increased risk of gastric cancer was associated with higher dietary intakes of saturated fat, whereas a reduced risk of gastric cancer was observed for those subjects having a higher intake of unsaturated fat( Reference Han, Jiang and Liu 12 ).
It is admissible to suppose that adopting a healthy diet followed by increased consumption of mono- and poly-unsaturated fat or the replacement of saturated fat with unsaturated fat may lead to beneficial outcomes in terms of overall, cardiovascular and cancer mortality at the population level. Recently, US guidelines recommended reducing saturated fat intake to <10 % of the total energy intake. On the other side, no recommendation to improve mono- and polyunsaturated fat intake was stated( Reference Sacks, Lichtenstein and Wu 13 ).
The aim of the present study was to estimate the association between an increase in mono- and polyunsaturated fat intake or the substitution of saturated fat to mono- and poly-unsaturated fat and mortality reduction in US adults. For this purpose, an energy partition model and an iso-energetic substitution analysis were conducted over a prospective study resulting from the American National Health and Nutrition Examination Survey (NHANES) linked to the US national death registry.
Methods
Participant selection
The NHANES is an epidemiological cross-sectional study aimed to generate a representative sample of the civilian non-institutionalised US adults using a multi-stage probability sampling design( 14 ). The NHANES study started in 1999 and every year about 5000 US citizens are involved providing data regarding their socio-economical characteristics, dietary habits, medical status and medical history. On a regular basis, the NHANES participants are linked to the US death registry using a probabilistic record linkage defining a prospective mortality study. The last linkage to the US mortality registry was in 2011( 15 ).
