Among patients undergoing percutaneous coronary intervention (PCI), large series have documented the incidence of post-PCI ischemic stroke to be 0.1–0.56%. Although the complication is uncommon, stroke in this subset of patients is associated with increased in-hospital mortality, longer hospital stay, and poorer discharge outcomes.Reference Fuchs, Stabile and Kinnaird1–Reference Alkhouli, Alqahtani, Tarabishy, Sandhu and Rihal3
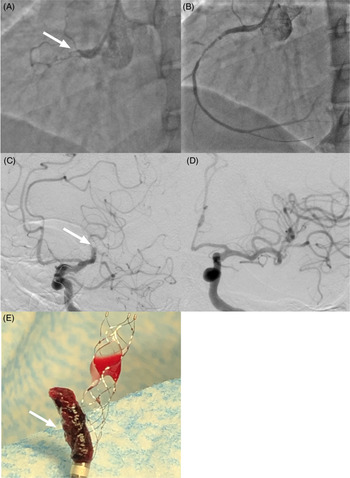
The patient is a 59-year-old male who was previously well until he developed progressive dyspnea over 3 days. He was diagnosed with non-ST elevation myocardial infarction (NSTEMI). He did not have hypertension or diabetes, but had a preexisting diagnosis of Ebstein’s anomaly. He underwent PCI 6 days after symptom onset. The left circumflex artery with a 70% mid-vessel stenosis was stented. The right coronary artery (RCA) was totally occluded proximally by thrombus. After a second balloon dilation (2.0 × 20 mm Sprinter Legend Balloon, Medtronic), the thrombus disappeared (see Figure 1A–B). After stent placement in the RCA, the patient became agitated and subsequently confused. The symptoms were attributed to periprocedural sedation. In recovery, he became dysarthric; consequently, a code stroke was called. He had an NIHSS of 7 (aphasia and dysarthria). He was unable to follow commands and spoke gibberish. The initial plain cranial CT showed an Alberta Stroke Program Early CT Score (ASPECTS) of 6 (left insula, M2, M3, and M6) and an occlusion at the left M1–M2 junction. He underwent successful (TICI 3) thrombectomy with a combined stent retriever (4 × 40 mm Solitaire, Medtronic) and aspiration (ACE 68, Penumbra) approach (see Figure 1C–F). Three months later, he only had moderate expressive aphasia.

Figure 1: Cardioembolic right coronary artery (RCA) clot going to the left middle cerebral artery. (A) Angiography demonstrating a thrombus (white arrow) in the proximal portion of the RCA. (B) After balloon inflation, the thrombus has disappeared. (C) Cerebral catheter angiography demonstrates a thrombus (white arrow) in the M1–M2 junction of the left middle cerebral artery. (D) TICI 3 reperfusion of the left middle cerebral artery after endovascular thrombectomy. (E) Mature clot (white arrow) in the stent retriever and the aspiration catheter.
Risk factors associated with stroke during PCI include the use of an intra-aortic balloon pump, carotid disease, atrial fibrillation, STEMI, previous valvular heart disease, and older age.Reference Fuchs, Stabile and Kinnaird1–Reference Alkhouli, Alqahtani, Tarabishy, Sandhu and Rihal3 Only valvular disease (Ebstein’s anomaly) was present in our patient. Known mechanisms for perioperative stroke during PCI include atheroma dislodgment from the aortic arch, clot forming around catheters, and intraprocedural hypotension causing watershed infarcts.Reference Fuchs, Stabile and Kinnaird1 We believe that the radiographic documentation and temporal progression of symptoms in our case support an intraprocedural embolization from the RCA to the left middle cerebral artery as a very rare mechanism causing our patient’s stroke. There has only been one similar report of such occurrence.Reference Villoth, Muralidharan, Bhaskar Naidu and Senguttuvan4 However, the possibility of a coronary artery embolus causing a stroke was tenuous in this case, with the stroke symptoms occurring 24 h after PCI. There are two potential mechanisms for the retrograde embolization of the thrombus from the coronary artery. Inflation of the undersized pre-dilatation balloon at the distal end of the fusiform mature thrombus may have caused it to jettison retrogradely out of the ostium of the RCA. Alternatively, following balloon inflation, the thrombus may have been dragged out of the coronary artery adhered to the deployed balloon following the pre-dilatation. Following undersized balloon inflation, the totally occluded artery was widely patent with no evidence of in situ thrombus, or distal embolization of thrombus.
Patients with in-hospital stroke were found to have longer onset-to-needle times compared to those with community-onset strokes.Reference Saltman, Silver, Fang, Stamplecoski and Kapral5 The case (symptom-to-groin 155 min) demonstrates that a lower threshold for the activation of a hospital’s code stroke protocol may have led to earlier reperfusion and better subsequent neurologic outcome. The dramatic treatment effect of mechanical thrombectomy for strokes,Reference Goyal, Menon and van Zwam6 emphasizes the importance of early intervention.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
JDBD, RB, JTT, CPF, MJK, and TRM all made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work and drafting the work or revising it critically for important intellectual content. JDBD, RB, JTT, CPF, MJK, and TRM are all responsible for the final approval of the version to be published. JDBD, RB, JTT, CPF, MJK, and TRM are all in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.