The number of all participants from the survey conducted between 1999 and 2011 was 62 210, of whom 21 290 were excluded because of no available data on mortality or age under 18 years, leaving 40 870 participants. After exclusion of subjects aged between 18 and 30 years, 30 509 subjects were retained. Exclusion of prevalent cases of cancer, diabetes and CVD reduced the sample to 21 344 participants. Finally, the exclusion of subjects with missing information on fat intake and adjusting covariates used in the models led to a final sample size of 18 372 individuals, resulting in a cumulative observational time of 116 398 person-years with a median observational time of 6·1 years. During the follow-up, 1118 deaths for all causes, 267 deaths for cardiovascular cause and 289 deaths due to cancer were observed. The flow chart of participant selection was reported on Fig. 1.
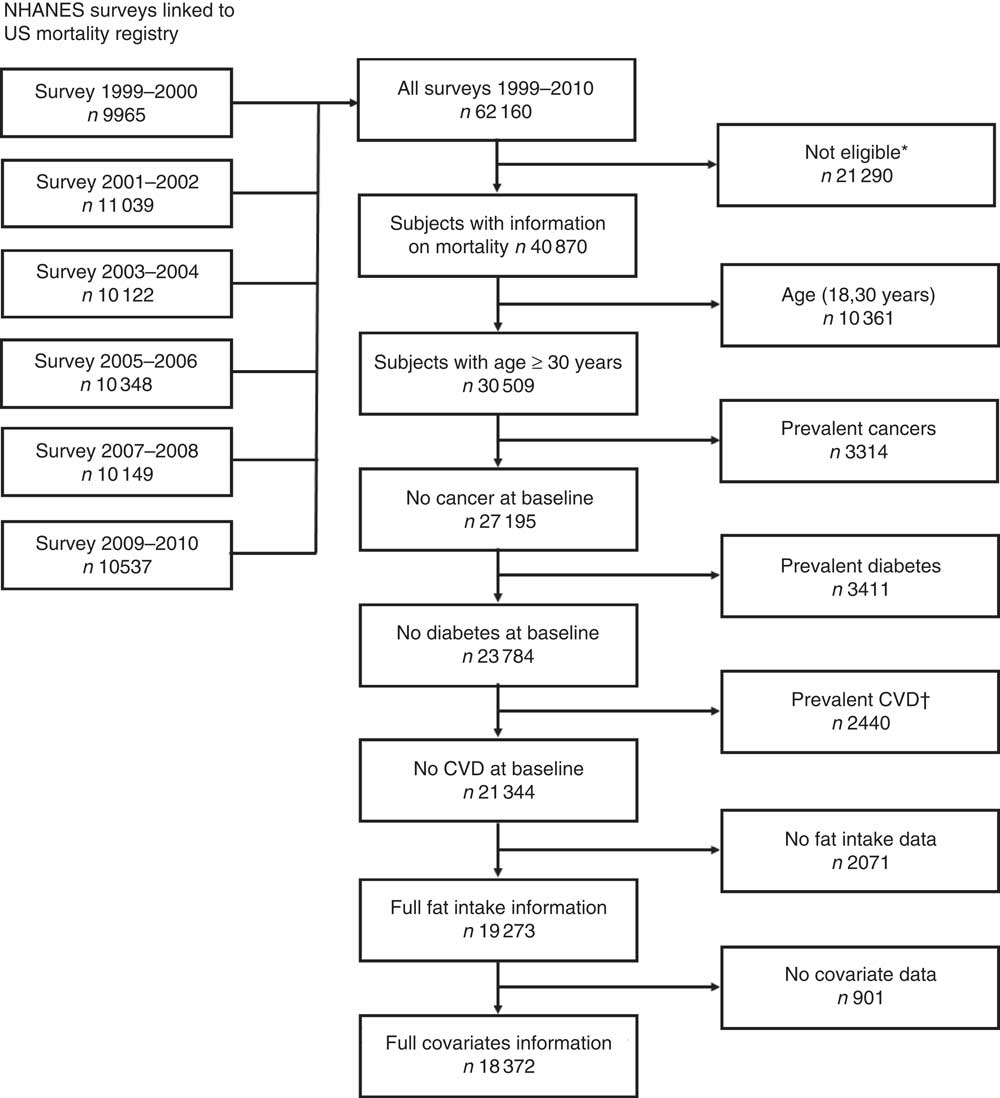
Fig. 1 Flow chart of participants selected from National Health and Nutrition Examination Survey (NHANES) surveys conducted between 1999 and 2010. * Subjects without mortality data or aged under 18 years old. † Subjects having at least one of the following: congestive heart failure, CHD, angina pectoris, heart attack and stroke.
Dietary assessment
A dietary interview assessing detailed dietary intake information was performed to estimate types and amounts of foods and beverages consumed and to calculate total energy intake. The dietary interview was composed of three sections – 24-h dietary recall, evaluation of nutritional supplements and dietary post recall – and was administered to all NHANES participants. To allow for better estimates of usual nutrient intakes, 2 d of dietary data were collected for the survey performed after 2002. The dietary post recall was conducted by telephone interview after approximately 3–10 d from the first dietary evaluation( 16 ).
Statistical analysis
The description of the sample was performed separately for subjects who died during the observational time and for those subjects who survived up to the end of the observational time. Medians and interquartile ranges were reported for continuous variables and percentages were reported for categorical variables (Table 1).
Table 1 Baseline characteristics of the 18 372 participants from the National Health and Nutrition Examination Survey study (Medians and 1st, 3rd quartiles; percentages)
SBP, systolic blood pressure; DBP, diastolic blood pressure; MFA, monounsaturated fat; PFA, polyunsaturated fat.
All analyses were based on multivariable adjusted Cox proportional hazard model having age as an underlying time variable and stratified by sex and 5-year age classes. Raw and multivariable adjusted models considering potential confounders were evaluated in a sequential modelling approach aimed to evaluate the residual confounding bias (results not shown). After the evaluation of the results from sequential modelling, a multivariate model adjusted for ethnicity (Black, White and others), BMI (continuous), alcohol intake (continuous), smoking status (more than 100 cigarettes/life), education (university degree), sedentariness (subjects who declared having more than 8 h/d of sedentary activity or who do not declared moderate or vigorous physical activity), dietary fibre intake (continuous) and blood pressure (systolic and diastolic blood pressure as continuous data) was chosen to report all of the results. The proportional hazard assumption was evaluated by Schoenfeld’s residuals. Sensitivity analyses were conducted excluding death cases assessed in the first 18 months after recruitment. Results from the analyses evaluating the association between tertiles of energy density of saturated, monounsaturated and polyunsaturated fat with all-cause and specific-cause mortality were reported along with trend tests performed considering 1 sd increase (Table 2). The associations between changes of fat intake and all-cause and specific-cause mortality were performed considering the energy partition and nutrient density paradigms as previously described by Hu et al.( Reference Hu, Stampfer and Rimm 17 ). In brief, in the energy partition model, the total energy from the nutrients is partitioned in the different components contributing to the energy intake, so that nutrients are coded in a metric of their energy contribution. In this model, the relative risk estimate corresponds to a given increase of energy from that specific component when all of the other components remain constant. The analyses based on the energy partition models were performed considering all of the dietary components (carbohydrates, proteins and fat) and the fat components only. On the other hand, the nutrient density model is a substitution model in which the ratio between the energy from the single dietary component and the overall energy from all dietary components are considered in the model so that the sum of all the components remains constant and corresponds to a given numerical value (100 % if the percentage is used). This model is performed considering the energy from fat components contributing to energy intake excluding one, so that the relative risk estimate for a given component represents the substitution of a given quantity (1 % when the percentage is used) of the excluded component with this one. In the present work, the substitution model was performed considering a 10 % substitution of the energy from fat consumption only. The reported risk then was related to 10 % substitution of fat only derived energy, excluding carbohydrates and proteins. Energy partition and substitution analysis were reported in Table 3.
Table 2 Associations between tertiles of total energy percentage from intake of specific fat and all-cause, cardiovascular and cancer mortality (Hazard ratios (HR) and 95 % confidence intervals)
Ref., referent values.
* Models are adjusted for ethnicity, BMI, alcohol intake, smoking status, education, sedentariness, fibre intake and blood pressure.
Table 3 Partition and substitution models for the association between dietary fat intake and all-cause, cardiovascular and cancer mortality (Hazard ratios (HR) and 95 % confidence intervals)
* Partition model1: energy partition model considering dietary fat, carbohydrates and proteins, risks for 418·4 kJ (100 kcal) increase of dietary fat maintaining constant all of the other components. Partition model2: energy partition model considering only dietary fat, risks for 418·4 kJ (100 kcal) increase of dietary fat maintaining constant all of the other components. Substitution model1: substitution of 10 % of energy from total fat intake derived from saturated fat. Substitution model2: substitution of 10 % of energy from total fat intake derived from monounsaturated fat. Substitution model3: substitution of 10 % of energy from total fat intake derived from dietary polyunsaturated fat.
All statistical analyses were performed taking into account the multi-stage probability sampling design of the NHANES study using the weights from the multi-stage probability sampling to avoid the effect of differential probabilities of selection among subgroups, and to compensate for exclusion of sampling areas in the sampling frame. The surveymean and the surveyfreq procedures of the SAS software were used to describe the sample, whereas the Cox models were fitted using the proc surveyphreg of the SAS software. Statistical analyses were performed using SAS package version 9.4 and type-I error (α) was set to 0·05 (5 %).
Results
Participants who survived at the end of the observational time were younger, mostly women, prevalently non-smokers, with lower systolic blood pressure and had higher intake of dietary fibre and overall energy when compared with participants who had died before the end of the observational time. Adiposity in terms of BMI and percentages of energy from fat, carbohydrates and protein intakes were comparable among those participants who survived at the end of the observational time and those who died. The analysis of the relation between fat intake and all-cause and specific-cause mortality showed that higher intakes of saturated fat resulted in an increased risk of mortality, whereas higher intakes of polyunsaturated fat resulted in a decreased risk of mortality. In particular, comparing the first tertile (7·1 %) with the third tertile (14·5 %) of energy percentage from saturated fat resulted in a significant 12 % increased risk for all-cause, cardiovascular and cancer mortality (hazard ratio (HR) 1·12; 95 % CI 1·07, 1·18; HR 1·12; 95 % CI 1·06, 1·17 and HR 1·12; 95 % CI 1·06, 1·17 for all-cause and cancer mortality, respectively). On the other hand, when comparing the first tertile (4·4 %) with the third tertile (10·2 %) of energy percentage from polyunsaturated fat, a significant reduction of all causes and specific cause risk of death up to 7 % was observed (HR 0·94; 95 % CI 0·90, 0·98; HR 0·93; 95 % CI 0·89, 0·97 and HR 0·93; 95 % CI 0·89, 0·97 for all-cause, cardiovascular and cancer mortality, respectively). Notably, the association between monounsaturated fat intake and mortality was not significant.
Partition models reported about the associations between a given increase in fat intake and mortality risk when maintaining constant the other sources of energy. According to these analyses, it was observed that an increase of 418·4 kJ/d (100 kcal/d) in any of the fats did not correspond to a significant change of the mortality risk when energy intake from other fats, carbohydrates and proteins remained constant. On the contrary, when the analysis is performed maintaining constant the energy from fat sources only, a 418·4 kJ/d (100 kcal/d) increase in saturated fat intake resulted in a 9 % significantly increased risk for all-cause, cardiovascular and cancer mortality. On the other hand, a 418·4 kJ/d (100 kcal/d) increase in polyunsaturated fat intake corresponded to a 2–3 % significant reduction in risk for all-cause and cardiovascular mortality when energy intake from other fat remains constant. Again, monounsaturated fat intake was not significantly related to the risk of death.
The iso-energetic substitution analysis applied to energy intake from fat only revealed that the substitution of 10 % of energy derived from saturated fat with an equal amount of energy from polyunsaturated fat resulted in an 8 % significant reduction in all-cause mortality risks. Substitution of saturated fat with monounsaturated fat resulted in a 3 % borderline significant risk reduction for all-cause mortality. A 4 % decreased risk in all-cause mortality was observed in the substitution model considering the substitution of 10 % of energy (from fat) derived from saturated fat with an equal amount of energy from mono-unsaturated fat. Finally, an iso-energetic substitution of 10 % of energy derived from monounsaturated fat with an equal amount of energy from polyunsaturated fat resulted in a significant decrease in all-cause and specific-cause mortality by 4 to 5 %. Results considering all-cause mortality were confirmed also for cause-specific mortality where 8 % cardiovascular and cancer death risk reduction was reported for the substitution of saturated fat with an equal amount of polyunsaturated fat. An evocative, but not statistically significant (P=0·0621 and P=0·0548 for cardiovascular and cancer death risk, respectively), 3 % cardiovascular and cancer death risk reduction was reported for the substitution of 10 % of energy from saturated fat with an equal amount of monounsaturated fat. The above results are maintained when excluding subjects who died in the first 18 months after recruitment (results not shown).
Discussion
In this observational prospective mortality study in US adults, higher saturated fat intake was associated with increased risk for all-cause mortality, CVD and cancer mortality. On the other hand, a reduction of all-cause and specific-cause mortality risk was observed for those participants having a higher intake of polyunsaturated fat compared with those having lower intakes of polyunsaturated fat. The present study confirmed evidence from randomised control trials on the beneficial effect of polyunsaturated fat intake on cardiovascular function( Reference Mozaffarian, Micha and Wallace 18 ). In addition, the present work reported about the beneficial outcomes deriving from mono- and polyunsaturated fat substituting saturated fat in terms of mortality at a population level. In summary, the present findings point out a beneficial association between a diet rich in monounsaturated and specifically polyunsaturated fat and low in saturated fat; these findings are confirmed by previous studies( Reference Abdelhamid, Martin and Bridges 5 , Reference Mozaffarian, Micha and Wallace 18 , Reference Hooper, Martin and Abdelhamid 19 ). Notably, the present study extended this evidence to cancer mortality to a complementary extent.
In the present study, a significant relation between monounsaturated fat intake and mortality risk was not found differently from previous studies( Reference Wang, Li and Chiuve 11 ). On the other hand, the present study showed that a substitution of 10 % of energy from saturated fat with an equal amount of energy from mono-unsaturated fat resulted in a borderline reduction of mortality risk. This result points out the suggestive idea that substitution of saturated fat with monounsaturated fat, more than an increase of monounsaturated fat intake per se, might be associated with a beneficial outcome in terms of mortality risk( Reference Kris-Etherton 20 ). According to our results regarding partition models, an increase of unsaturated fat and a decrease of saturated fat intake have beneficial effects only when maintaining constant the energy from other fat sources excluding carbohydrates and proteins. The finding from the present study implies that substitution of saturated fat with polyunsaturated fat is possibly related to even stronger beneficial association with the mortality outcomes that were investigated. As a confirmation of the previous conjecture in the present study, the iso-energetic substitution of saturated fat with unsaturated fat was associated with a significantly reduced risk for all-cause and cause-specific mortality. This evidence was suggested indirectly from previous studies evaluating the relation between fat intake and cardiovascular and overall mortality( Reference Mozaffarian, Micha and Wallace 18 , Reference de Oliveira Otto, Mozaffarian and Kromhout 21 ). Again, for the first time to our knowledge the present work extends the evidence of a beneficial effect of the substitution of saturated fat intake with mono- and polyunsaturated fat on cancer mortality. This further emphasises the importance of the type of dietary fat in all-cause and cause-specific mortality. Results from the present study are comparable with those from other studies in which substitution analysis was used to evaluate mortality risk reduction in the USA. In particular, the present study confirms previous findings regarding fat substitution analysis performed in the Nurses’ Health Study where it appeared that saturated to polyunsaturated fat substitution in diet reduces mortality( Reference Wang, Li and Chiuve 11 ). In the present study, it was also confirmed that saturated to poly-unsaturated fat substitution and not saturated fat substitution with other sources of energy, such as carbohydrates, effectively results in beneficial outcomes in terms of mortality. Finally, it must be noticed that no relevant differences in terms of adiposity were observed when looking at survivors and participants who experience death before the end of the observational time. On the other hand, it should be noticed that survivors were younger, healthier and mostly women, whereas participants who died were older, prevalently smokers and prevalently men. This apparently affected adiposity reducing the mean of the BMI in non-survivors. Scientific evidence accumulated over the past decades already explained the possible mechanisms underlying the association between dietary fat intake and cardiovascular outcomes. An early identified mechanism is the mediation between plasma cholesterol level and dietary saturated fat intake. A recent meta-analysis conducted in humans and considering the association between dietary saturated fat intake with main cardiovascular outcomes and mortality reinforced this evidence by means of meta-regressions and subgroup analysis( Reference Hooper, Martin and Abdelhamid 19 ). Among the other factors related to the relation between saturated fat and cardiovascular outcomes, adiposity certainly plays a crucial role( Reference Van Gaal, Mertens and De Block 22 ). Obesity and overweight are conditions normally correlated to high energy intake and sedentariness. Obese and overweight subjects normally also have suboptimal diet and high intakes of saturated fat( Reference Bray, Paeratakul and Popkin 23 , Reference Bray and Popkin 24 ). Nevertheless, obesity and overweight were associated with circulating cytokines and other inflammatory biomarkers that are related to atherosclerosis and then to main cardiovascular outcomes( Reference Lau, Dhillon and Yan 25 ). Moreover, obesity and overweight were consistently associated with increased risk of different cancers through mechanisms acting by impaired hormonal status and increased type 2 diabetes risk( Reference Calle and Kaaks 26 – Reference McMillan, Sattar and Lean 28 ). It is then admissible to suppose that unhealthy diet and a related high saturated fat intake may play a role in leading to an increased cardiovascular and all-cause mortality risk via adiposity-related mechanisms. Mechanisms about how saturated fat intake may result in an increased cardiovascular risk were widely reported in scientific literature. In particular, saturated fat increases the HDL cholesterol and reduces LDL particles heterogeneity in size increasing their density( Reference Dreon, Fernstrom and Campos 29 ). It was shown that smaller and denser LDL particles are strongly associated with atherosclerosis, CVD and stroke( Reference Krauss 30 , Reference Siri-Tarino, Sun and Hu 31 ).
Biological mechanisms regarding polyunsaturated dietary fat intake in relation to cardiovascular outcomes and adiposity have been proposed. A general beneficial effect of polyunsaturated dietary fat on cardiovascular function may be related to its activity in depressing plasma lipids, inhibition of apo synthesis and inhibition of cyclo-oxygenases and lipoxygenases activity, which, in turn, reduces eicosanoid synthesis decreasing thromboxane and platelets tendency to aggregate( Reference Kinsella, Lokesh and Stone 32 ). On the other hand, there is some evidence suggesting that polyunsaturated dietary fats are beneficial in terms of preventing obesity, overweight and type 2 diabetes risk( Reference Delarue, LeFoll and Corporeau 33 ). Finally, polyunsaturated fat intake may result as beneficial in terms of all-cause and cancer-related mortality also because of their antioxidative activity( Reference Hsieh and Kinsella 34 , Reference Porter 35 ).
The present work has limitations owing to its observational nature that limit the proposed results in terms of causal association. On one hand, it is acknowledged that randomised controlled trials and meta-analysis of interventional studies were conducted to evaluate such diet interventions and the effect of fat components on biomarkers of short-term outcomes( Reference Fattore, Bosetti and Brighenti 36 ). On the other hand, it is clear that these approaches cannot be technically performed when long-term outcomes, such as mortality, are considered in healthy subjects. Moreover, in the past, randomised control trials resulted in inconsistent outcomes as observational time, more than the sample size, is an operational limit( Reference Hooper, Martin and Abdelhamid 19 ). Nevertheless, another possible limitation was that the saturated and polyunsaturated type was not taken into account. This information represents an interesting public health question and will be certainly considered by further studies. Finally, underlying morbid conditions at baseline could have affected the results without any possibility of control. This second limitation and a related possible reversal causation can be excluded as prevalent morbid conditions at baseline were excluded in the main analysis and death in the first 18 months from follow-up was excluded in a sensitivity analysis.
Conclusions
High intake of saturated fat corresponded to an increased risk of mortality in US adults, high intake of polyunsaturated fat resulted in a reduced mortality risk in US adults and high intake of monounsaturated fat did not reduce mortality risk in US adults. Substitution of saturated fat with monounsaturated and polyunsaturated fat led to beneficial mortality reduction at the population level, highlighting the importance of the type of fat in the diet.
Acknowledgements
The authors sincerely thank Mrs Ronel Benson and Mrs Henriette Claaseen for administrative support furnished.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
C. R. conceived the study, conceived and performed the statistical analysis and drafted the manuscript; J. B. supported in the planning of the statistical analysis, participated in the interpretation of the results and supported the drafting of the manuscript. M. Z. supported in the planning of the statistical analysis and participated in the interpretation of the results. H. S. K. supervised manuscript editing and interpretation of the results. C. M. S. supported in the planning of the statistical analysis, participated in the interpretation of the results and supported the drafting of the manuscript. All authors read and agreed with the final version of the manuscript.
The authors declare that there are no conflicts of interest.






